Mitigative E Cacy of the Clinical Dosage Administration of Granulocyte
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Therapeutic Class Overview Colony Stimulating Factors
Therapeutic Class Overview Colony Stimulating Factors Therapeutic Class Overview/Summary: This review will focus on the granulocyte colony stimulating factors (G-CSFs) and granulocyte- macrophage colony stimulating factors (GM-CSFs).1-5 Colony-stimulating factors (CSFs) fall under the naturally occurring glycoprotein cytokines, one of the main groups of immunomodulators.6 In general, these proteins are vital to the proliferation and differentiation of hematopoietic progenitor cells.6-8 The G- CSFs commercially available in the United States include pegfilgrastim (Neulasta®), filgrastim (Neupogen®), filgrastim-sndz (Zarxio®), and tbo-filgrastim (Granix®). While filgrastim-sndz and tbo- filgrastim are the same recombinant human G-CSF as filgrastim, only filgrastim-sndz is considered a biosimilar drug as it was approved through the biosimilar pathway. At the time tbo-filgrastim was approved, a regulatory pathway for biosimilar drugs had not yet been established in the United States and tbo-filgrastim was filed under its own Biologic License Application.9 Only one GM-CSF is currently available, sargramostim (Leukine). These agents are Food and Drug Administration (FDA)-approved for a variety of conditions relating to neutropenia or for the collection of hematopoietic progenitor cells for collection by leukapheresis.1-5 Due to the pathway taken, tbo-filgrastim does not share all of the same indications as filgrastim and these two products are not interchangeable. It is important to note that although filgrastim-sndz is a biosimilar product, and it was approved with all the same indications as filgrastim at the time, filgrastim has since received FDA-approval for an additional indication that filgrastim-sndz does not have, to increase survival in patients with acute exposure to myelosuppressive doses of radiation.1-3A complete list of indications for each agent can be found in Table 1. -

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

Treatment of MDS in 2014 and Beyond Treatment Goals in MDS
5/22/2014 Treatment of MDS in 2014 and Beyond Treatment goals in MDS • Get rid of it May 17, 2014 • If you can’t do that, make life better and longer – Improve blood counts Gail J. Roboz, M.D. – Improve quality of life Director, Leukemia Program – Decrease time to progression/leukemia Associate Professor of Medicine Hematopoietic Growth Factors: Hematopoietic Growth Factors: What are they? What are they? • Erythropoietin (EPO,Procrit®, Epogen®) – red • Synthetic versions of proteins normally • Granulocyte colony stimulating factor (GCSF, made in the body to stimulate growth of red Neupogen®) – white cells, white cells and platelets • Granulocyte-macrophage colony stimulating • Promote growth and differentiation factor (GM-CSF, Leukine®) – white • Thrombopoietin (TPO, romiplostim, Nplate®) – • Inhibitors of apoptosis (cell death) platelets • Darbepoietin (Aranesp®) • Peg-filgrastim (Neulasta®) • Note, these are not FDA-approved for MDS Erythropoietin (epo) in MDS Erythropoietin (epo) in MDS • Anemia is presents in >80% of MDS pts at dx • Often high endogenous epo levels • Transfusions help, but many issues • Many different doses and schedules • Recombinant EPO is FDA-approved for treating • Higher response rates with epo + G-CSF if anemia associated with kidney failure epo ≤500 mU/mL and transfusions <2 • Has been used since about 1990 in MDS U/month • Response rates in about 15-30% of patients • Poor probability of response if epo >500 • Many different studies including >1000 patients mU/mL and transfusions >2 U/month • Part of the NCCN MDS treatment guidelines 1. Casadevall N, et al. Blood. 2004;104:321-327. 2. Hellstrom-Lindberg E. Br J Haematol. 1995;89:67-71. -

Comparison Between Filgrastim and Lenograstim Plus Chemotherapy For
Bone Marrow Transplantation (2010) 45, 277–281 & 2010 Macmillan Publishers Limited All rights reserved 0268-3369/10 $32.00 www.nature.com/bmt ORIGINAL ARTICLE Comparison between filgrastim and lenograstim plus chemotherapy for mobilization of PBPCs R Ria, T Gasparre, G Mangialardi, A Bruno, G Iodice, A Vacca and F Dammacco Department of Biomedical Sciences and Human Oncology, Section of Internal Medicine and Clinical Oncology, University of Bari Medical School, Bari, Italy Recombinant human (rHu) G-CSF has been widely used during transplantation.4 However, the use of G-CSF after to treat neutropenia and mobilize PBPCs for their autologous PBPC transplantation has been queried, as its autologous and allogeneic transplantation. It shortens further reduction in time to a safe neutrophil count5,6 does neutropenia and thus reduces the frequency of neutropenic not always imply fewer significant clinical events, such as fever. We compared the efficiency of glycosylated rHu infections, length of hospitalization, extrahematological and non-glycosylated Hu G-CSF in mobilizing hemato- toxicities or mortality.7,8 Even so, the ASCO guidelines still poietic progenitor cells (HPCs). In total, 86 patients were recommend the use of growth factors after autologous consecutively enrolled for mobilization with CY plus either PBPC transplantation.9 glycosylated or non-glycosylated G-CSF, and under- G-CSF induces the proliferation and differentiation of went leukapheresis. The HPC content of each collection, myeloid precursor cells, and also provides a functional toxicity, days of leukapheresis needed to reach the activity that influences chemotaxis, respiratory burst and minimum HPC target and days to recover WBC (X500 Ag expression of neutrophils. -

Human G-CSF ELISA Kit (ARG80143)
Product datasheet [email protected] ARG80143 Package: 96 wells Human G-CSF ELISA Kit Store at: 4°C Component Cat. No. Component Name Package Temp ARG80143-001 Antibody-coated 8 X 12 strips 4°C. Unused strips microplate should be sealed tightly in the air-tight pouch. ARG80143-002 Standard 3 X 2 ng/vial 4°C (Lyophilized) ARG80143-003 Standard diluent 20 ml 4°C buffer ARG80143-004 Antibody conjugate 400 µl 4°C concentrate ARG80143-005 Antibody diluent 16 ml 4°C buffer ARG80143-006 HRP-Streptavidin 400 µl 4°C (Protect from concentrate light) ARG80143-007 HRP-Streptavidin 16 ml 4°C diluent buffer ARG80143-008 20X Wash buffer 50 ml 4°C ARG80143-009 TMB substrate 12ml 4°C (Protect from light) ARG80143-010 STOP solution 12ml 4°C ARG80143-011 Plate sealer 4 strips Room temperature Summary Product Description ARG80143 Human G-CSF ELISA Kit is an Enzyme Immunoassay kit for the quantification of Human G-CSF in Serum, Plasma, Cell culture supernatants. Tested Reactivity Hu Tested Application ELISA Specificity No significant cross-reactivity or interference with Human CT-1,IL-11,OSM,CNTF,HGF,M-CSF;mouse IL-6;rat IL-6,CNTF Target Name G-CSF Conjugation HRP Conjugation Note Substrate: TMB and read at 450 nm Sensitivity 15 pg/ml Sample Type Serum, Plasma, Cell culture supernatants Standard Range 31.25 - 2000 pg/ml www.arigobio.com 1/3 Sample Volume 100 µl Precision CV: Alternate Names Granulocyte colony-stimulating factor; Lenograstim; C17orf33; GCSF; G-CSF; Filgrastim; Pluripoietin; CSF3OS Application Instructions Assay Time 4 hours Properties Form 96 well Storage instruction Store the kit at 2-8°C. -

S. No. Name of the Firm Date of Permission No. Name of the Indication Dosage Form & Strength
List of new drugs (r-DNA origin) approved for mannufacture and marketing in India for the Year 2021 S. No. Name of the firm Date of Permission No. Name of the Indication Dosage Form & Strength Rheumatoid Arthritis (RA)–Etanercept in combination with methotrexate is indicated for the treatment of moderate to severe active rheumatoid arthritis in adults when the response to disease-modifying antirheumatic drugs, including methotrexate (unless contraindicated), has been inadequate.Etanercept can be given as monotherapy in case of intolerance to methotrexate or when continued treatment with methotrexate is inappropriateEtanercept is also indicated in the treatment of severe, active and progressive rheumatoid arthritis in adults not previously treated with methotrexate. Etanercept, alone or in combination with methotrexate, has been shown to reduce the rate of progression of joint damage as measured by X-ray and to improve physical functionJuvenile Idiopathic Arthritis (JIA) – Treatment of polyarthritis (rheumatoid factor positive or negative)and extended oligoarthritis in children and adolescents from the age of 2 years who have had aninadequate response to, or who have proved intolerant of, methotrexate.Treatment of psoriatic arthritis in adolescents from the age of 12 years who have had an inadequate response to, or who have proved intolerant of, methotrexate.Treatment of enthesitis-related arthritis in adolescents from the age of 12 years who have had an inadequate response Solution for subcutaneous Injection (single use)Pre- Mylan Pharmaceuticals to, or who have proved intolerant of, conventional therapy.Etanercept has not been studied in children aged less than 2 filled syringe:(i). 50 mg/mL in Prefilled Syringes(ii). -

Novel Concepts of Treatment for Patients with Myelofibrosis And
cancers Review Novel Concepts of Treatment for Patients with Myelofibrosis and Related Neoplasms Prithviraj Bose * , Lucia Masarova and Srdan Verstovsek Department of Leukemia, University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA; [email protected] (L.M.); [email protected] (S.V.) * Correspondence: [email protected] Received: 30 August 2020; Accepted: 1 October 2020; Published: 9 October 2020 Simple Summary: Myelofibrosis (MF) is an advanced form of a group of rare, related bone marrow cancers termed myeloproliferative neoplasms (MPNs). Some patients develop myelofibrosis from the outset, while in others, it occurs as a complication of the more indolent MPNs, polycythemia vera (PV) or essential thrombocythemia (ET). Patients with PV or ET who require drug treatment are typically treated with the chemotherapy drug hydroxyurea, while in MF, the targeted therapies termed Janus kinase (JAK) inhibitors form the mainstay of treatment. However, these and other drugs (e.g., interferons) have important limitations. No drug has been shown to reliably prevent the progression of PV or ET to MF or transformation of MPNs to acute myeloid leukemia. In PV, it is not conclusively known if JAK inhibitors reduce the risk of blood clots, and in MF, these drugs do not improve low blood counts. New approaches to treating MF and related MPNs are, therefore, necessary. Abstract: Janus kinase (JAK) inhibition forms the cornerstone of the treatment of myelofibrosis (MF), and the JAK inhibitor ruxolitinib is often used as a second-line agent in patients with polycythemia vera (PV) who fail hydroxyurea (HU). In addition, ruxolitinib continues to be studied in patients with essential thrombocythemia (ET). -

Nplate (Romiplostim) Discard Any Unused Portion of the Single-Use Vial
HIGHLIGHTS OF PRESCRIBING INFORMATION Do not shake during reconstitution; protect reconstituted Nplate from These highlights do not include all the information needed to use Nplate light; administer reconstituted Nplate within 24 hours. (2.2) safely and effectively. See full prescribing information for Nplate. The injection volume may be very small. Use a syringe with graduations to 0.01 mL. (2.2) ® Nplate (romiplostim) Discard any unused portion of the single-use vial. (2.2) For subcutaneous injection ---------------------DOSAGE FORMS AND STRENGTHS---------------------- 250 mcg or 500 mcg of deliverable romiplostim in single-use vials ( 3) Initial U.S. Approval: 2008 ---------------------------RECENT MAJOR CHANGES--------------------------- -------------------------------CONTRAINDICATIONS ---------------------------- Indications and Usage (1) 07/2011 None (4) Dosage and Administration, Nplate Distribution removal 12/2011 -----------------------WARNINGS AND PRECAUTIONS------------------------ Program (2) In patients with MDS, Nplate increases blast cell counts and increases Warnings and Precautions: Progression of Myelodysplastic the risk of progression to acute myelogenous leukemia. (5.1) Syndromes (5.1) 07/2011 Thrombotic/thromboembolic complications may result from increases in Warnings and Precautions: Thrombotic/Thromboembolic platelet counts with Nplate use. Portal vein thrombosis has been Events (5.2) 07/2011 reported in patients with chronic liver disease receiving Nplate. Use Warning and Precaution: Bone Marrow Reticulin Formation with additional caution in ITP patients with chronic liver disease. (5.2) and Fibrosis (5.3) 12/2011 Discontinuation of Nplate may result in worsened thrombocytopenia Warnings and Precautions: Laboratory Monitoring (5.6) 12/2011 than was present prior to Nplate therapy. Monitor complete blood Warnings and Precautions: Nplate Distribution removal 12/2011 counts (CBCs), including platelet counts, for at least 2 weeks following Program (5.7) Nplate discontinuation. -

Romiplostim Reverts the Thrombocytopenia in Dengue Hemorrhagic Fever
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector letter Romiplostim reverts the 160 thrombocytopenia in den- gue hemorrhagic fever 140 120 To the Editor: First-genera- /L) tion thrombopoietic agents were 9 100 recombinant forms of human thrombopoietin (TPO), but their 80 development was discontinued due to the onset of neutralizing auto- 60 Platelet count (×10 antibodies cross-reacting with 40 endogenous TPO. Second-gen- eration thrombopoiesis-stimulat- 20 ing molecules (romiplostim and 0 eltrombopag), have completed 0 10 20 0 40 50 55 60 70 80 90 100 110 120 10 140 150 160 170 180 190 200 210 220 20 phase III trials in primary im- Time in days mune thrombocytopenia, whereas 9 phase II and III trials are ongoing Figure 1. Platelet count (x10 /L) by day. Arrows denote doses of romiplostim (4 µg/kg). in other conditions characterized by thrombocytopenia.1 Dengue gen and IgM antibodies were pres- DHF in which romiplostim has is the most prevalent arthropod- ent; the bone marrow had hypo- been successfully used. An immune borne virus affecting humans to- plasia and no evidence of myeloma mechanism of thrombocytopenia day causing a spectrum of disease, was found. The patient was treated due to increased platelet destruc- ranging from a mild febrile illness with intravenous hydrocortisone tion appears to be operative in pa- to a life-threatening dengue hem- (300 mg/day) and subcutaneous tients with DHF;9 however, in the orrhagic fever (DHF).2 The main filgrastim (300 ug/day), with the case that we are reporting, the previ- hematological findings of dengue neutropenia resolving 4 days later. -
Patient's Name
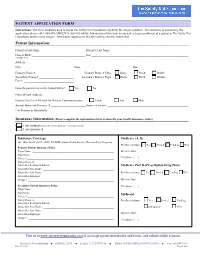
PATIENT APPLICATION FORM Instructions: This form should be used to assess The Safety Net Foundation eligibility for Amgen products. For assistance in completing this application, please call 1-888-SN-AMGEN (1-888-762-6436). Submission of this form is required to begin enrollment of a patient in The Safety Net Foundation sponsored by Amgen. Information supplied on this form will be strictly confidential. Patient Information: Patient’s First Name: ______________________________ Patient’s Last Name: ____________________________________________________ Date of Birth: ____________________________________ Sex: _________________________________________________________________ (MMDDYYYY) Address: ____________________________________________________________________________________________________________ City: ___________________________________ State: __________________________________ Zip: _________________________________ Primary Phone #: _________________________ Primary Phone # Type: Home Work Mobile Secondary Phone #: _______________________ Secondary Phone # Type: Home Work Mobile Fax #: _________________________________ Does the patient live in the United States?: Yes No Patient Email Address: _________________________________________________________________________________________________ Patient’s Preferred Method for Written Communications: Email Fax Mail Annual Household Income: $ _______________________ Source of Income: ______________________________________________________ # of Persons in Household: _________________________ -

Hematopoietic Growth Factors Version 2.2019 — March 27, 2019
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Hematopoietic Growth Factors Version 2.2019 — March 27, 2019 NCCN.org Continue Version 2.2019, 03/27/19 © 2019 National Comprehensive Cancer Network® (NCCN®), All rights reserved. NCCN Guidelines® and this illustration may not be reproduced in any form without the express written permission of NCCN. NCCN Guidelines Index NCCN Guidelines Version 2.2019 Table of Contents Hematopoietic Growth Factors Discussion *Pamela Sue Becker, MD/PhD/Chair ‡ Þ ξ Dwight D. Kloth, PharmD, BCOP ∑ Vivek Roy, MD ‡ Fred Hutchinson Cancer Research Center/ Fox Chase Cancer Center Mayo Clinic Cancer Center Seattle Cancer Care Alliance Eric H. Kraut, MD ‡ Hope S. Rugo, MD † ‡ * Elizabeth A. Griffiths, MD/Vice Chair ‡ Þ † The Ohio State University Comprehensive UCSF Helen Diller Family Roswell Park Comprehensive Cancer Center Cancer Center - James Cancer Hospital Comprehensive Cancer Center and Solove Research Institute Laura Alwan, PharmD ∑ Sepideh Shayani, PharmD ∑ ‡ Fred Hutchinson Cancer Research Center/ Gary H. Lyman, MD, MPH † ‡ City of Hope National Medical Center Seattle Cancer Care Alliance Fred Hutchinson Cancer Research Center/ Saroj Vadhan-Raj, MD † Þ Kimo Bachiashvili, MD ‡ Seattle Cancer Care Alliance The University of Texas University of Alabama at Birmingham MD Anderson Cancer Center Comprehensive Cancer Center Mary Mably, RPh, BCOP ∑ ‡ University of Wisconsin Sumithira Vasu, MBBS ‡ Mona Benrashid, PharmD ∑ Carbone Cancer Center The Ohio State University Comprehensive Vanderbilt-Ingram -

Romiplostim (Nplate), Eltrombopag (Promacta)
Clinical Policy: romiplostim (Nplate), eltrombopag (Promacta) Reference Number: CP.CPA.104 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal See Important Reminder at the end of this policy for important regulatory and legal information. Description The following are thrombopoietin receptor agonists requiring prior authorization: romiplostim (Nplate™), eltrombopag (Promacta®). FDA approved indication Nplate and Promacta are indicated for the treatment of thrombocytopenia in patients with chronic immune (idiopathic) thrombocytopenic purpura (ITP) who have had an insufficient response to corticosteroids, immunoglobulins or splenectomy. Limitation of use: Nplate and Promacta • Should be used only in patients with ITP whose degree of thrombocytopenia and clinical condition increase the risk for bleeding. • Should not be used in an attempt to normalize platelet counts. Policy/Criteria Provider must submit documentation (which may include office chart notes and lab results) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Nplate or Promacta is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Chronic Idiopathic Thrombocytopenic Purpura (ITP) (must meet all): 1. Diagnosis of ITP (chronic, relapsed, or refractory) with an increased risk for bleeding based on the degree of thrombocytopenia and clinical condition; 2. Request is for Promacta or Nplate; 3. Dose does not exceed: 10 mcg/kg/week (Nplate); 75 mg/day (Promacta). Approval duration: Promacta: Length of benefit Nplate: 6 months or to member’s renewal period, whichever is longer. B. Chronic Hepatitis C Thrombocytopenia (must meet all): 1. Diagnosis of thrombocytopenia in patients with chronic hepatitis C; 2.