CVD: Primary Care Intelligence Packs CCG: NHS Kernow CCG
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accessible Walks in South East Cornwall
Lostwithiel Riverside Walk, Lostwithiel PL22 OBS Park along the quayside in Lostwithiel, where there is no charge. With your back to the river ACCESSIBLE WALKS IN follow the road to your left, this is an ideal spot for a short stroll (15-20mins) tracking the River Fowey as it meanders through Coulson Park and then Shirehall Moor. The well defined SOUTH EAST CORNWALL path is suitable for wheelchairs and prams up until the start of the moor where it then narrows. In Coulson Park you’ll find a fenced children’s play area and picnic benches dotted along the route. Retrace your steps back to the beginning of the walk Cadsonbury Riverside Walk, Newbridge, nr Callington Take the A390 road from Liskeard to Callington. The road drops into a river valley and crosses a bridge at a place called Newbridge. Immediately before the bridge turn right along a small country lane, to a small National Trust car park about 100 metres on the right. From the car park there is a short level walk, suitable for all ,along good surfaces, that follows the wide shallow River Lynher. As the footpath ends you can either retrace your route alongside the river or follow the peaceful country lane back to the car park. For the more active, there are wonderful far reaching views from the top of Cadsonbury Hill Fort, an impressive iron age fortification. Mount Edgcumbe Country Park, Torpoint PL10 1HZ The multi-use trail at Mount Edgcumbe Country Park is designed for cyclists, walkers and riders to share. The trail is also accessible for wheelchair users. -
Minutes 26.02.19
Marazion Surgery Minutes of the Marazion Surgery Patient Participation Group Meeting on Monday 26th February 2019, at 6.30pm Present: Apologies: Mrs Juliette Benstead Mr Brian Baker Mrs Carol Brown Mrs Mary Baldwin Mr Derek Brown Mrs Janet Bullock Mrs Jackie Brown Ms Tania Cannavo Mrs Sandra Easterbrook Mrs Elizabeth Clarke Mr Leslie Lipert Mrs Serena Collins Mr Michael Miller Mrs Margaret East Mrs Mary Page Mrs Kate Ford Mr Michael Page Mrs Susan Harrison Mrs Heather Stewart Mrs Gillian Johnson Dr Neil Walden Mrs Trudy Jones Mr Barry Webb Mrs Jane King Mrs Ailean Wheeler Mrs Ann Miller Mrs Pauline Needham Mrs Fran Phillips Ms Jane Richards Mr Colin Treleven 1. Minutes of Previous Meeting: The Minutes of the meeting on 26th June 2018 were agreed to be a true record. 2. Matters Arising: 2.1 Friends & Family Test: The results are always posted on the website and in the waiting room, and continue to be extremely positive about all aspects of the surgery. 2.2 Medical Students: Feedback from the students about the Practice, and from patients about the students, continued to be very positive. The Practice was applying to become a teaching practice for GP Registrars. 2.3 Improved Access to General Practice: The Practice already offered clinics in the early morning and evening, with doctors and assistant practitioners; however the Practice was also now involved with a pilot to Improve Access to General Practice. This currently included offering evening and occasional Sunday morning clinics. 2.4 West Cornwall Hospital: Dr Walden assured the group that WCH was safe for the future with an aspiration to do more close to home, in terms of admissions from the local area and out- patient tests and services. -

Notice of Poll and Situation of Polling Stations
NOTICE OF POLL AND SITUATION OF POLLING STATIONS CORNWALL COUNCIL VOTING AREA Referendum on the United Kingdom's membership of the European Union 1. A referendum is to be held on THURSDAY, 23 JUNE 2016 to decide on the question below : Should the United Kingdom remain a member of the European Union or leave the European Union? 2. The hours of poll will be from 7am to 10pm. 3. The situation of polling stations and the descriptions of persons entitled to vote thereat are as follows : No. of Polling Station Situation of Polling Station(s) Description of Persons entitled to vote 301 STATION 2 (AAA1) 1 - 958 CHURCH OF JESUS CHRIST OF LATTER-DAY SAINTS KINGFISHER DRIVE PL25 3BG 301/1 STATION 1 (AAM4) 1 - 212 THE CHURCH OF JESUS CHRIST OF LATTER-DAY SAINTS KINGFISHER DRIVE PL25 3BG 302 CUDDRA W I HALL (AAA2) 1 - 430 BUCKLERS LANE HOLMBUSH ST AUSTELL PL25 3HQ 303 BETHEL METHODIST CHURCH (AAB1) 1 - 1,008 BROCKSTONE ROAD ST AUSTELL PL25 3DW 304 BISHOP BRONESCOMBE SCHOOL (AAB2) 1 - 879 BOSCOPPA ROAD ST AUSTELL PL25 3DT KATE KENNALLY Dated: WEDNESDAY, 01 JUNE, 2016 COUNTING OFFICER Printed and Published by the COUNTING OFFICER ELECTORAL SERVICES, ST AUSTELL ONE STOP SHOP, 39 PENWINNICK ROAD, ST AUSTELL, PL25 5DR No. of Polling Station Situation of Polling Station(s) Description of Persons entitled to vote 305 SANDY HILL ACADEMY (AAB3) 1 - 1,639 SANDY HILL ST AUSTELL PL25 3AW 306 STATION 2 (AAG1) 1 - 1,035 THE COMMITTEE ROOM COUNCIL OFFICES PENWINNICK ROAD PL25 5DR 306/1 STATION 1 (APL3) 1 - 73 THE COMMITTEE ROOM CORNWALL COUNCIL OFFICES PENWINNICK -

Land at Bicton, Bicton Road, St Ive, Liskeard, Cornwall, PL14 5RF
Land At Bicton, Bicton Road, St Ive, Liskeard, Cornwall, PL14 5RF South east facing pasture land with road and river frontage Pensilva 2.5 miles - Callington 4.5 miles - Liskeard 5.9 miles • Productive Pasture • Broadleaf Woodland • Stream and Road Frontage • 5 Practical Shaped Fields • South East Facing • Substantial Pole Framed Barn • Spectacular Views • 41.92 Acres in All • Guide price £285,000 01566 774999 | [email protected] Cornwall | Devon | Somerset | Dorset | London stags.co.uk Land At Bicton, Bicton Road, St Ive, Liskeard, Cornwall, PL14 5RF SITUATION The land is situated on the edge of Bodmin A substantial, but aged pole barn lies just Moor with spectacular, far reaching views inside the gateway. There is also a small field across to Kit Hill and the surrounding area. It shelter, roughly in the centre of the land, is mid way between Pensilva, St Ive, and where four fields meet. Golberdon, 10.8 miles from the A30 Plusha Junction and just over 6 miles from the All the fields have internal gateways between Liskeard Junction on the A38. them. The land enjoys road frontage on to a minor road and a wide entrance gateway The land lies between 125 metres and140 leads to an area of hard standing and the metres above sea level, in an area regarded barn. as good grass growing agricultural land. It is SERVICES accessed from the minor road leading from The land is naturally watered by the stream St Ive to Golberdon. that runs along the southern boundary. We DESCRIPTION understand that mains water is available The land comprises 41.92 acres of "one" field to the west and a legal right exists productive pasture land with some broadleaf to bury a pipe from the main to the land. -
MINUTES: of the Meeting of Planning And
MINUTES: of the meeting of Planning and Development Committee held in The Council Chamber, The Passmore Edwards Building, The Cross, Cross Street, Camborne, TR14 8HA on Tuesday 15th January 2019 at 6.30 pm PRESENT: Councillor C Godolphin Chairman Councillor J P Collins Councillor V Dalley Councillor Ms Z Fox Councillor L Lemon from point mentioned Councillor D Wilkins IN ATTENDANCE: Amanda Mugford, Town Clerk; Melanie Negus, Administrative Assistant and eleven members of the public. The Chairman explained the safety procedures to all present. P.4059 TO RECEIVE APOLOGIES FOR NON-ATTENDANCE P.4059.2 RESOLVED: that the apologies from Councillors Kelynack, Morgan, and Winter for non-attendance of the meeting of the Planning and Development Committee held on 15th January 2019 were received Proposed by Councillor Godolphin Seconded by Councillor Wilkins On a vote being taken the matter was approved unanimously P.4060 MEMBERS TO DECLARE DISCLOSABLE PECUNIARY INTERESTS AND NON-REGISTERABLE INTERESTS (INCLUDING THE DETAILS THEREOF) IN RESPECT OF ANY ITEMS ON THIS AGENDA INCLUDING ANY GIFTS OR HOSPITALITY EXCEEDING £25 There were no declarations of interests. P.4061 TO APPROVE WRITTEN REQUEST(S) FOR DISPENSATIONS 3182 There were no dispensation requests. P.4062 CHAIRMAN’S ANNOUNCEMENTS There were no Chairman’s announcements. P.4063 TO RECEIVE AND APPROVE THE MINUTES OF THE MEETING OF THIS COMMITTEE HELD ON THE 11TH DECEMBER 2018 AND THE CHAIRMAN TO SIGN THEM P.4063.2 RESOLVED: that the Minutes of the meeting of the Planning and Development Committee held on the 11th December 2018 were received, approved and signed by the Chairman Proposed by Councillor Godolphin Seconded by Councillor Mrs Dalley On a vote being taken the matter was approved unanimously by those entitled to vote. -

Bywood Cottage, Golberdon Road, Pensilva, Liskeard, Cornwall, PL14 5RL
Bywood Cottage, Golberdon Road, Pensilva, Liskeard, Cornwall, PL14 5RL A charming 4 bedroom semi-detached cottage occupying a delightful rural position Pensilva 0.8 miles - Liskeard 6 miles - Plymouth 20 miles • Sitting Room • Dining Room • Kitchen • Family Room • 4 Bedrooms (Master En Suite) • Integral Double Garage • Garden • Off Road Parking • Guide price £335,000 01566 774999 | [email protected] Cornwall | Devon | Somerset | Dorset | London stags.co.uk Bywood Cottage, Golberdon Road, Pensilva, Liskeard, Cornwall, PL14 5RL SITUATION room with beamed ceiling and a woodburning stove with The property occupies an enviable position less than a a stone surround. Door to the dining room with slate mile from the popular self-contained village of Pensilva, flooring, a feature stone fireplace and a doorway to the which is well served by a shop catering for most day to kitchen. The kitchen has a range of wall mounted units, day needs, health centre, part-time post office, village base units and drawers, space for appliances and a pub, primary school and church. Millennium House cooker, a sink and a door to the garage. Off the kitchen community centre offers a wide range of activities and is an inner hall with stairs leading up to the first floor. events on a daily basis. The east Cornwall towns of Callington (5 miles) and Liskeard (6 miles) have a varied The first floor comprises: a master bedroom with an en amount of shops and retail outlets, scholastic facilities to suite shower room, 3 further bedrooms, a family A-level standard and doctors', dentists' and veterinary bathroom with a bath and shower and a family room surgeries, which serve this widely based rural community. -

Duchy Health Charity
MEET THE FUNDERS SPRING EVENT 2021 Resource Document VISION AND TASK, THE HOPE OF THE WORLD, IN THIS GREAT COMMISSION WE SHARE: TO SERVE AND WORK AND PRAY, UNTIL THE KINGDOM OF LOVE IS EVERYWHERE. Dr Kathy Lang 2014 CONTENTS 01 ABOUT MtF ADDITIONAL FUNDERS 05 & RESOURCES 02 EVENT FOCUS 06 2021 PROGRAMME 03 EVENT HOSTS & 06 ATTENDEE LIST SPEAKERS 04 EXPERTS THROUGH 07 WHAT'S NEXT? EXPERIENCE Programme 25th May 10:00 AM WELCOME 10:15 AM HOUSEKEEPING 10:20 AM OPENING PRAYER 10:30 AM ALLCHURCHES TRUST LTD 10:50 AM CORNWALL HISTORIC CHURCHES TRUST 11:10 AM NATIONAL LOTTERY COMMUNITY FUND 11:30 AM BREAK 11:45 AM THE JOSEPH RANK TRUST 12:05 AM WORKSHOPS 12:40 AM NEXT STEPS & CLOSE Programme 26th May 10:00 AM WELCOME & OPENING PRAYER 10:20 AM CORNWALL COMMUNITY FOUNDATION 10:40 AM SOUTH WEST WATER 11:00 AM EXPERTS THROUGH EXPERIENCE 11:20 AM BREAK 11:30 AM NATIONAL CHURCHES TRUST 11:50 AM GROUNDWORK SOUTH 12:10 PM WORKSHOPS 12:45 PM NEXT STEPS & CLOSE ABOUT THE EVENT About The Event Meet the Funders (MtF) is an innovative year-long programme that strengthens community work in Cornwall. We support projects that address poverty, exclusion, 1 isolation, and rurality. Spring Event We believe that the best people to develop flourishing communities are the communities themselves and that faith groups in Cornwall are often at the very heart of that! MtF begins this year on the 25th and 26th of May with our 6 Spring Event. These days are an opportunity for Cornish Community projects seeking funding to meet and network with a large number of local and national funders. -
Cornwall Local Plan: Community Network Area Sections
Planning for Cornwall Cornwall’s future Local Plan Strategic Policies 2010 - 2030 Community Network Area Sections www.cornwall.gov.uk Dalghow Contents 3 Community Networks 6 PP1 West Penwith 12 PP2 Hayle and St Ives 18 PP3 Helston and South Kerrier 22 PP4 Camborne, Pool and Redruth 28 PP5 Falmouth and Penryn 32 PP6 Truro and Roseland 36 PP7 St Agnes and Perranporth 38 PP8 Newquay and St Columb 41 PP9 St Austell & Mevagissey; China Clay; St Blazey, Fowey & Lostwithiel 51 PP10 Wadebridge and Padstow 54 PP11 Bodmin 57 PP12 Camelford 60 PP13 Bude 63 PP14 Launceston 66 PP15 Liskeard and Looe 69 PP16 Caradon 71 PP17 Cornwall Gateway Note: Penzance, Hayle, Helston, Camborne Pool Illogan Redruth, Falmouth Penryn, Newquay, St Austell, Bodmin, Bude, Launceston and Saltash will be subject to the Site Allocations Development Plan Document. This document should be read in conjunction with the Cornwall Local Plan: Strategic Policies 2010 - 2030 Community Network Area Sections 2010-2030 4 Planning for places unreasonably limiting future opportunity. 1.4 For the main towns, town frameworks were developed providing advice on objectives and opportunities for growth. The targets set out in this plan use these as a basis for policy where appropriate, but have been moderated to ensure the delivery of the wider strategy. These frameworks will form evidence supporting Cornwall Allocations Development Plan Document which will, where required, identify major sites and also Neighbourhood Development Plans where these are produced. Town frameworks have been prepared for; Bodmin; Bude; Camborne-Pool-Redruth; Falmouth Local objectives, implementation & Penryn; Hayle; Launceston; Newquay; Penzance & Newlyn; St Austell, St Blazey and Clay Country and monitoring (regeneration plan) and St Ives & Carbis Bay 1.1 The Local Plan (the Plan) sets out our main 1.5 The exception to the proposed policy framework planning approach and policies for Cornwall. -

Liskeard • Looe • Polperro Callington • Liskeard Via Pensilva
SH: School Holidays Only COLL - Callywith SD: School Days Only 73/73A/74/174 via Pensilva - St Cleer NS: Not Saturdays Callington • Liskeard College Days Only SSH: Saturdays and School Holidays Only SNC: Saturday Not College Days MON to SAT except Bank Holidays SNC COLL SSH SD SD SSH SD SSH SD 73A 174 174 74 74 74 74 73 74 74 73 73 74 74 74 74 74 74 Callington Community College 0 817 1510 Callington New Road 0735 0735 0820 0820 0920 1020 122 0 14 20 1520 154 0 16 4 0 174 0 183 0 Callington Westover Road 0738 0738 0823 0823 0923 1023 1223 1423 1523 1543 1643 174 3 1833 St Ive Church End 0747 0747 0832 0832 0932 1032 1232 1432 1532 1552 1652 1752 1842 Pensilva Victoria Inn 0753 0753 0838 0838 0938 1038 123 8 1438 1538 1558 1658 175 8 184 8 Glen Park 0755 0755 0840 0840 0940 104 0 124 0 1440 154 0 16 0 0 170 0 180 0 1850 Darite Crows Nest 0758 0758 0843 0843 0943 1043 124 3 14 43 1543 16 03 1703 1803 1853 Darite Bus Shelter 0801 0801 0846 0846 0946 104 6 124 6 14 4 6 154 6 16 06 170 6 1806 1856 St Cleer Church 0808 0808 0853 0853 0953 1053 1253 14 53 1553 1613 1713 1813 19 03 Tremar Phone Box 0 8 11 0 8 11 0856 0856 0956 1056 125 6 14 56 1556 1616 1716 1816 19 0 6 Trevecca/Depot 0 817 0 817 0902 0902 10 02 11 0 2 13 0 2 1502 16 02 1622 1722 1822 1912 Liskeard Hospital Clemo Road $ $ 0906 0906 10 06 11 0 6 13 0 6 1506 16 06 1626 1626 1726 1826 1916 Liskeard Morrisons A390 $ $ 0909 0909 10 09 11 0 9 1215 13 0 9 1509 1530 16 09 1629 1629 1729 1829 1919 Liskeard Sch & Community College [Sch Grounds] $ $ $ $ $ $ $ $ $ 1525 $ $ $ $ $ $ $ Liskeard -
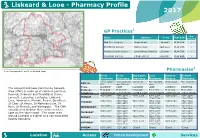
Liskeard & Looe
Liskeard & Looe - Pharmacy Profile 2017 GP Practices1 Dis - Name Address Town Post Code pensing Oak Tree Surgery Clemo Road Liskeard PL14 3XA Old Bridge Surgery Station Road East Looe PL13 1HA Pensilva Health Centre School Road, Pensilva Liskeard PL14 5RP Rosedean Surgery 8 Dean Street Liskeard PL14 4AQ 2 Note: See Appendix 1 and 2 for detailed maps Pharmacies Boots Boots Day Lewis Looe Oaktree Roberts pharmacy pharmacy pharmacy Pharmacy Surgery Pharmacy 21-22 Baytree 1-6 Coach Hse 6 Dean St Fore St, East Clemo road The Coombes Address Hill Arc, Fore St Looe Town LISKEARD LOOE LISKEARD LOOE LISKEARD POLPERRO The Liskeard and Looe Community Network Postcode PL14 4BG PL13 1DT PL14 4AA PL13 1DT PL14 3XA PL13 2RG Area (CNA) is made up of eighteen parishes; Telephone 01579 343183 01503 262980 01579 342225 01503 262243 01579 324254 01503 272250 Deviock, Dobwells and Trewidland, Duloe, 0830-1800 0900-1300 0900 - 1730 0900-1300 0830 - 1830 0900-1200 MONDAY Lanreath, Lansallos, Lanteglos, Liskeard, 1330-1800 1330-1730 1300-1730 Looe, Menheniot, Morvah, Pelynt, Quethiock, 0830-1800 0900-1300 0900 - 1730 0900-1300 0830 - 1830 0900-1200 TUESDAY St Cleer, St Keyne, St Martinby-Looe, St 1330-1800 1330-1730 1300-1730 0830-1800 0900-1300 0900 - 1730 0900-1300 0800 - 1830 0900-1200 Neot, St Pinnock, and Warleggan. The CNA WEDNESDAY 1330-1800 1330-1730 1400-1800 extends from Bodmin Moor in the north to 0830-1800 0900-1300 0900 - 1730 0900-1300 0800 - 1830 0900-1200 THURSDAY Looe on the south coast. The urban area 1330-1800 1330-1730 1400-1800 around Liskeard is subject to a non-controlled 0830-1800 0900-1300 0900 - 1730 0900-1300 0830 - 1830 0900-1200 FRIDAY locality boundary. -

Area Food Deliveries Other Support Liskeard Kevin James, Milkman – a Wide Selection of FB Page: Liskeard COVID-19 Food and Essentials Available Too
Area Food deliveries Other Support Liskeard Kevin James, Milkman – A wide selection of FB Page: Liskeard COVID-19 food and essentials available too. – covering Help and Support Liskeard, Looe, Torpoint, Polperro, Bodmin, FB Page: Dobwalls and Saltash, Launceston and everywhere Liskeard Coronavirus Support between: 01579 340 386 Liskeard and Looe Foodbank: Victoria Inn (Pensilva) – Meals on Wheels: 07512 011452 01579 363933 Beddoes Fruit and Veg (Liskeard) – Home deliveries: 01579 363 933 Phillip Warren – Oughs Butchers (Liskeard) – Home deliveries: 07423327218 Spar (Menheniot) – Home deliveries: 01579 342266 Horizon Farm Shop – Groceries and meals delivered (St Cleer/Pensilva etc): 01579 557070 Crows Nest (Meals home delivered): 01579 345930 Liskeard Pet Shops (Deliveries): 01579 347 144 Highwayman (Dobwalls) Meals Home delivered): 01579 320114 Village Greens Mount (deliveries to Warleggan Parish, St Neot and Cardinham) 07815619754 The Fat Frog (Home delivery in 2.5 mile radius of Liskeard): 01579 348818 The Liskeard Tavern (Staff willing to volunteer in their community): 01579 341752 Pensilva Stores (Home Deliveries Pensilva): 01579 362457 Rumours Cafe (Free local delivery Liskeard): 01579 342302 Looe Tredinnick Farm Shop - (Looe and FB: Looe Coronavirus Support surrounding area): 01503 240992 FB: Pelynt COVID community Support Sarahs Taxis (Able to deliver items to home FB: Morval and Widegates for free) 01503 265688 covid 19 support group FB: Polruan isolation support Café Fleur (Meals can be dropped to your car): 01503 265734 Liskeard -

THE DIOCESE of TRURO – June 2006
DIOCESE OF TRURO Church House, Woodlands Court, Truro Business Park Threemilestone, Truro, TR4 9NH Daily Intercessions including Anglican World Cycle April 2017 1 Frederick Denison Maurice, priest, teacher of the faith, 1872 Bishop Tim returning from his sabbatical Sa Missouri (V, The Episcopal Church) + Wayne Smith. West Missouri (VII, The Episcopal Church) + Martin Field. 2 FIFTH SUNDAY OF LENT. The Cathedral – Roger Bush (C), Lynda Barley (C), Alan Bashforth (C), Mark Chapman (C), Simon Griffiths (C), Jane Horton (C) & the other members of the Chapter, Audrey Elkington (C), Helen Davies & Daphne Skinnard. Deanery of Carnmarth North – Vacant (RD), Sally Piper (LC). Su Porvoo: Church of Ireland: Diocese of Armagh, Archbishop Richard Clarke; Evangelical Lutheran Church in Denmark: Diocese of Funen, Bishop Tine Lindhardt. AWC: Mityana (Uganda) + Stephen Kaziimba. 3 Members of the Episcopal College meeting today M Mombasa (Kenya) + Julius Katio Kalu. 4 The Rural Deans meeting today Tu Monmouth (Wales) + Richard Pain. 5 The Lay Chairs of our deaneries W Montana (VI, The Episcopal Church) + Charles Franklin Brookhart. 6 Members of Deanery Synods Th Montreal (Canada, Canada) + Mary Irwin-Gibson. 7 United Nations World Health Day* St Goran (Patr’l) w St Michael Caerhays – Christopher Newell (C), Graham Downes (R). F Moosonee (Ontario, Canada) + Thomas Corston. 8 For all those working in Church House Sa Moray, Ross & Caithness (Scotland) + Mark Strange. 9 PALM SUNDAY Boscastle and Tintagel Group of Churches – includes Minster (Patronal) and Tintagel (Patronal) - Churchwardens and Parish Officers, for their parishes in transition. Su Porvoo: Church of Sweden: Diocese of Uppsala, Archbishop Antje Jackelén, Bishop Ragnar Persenius; Church in Wales: Diocese of Llandaff, Archbishop Barry Morgan, Bishop David Wilbourne.