Dry Eye- Study of Prevalence, Associated Risk Factors and Frequency of Symptoms in Meerut District
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

District Census Handbook, 33-Banda, Uttar
CENSUS 1961 DISTRICT CENSUS HANDBOOK UTTAR PRADESH 33-BANDA DISTRICT LUCKNOW: Superintendent, Printing and Stationery, U. P. (India) 1965 [Price Rs. 10.00 Preface: • Introduction I-CENSUS TABLES A-GENERAL POPULATION TABLES A-I Area, Houses and Population Appendix II-Number of Villages with a Population of 5,000 and over and Towns with Ii 6 Population unuer 5,000 6 Appendix Ill-Houseless and Institutional Population 6 A--II Variation in Population during Sixty Years 7 Appendix 1951 Population according to the territorial jurisdiction in 1951 and cbanges in area and population invalved in those changes 7 A-III Villages Classified by Population a A-IV Towns (and Town-groups) classified by Population in 1961 with Variation since 1941 9 Appendix New Towns added in 1961 and Towns in 1951 declassified in 1961 10 Explanatory Note to the Appendix 10 B-GENERAL ECONOMIC TABLES B-1 & II Workers and Non-workers in District and Towns classified by Sex and Broad Age-groups 12 B-III Part A-Industrial Classification of Workers and Non-workers by Educational Levels in Urban Areas only 18 Part B-Industrial Classification of Workers and Non-workers by Educational Levels in Rural Areas only 20 B-IV Part A-Industrial Classification by Sex and Class of Worker of Peraona at Work at Household Industry Part B-Industrial Classification by Sex and Class of Worker of Persons at Work in Non-household Industry, Trade, Business, Profession or Service 28 Part C-Industrial Classification by Sex and Divisions, Major Groups and Minor Groups of Persons at Work other than Cultivation 35 Occupational Claasification by Sex of Persons at Work other than Cultivation. -

District Population Statistics, 45-Kheri, Uttar Pradesh
Census' of India, 1951 ·DISTRICT POPULATION STATISTICS UTTAR PRADESH 45-KHERI DISTRlCT· • 1 I 315.42 1111 KHEDPS . OFFICE OF THE REGISTRAR . GENERAL, INDIA, NEW DELHI . 82011 ( LIBRARY) Class No._ 315.42 Book No._ 1951 KHE DPS 21246 Accession 1\10. ________ >ULED CASTES IN UTTAR PRADESH _h.e Constitution (Scheduled Castes) Order, 1950] ~~~~-------------------------------- (1) Throughout the State- <H Agariya (22) Bhuyi6l' (43) Kanjar (2) Badi . (23) Boria . (44) Kap6l'iya (3) Badhik (24) Chamar (45) Karwal (4) Baheliya (25) Chero (46) Khaira.hA (5) B&iaa (26) Dabgar t47) Kharot. (b) Baisw6l' (27) Dhangar (48) KJia.rw6l' (excluding Benbl\llSj) (7) Bajaniya (28) Dhanuk (49) Kol (8) Bajgi (29) Dbarkar (50) Korwa (9) Balahar (30) DhQbi (51) Lalbegi /(I0) Ba,lmiki (31) Dhusia OJ' Jhusia _ (52) Majhw6l' (II) Bangali (32) Dom j53) Nat ~ (12) Banmanus (33) DOmar (54) Panltha (13) Bansphor (34) Dusadh ;I (55) Par~ya (l~) Barwar (3"5). GhMami (56) P~i . (15) Basor (36) Ghasiya (57) Patari (16) Bawariya (37) Gual (58) Rawat (17) Beldar (38) Habura. (59) Saharya (lS) Seriya. (39) Hilori (60, Salia.urhiyllo (19) Bha.n.tu (40}'He~ (61) StmBiya . (20) Bhoksa (41) .Jatava (621 Shilpkar (21) Bhuiya (42) Kalaha7l (63) Turaiha (2) In B'Undelkhand Division and the portion 0/ Mi~,ap'U;',District,'~(Juth of Kaimu,. > Rang.e- . -, .'- Gond FOREWORD THE Uttar Pradesh Government asked me in March, 1952, to supply them for the purposes of elections to local bodies population statistics with separation for scheduled castes (i) mohallaJward-wise for urban areas, and (ii) village-wise for rural areas. -

List of Examination Centres for Even Semester Exam 2011 – 12 (MAY-2012) Sr
List of Examination Centres For Even Semester Exam 2011 – 12 (MAY-2012) Sr. Code, Name and Address of List of Institutions whose student shall appear at the examination Code of Nodal Centre No. Examination Centres Centres for Theory Examination to which examination centre is attached 1 2 3 4 5 1 (001) Anand Engineering 1. (002) Faculty Of Engineering & Technology, Agra B. Tech 001 Agra College, Agra College, Agra 2. (006) Agra Public Institute Of Technology & B.Phar Computer Education (Deptt. Of Pharmacy), Agra 3. (243) College Of Pharmacy Agra, Agra B.Phar 4. (314) Sai Nath College Of Pharmacy,Agra B.Phar 5. (617) Uttam Institute Of Management Studies,Agra MBA 6. (659) Heritage Institute Of Hotel & Tourism,Agra BHMCT 2 (003)Babu Mohan Lal Arya 1. (004) R.B.S.College, Faculty Of Engg.& B.Tech 001 Agra Smarak Engg. College, Agra Technology,Agra Agra 2. (278) Aryan Institute Of Management And Computer MBA Studies,Agra 3. (338) K. P. Engineering College ,Agra B.Tech, MBA 4. (436) K. P. College Of Management,Agra MBA 3. (004) R.B.S.College, Faculty Of 1. (001) Anand Engineering College, Agra B.Tech, 001 Agra Engg. & Technology,Agra MBA,MCA 4. (005) Raja Balwant Singh 1. (003) Babu Mohan Lal Arya Smarak Engg. College, B.Tech, MBA 001 Agra College,Agra Agra 5. (064) Hindustan College Of 1. (317) Dhanwantri Institute Of Pharmacy,Mathura B.Phar 001 Agra Science & Technology, Mathura 2. (366) Nikhil Institute Of Engineering & B.Tech, MBA Management,Mathura 3. (394) College Of Business Studies,Agra MBA 4. -

Solid Waste Management and Characteristics in Lucknow, Uttar Pradesh, India
International Journal of Scientific & Engineering Research, Volume 4, Issue 11, November-2013 1645 ISSN 2229-5518 Solid Waste Management and Characteristics in Lucknow, Uttar Pradesh, India Rahul Charles Francis, L.P.Singh, Earnest Vinay Prakash Department of Mechanical Engineering, Sam Higginbottom Institute of Agriculture Technology and Sciences (Deemed University), Naini, Allahabad 211007,Uttar Pradesh, India Abstract Increasing population levels, rapid economic growth and rise in community living standard accelerates the generation rate of muni-cipal solid waste (MSW) in Indian cities. Improper management of SW (Solid Waste) causes hazards to inhabitants. The objectives of the study areto determine the quantitative and qualitative characteristics of SW along with basic information and to create GIS maps for Lucknow city. The samples have been randomly collected from various locations and analyzed to determine the characteristics of SW. A ques-tionnaire survey has been carried out to collect data from inhabitants including SW quantity, collection frequency, satisfaction level,etc. The Geographic Information System (GIS) has been used to analyze existing maps and data, to digitize the existing sanitary ward boundaries and to enter the data about the wards and disposal sites. The total quantity of MSW has been reported as 800 ton/day, and the average generation rate of MSW has been estimated at 0.65 kg/capita/day. The generated Arc GIS maps give efficient information concerning static and dynamic parameters of the municipal solid waste management (MSWM) problem such as the generation rate of MSW in different wards, collection point locations, MSW transport means and their routes, and the number of disposal sites and their attributes. -

District Fact Sheet Bara Banki Uttar Pradesh
Ministry of Health and Family Welfare National Family Health Survey - 4 2015 -16 District Fact Sheet Bara Banki Uttar Pradesh International Institute for Population Sciences (Deemed University) Mumbai 1 Introduction The National Family Health Survey 2015-16 (NFHS-4), the fourth in the NFHS series, provides information on population, health and nutrition for India and each State / Union territory. NFHS-4, for the first time, provides district-level estimates for many important indicators. The contents of previous rounds of NFHS are generally retained and additional components are added from one round to another. In this round, information on malaria prevention, migration in the context of HIV, abortion, violence during pregnancy etc. have been added. The scope of clinical, anthropometric, and biochemical testing (CAB) or Biomarker component has been expanded to include measurement of blood pressure and blood glucose levels. NFHS-4 sample has been designed to provide district and higher level estimates of various indicators covered in the survey. However, estimates of indicators of sexual behaviour, husband’s background and woman’s work, HIV/AIDS knowledge, attitudes and behaviour, and, domestic violence will be available at State and national level only. As in the earlier rounds, the Ministry of Health and Family Welfare, Government of India designated International Institute for Population Sciences, Mumbai as the nodal agency to conduct NFHS-4. The main objective of each successive round of the NFHS has been to provide essential data on health and family welfare and emerging issues in this area. NFHS-4 data will be useful in setting benchmarks and examining the progress in health sector the country has made over time. -

District Population Statistics, 4-Meerut, Uttar Pradesh
I Census of India, 195 1 DISTRICT POPULATION STATISTICS UTTAR PRADESH 4-MEEl{UT DISTRICT 315.42 ALLAHABAD: TING AND STATIONERY, UTTAR PRADESH, INDIA 1951 1952 MEE DPS Price, Re.1-S. FOREWORD THE Uttar Pradesh Government asked me in March. 1952, (0 'supply them for the purposes of elections to local bodies population statistics with ,separation for scheduled castes (i) mohalla/ward-wise for urban areas, and (ii) village-wise for rural areas. The Census Tabulation Plan did nbt provide for sorting of scheduled cast<;s population for areas smaller than a tehsil or urban tract and the request from the Uttar Pradesh Government came when the slip sorting had been finished and (he Tabulation Offices closed. As the census slips are mixed up for the purposes of sorting in one lot for a tehsil or urban tract, collection of data regarding scheduled castes population by moh'allas/wards and villages would have involved enormous labour and expense if sorting of the slips had been taken up afresh. Fortunately, however, a secondary census record, viz. the National Citizens' Register, in which each slip has been copied, was available. By singular foresight it had been pre pared mohalla/ward-wise for urban areas and village-wise for rural areas. Th e required information has, therefore. been extracted from. this record, 2. In the above circumstances there is a slight difference in the figures of population as arrived at by an earlier sorting of the slips and as now determined by counting from the National Citizens' Register. This difference has been accen mated by an order passed by me during the later coum from the National Register of Citizens as follows:- (i) Count Ahirwars of Farrukhabad District, Raidas and Bhagar as ·Chamars'. -

District Population Statistics, 22 Allahabad, Uttar Pradesh
.------·1 Census of India, 1951 I DISTRICT POPULATION STATISTICS UTTAR PRADESH 22-ALLAHABAD DISTRICT t I 315.42 ALLAHABAD: PluNnNG AND STATIONERY, UTTAR PRADESH, INDIA 1951 1953 ALL CPS Price, Re.1-S. FOREWORD THE Uttar Pradesh Government asked me in March, 1952, to supply them for the purposes of elections to local bodies population statistics with separation for scheduled castes (i) mohalla/ward -wise for urban areas, and (ii) village-wise for rural areas. The Census Tabulation Plan did not provide for sorting of scheduled castes population for areas smaller than a tehsil or urban tract and the request from the Uttar Pradesh Government came when the slip sorting had been finished and the Tabulation Offices closed. As the census slips are mixed up for the purposes of sorting in one lot for a tehsil or urban tract, collection of data regarding scheduled castes population by mohallas/wards and villages would have involved enormous labour and expense if sorting of the slips had been taken up afresh. Fortunately, however, a secondary census record, viz. the National Citizens' Register, in which each slip has been copied, was available. By singular foresight it had been pre pared mohalla/ward-wise for urban areas and village-wise for rural areas. The required information has, therefore, been extracted from this record. 2. In the above circumstances there is a slight difference in the figures of population as arrived at by an earlier sorting of the slips and as now determined by counting from the National Citizens' Register. This difference has been accen tuated by an order passed by me during the later count. -
LOK SABHA UNSTARRED QUESTION NO. 1326 to BE ANSWERED on 10.02.2020 REGARDING PROMOTION of CNG and PNG List of Geographical Areas Covered Till 10Th CGD Bidding Round
LOK SABHA UNSTARRED QUESTION NO. 1326 TO BE ANSWERED ON 10.02.2020 Promotion of CNG and PNG 1326. SHRI SANGAM LAL GUPTA: SHRI RAMDAS C. TADAS: पेट्रोलियम और प्राकृलिक गैस मंत्री Will the Minister of PETROLEUM AND NATURAL GAS be pleased to state: (a) whether the Government proposes to promote the use of CNG and PNG to control pollution; (b) if so, the cities of Uttar Pradesh and Maharashtra which have been connected to CNG and PNG supply so far along with the cities proposed to be connected in the near future; (c) whether the Government proposes to connect Pratapgarh in Uttar Pradesh and Wardha and Amravati in Maharashtra with CNG and PNG supply by opening CNG and PNG stations there; (d) if so, the details thereof along with the time by which it is likely to be done; and (e) if not, the reasons therefor? ANSWER पेट्रोलियम और प्राकृलिक गैस मंत्री (श्री धमेन्द्र प्रधान) MINISTER OF PETROLEUM AND NATURAL GAS (SHRI DHARMENDRA PRADHAN) (a) : Government has taken a series of decisions to promote use of CNG and PNG. (b) to (e) : Development of City Gas Distribution (CGD) networks supports the availability and accessibility of natural gas in form of Piped Natural Gas (PNG) to households, industrial uses and Compressed Natural Gas (CNG) for transportation uses. Petroleum & Natural Gas Regulatory Board (PNGRB) is the authority to grant authorization to the entities for developing of CGD network in Geographical Areas (GAs) as per PNGRB Act, 2006. PNGRB identifies GAs for authorizing the development of CGD network in synchronization with the development of natural gas pipeline connectivity and natural gas availability. -

Ground Water Scenario of Lakhimpur Kheri District, Up
GROUND WATER SCENARIO OF LAKHIMPUR KHERI DISTRICT, U.P. (A.A.P.: 2012-2013) By Dr. D.S. Pandey Scientist 'D' CONTENTS Chapter Title Page No. DISTRICT AT A GLANCE ..................2 I. INTRODUCTION ..................5 II. CLIMATE & RAINFALL ..................5 III. GEOMORPHOLOGY & SOIL TYPES ..................6 IV. GROUND WATER SCENARIO ..................6 V. GROUND WATER MANAGEMENT STRATEGY ..................8 VI. GROUND WATER RELATED ISSUE AND PROBLEMS ..................9 VII. MASS AWARENESS PROGRAMME ..................9 PLATES: I. INDEX MAP OF LAKHIMPUR KHERI DISTRICT, U.P. II. PRE-MONSOON DEPTH TO WATER LEVEL MAP (MAY, 2012) OF LAKHIMPUR KHERI DISTRICT, U.P. III. POST-MONSOON DEPTH TO WATER LEVEL MAP (NOV. 2012) OF LAKHIMPUR KHERI DISTRICT, U.P. IV. DYNAMIC GROUND WATER RESOURCES OF LAKHIMPUR KHERI DISTRICT, U.P. V. GROUND WATER USER MAP, LAKHIMPUR KHERI DISTRICT, U.P. VI. ARSENIC AFFECTED AREA OF LAKHIMPUR KHERI DISTRICT, U.P. VII. Exploratory Tubewells (C.G.W.B.) For Arsenic Studies DISTRICT AT GLANCE 1. GENERAL INFORMATION i. Geographical Area (Sq. Km.) : 7680.00 ii. Administrative Divisions (as on 31.3.2005) Number of Blocks : 6/15 Number of Panchayat Villages : 1829 iii. Population (as on 2001 census) : 32,07,234 iv. Average Annual Rainfall (mm) : 1093.50 mm 2. GEOMORPHOLOGY Major Physiographic Units : Older & Younger Alluvium Major Drainages : Gomati & Ghaghra 3. LAND USE (Sq. Km.) a) Forest area (Sq. Km.) : 2321.54 b) Net area sown (Sq. Km.) : 4863.82 c) Cultivable area (Sq. Km.) : 4863.82 4. MAJOR SOIL TYPES : Sandy Loam 5. AREA UNDER PRINCIPAL CROPS (as on 2004-05) : 6984.20 6. IRRIGATION BY DIFFERENT SOURCES (Areas and Number of Structures) (Sq.Km.) Dugwells : 168 Tubewells / Borewells : 713 state tubewells & 108430 Private tubewells Canals : 641 Km. -

Meerut-Baghpat Sl.No. 1 2 3 4 5 6 7 8 Service Code T322 T322 T322 T322 T322 T322 T322 T322 Depot Baishali Baishali Baishali Bais
MEERUT-BAGHPAT SL.NO. 1 2 3 4 5 6 7 8 SERVICE CODE T322 T322 T322 T322 T322 T322 T322 T322 DEPOT BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI REGION MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT FROM MEERUT DEP. 0 0 5:30 5:40 5:50 6:00 6:05 6:10 6:15 6:20 BAGHPAT ARR. 52 52 7:45 7:55 8:05 8:15 8:20 8:25 8:30 8:35 BAGHPAT-MEERUT SL.NO. 1 2 3 4 5 6 7 8 SERVICE CODE T321 T321 T321 T321 T321 T321 T321 T321 DEPOT BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI REGION MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT FROM BAGHPAT DEP. 0 0 8:15 8:25 8:35 8:45 8:50 8:55 9:00 9:05 MEERUT ARR. 52 52 10:30 10:40 10:50 11:00 11:05 11:10 11:15 11:20 Page 1 of 7 MEERUT-BAGHPAT SL.NO. 9 10 11 12 13 14 15 16 SERVICE CODE T322 T322 T322 T322 T322 T322 T322 T322 DEPOT BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI REGION MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT FROM MEERUT DEP. 0 0 6:25 6:30 6:35 6:40 6:45 6:50 6:55 9:00 BAGHPAT ARR. 52 52 8:40 8:45 8:50 8:55 9:00 9:05 9:10 11:00 BAGHPAT-MEERUT SL.NO. 9 10 11 12 13 14 15 16 SERVICE CODE T321 T321 T321 T321 T321 T321 T321 T321 DEPOT BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI BAISHALI REGION MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT MEERUT FROM BAGHPAT DEP. -

List of Ph.D. Awarded
Geography Dept. B.H.U.: List of PhD awarded, 1958-2013 1 Updated: 19 August 2013: The 67th Geography Foundation Day B.H.U. Banaras Hindu University, Varanasi, UP 221005. INDIA Department of Geography Doctoral Dissertation, Ph.D., in Geography: 1958 – 2013. No. Name of Scholar Title of the Doctoral Dissertation Awarded, & pub. year 1 2 3 4 1. Supervisor : Prof. Ram Lochan Singh (1946-1977) (late) 1. Shanti Lal Kayastha Himalayan Beas-Basin : A Study in Habitat, Economy 1958 and Society Pub. 1964 2. Radhika Narayan Ground Water Hydrology of Meerut District, U.P 1960 Mathur (earlier worked under Prof. Raj Nath, Geology Dept.) Pub. 1969 3. M. N. Nigam Urban Geography of Lucknow : (Submitted at Agra 1960 University) 4. S. L. Duggal Land Utilization Pattern in Moradabad District 1962 (submitted at Punjab University) 5. Vijay Ram Singh Land Utilization in the Neighbourhood of Mirzapur, U.P. 1962 Pub. 1970 6. Jagdish Singh Transport Geography of South Bihar 1962 Pub. 1964 7. Baccha Prasad Rao Vishakhapatanam : A Study in Geography of Port Town 1962 Pub. 1971 8. (Ms) Surinder Pannu Agro-Industrial Relationship in Saryupar Plain of U.P. 1962 9. Kashi N. Singh Rural Markets and Rurban Centres in Eastern U.P. 1963 10. Basant Singh Land Utilization in Chakia Tahsil, Varanasi 1963 11. Ram Briksha Singh Geography of Transport in U.P. 1963 Pub. 1966 12. S. P. Singh Bhagalpur : A Study in Regional Geography 1964 13. N. D. Bhattacharya Murshidabad : A Study in Settlement Geography 1965 14. Attur Ramesh TamiInadu Deccan: A Study. in Urban Geography 1965 15. -
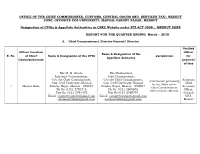
Meerut Zone, Opposite Ccs University, Mangal Pandey Nagar, Meerut
OFFICE OF THE CHIEF COMMISSIONER, CUSTOMS, CENTRAL GOODS AND SERVICES TAX:: MEERUT ZONE, OPPOSITE CCS UNIVERSITY, MANGAL PANDEY NAGAR, MEERUT Designation of CPIOs & Appellate Authorities in CBEC Website under RTI ACT 2005 :: MEERUT ZONE REPORT FOR THE QUARTER ENDING March – 2018 A. Chief Commissioner/ Director General/ Director Notified Office/ Location Officer Name & Designation of the S. No. of Chief Name & Designation of the CPIO Jurisdiction for Appellate Authority Commissionerate payment of fees Shri R. K. Gupta, Shri Roshan Lal, Assistant Commissioner, Joint Commissioner O/o the Chief Commissioner, O/o the Chief Commissioner, Assistant Information pertaining Opp. CCS University, Mangal Opp. CCS University, Mangal Chief to the Office of the 1 Meerut Zone Pandey Nagar, Meerut - 250004 Pandey Nagar, Meerut - 250004 Accounts Chief Commissioner, Ph No: 0121-2792745 Ph No: 0121-2600605 Officer, Meerut Zone, Meerut. Fax No: 0121-2761472 Fax No:0121-2769707 Central Email: [email protected] Email: [email protected] GST, [email protected] [email protected] Meerut B. Commissioner/ Addl. Director General Notified S. Commission Name & Designation of the officer for Name & Designation of the CPIO Jurisdiction No. erate Appellate Authority payment of fees Areas falling Shri Kamlesh Singh Shri Roshan Lal Joint Commissioner under the Assistant Chief Assistant Commissioner Districts of Accounts O/o the Commissioner, Office of the Commissioner of Central Meerut, Officer, Office Central GST Commissionerate Goods & Services Tax, Baghpat, of the Central GST Meerut, Opp. CCS University, Commissionerate: Meerut, Opposite: Muzaffarnagar, Commissioner Meerut Mangal Pandey Nagar, Meerut. Saharanpur, 1 Chaudhary Charan Singh University, of Central Commissione Fax No: 0121-2792773 Shamli, Goods & Mangal Pandey Nagar, Meerut- rate Amroha, Services Tax, 250004 Moradabad, Commissionera Bijnore and te: Meerut Ph No: 0121-2600605 Rampur in the Fax No:0121-2769707 State of Uttar Pradesh.