Urban Health Status in Ahmedabad City: GIS Based Study of Baherampura, Kubernagar, and Vasna Wards
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Kindly Send Your Correct Contact Details(Address, Mobile No., E-Mail Id) at [email protected] LIST of MEMBERS WHOSE ADDRESS ARE NOT CORRECT
LIST OF MEMBERS WHOSE ADDRESS ARE NOT CORRECT Membersh Category Name ip No. Name Address City PinCode EMailID IND_HOLD 6454 Mr. Desai Shamik S shivalik ,plot No 460/2 Sector 3 'c' Gandhi Nagar 382006 [email protected] Aa - 33 Shanti Nath Apartment Opp Vejalpur Bus Stand IND_HOLD 7258 Mr. Nevrikar Mahesh V Vejalpur Ahmedabad 380051 [email protected] Alomoni , Plot No. 69 , Nabatirtha , Post - Hridaypur , IND_HOLD 9248 Mr. Halder Ashim Dist - 24 Parganas ( North ) Jhabrera 743204 [email protected] IND_HOLD 10124 Mr. Lalwani Rajendra Harimal Room No 2 Old Sindhu Nagar B/h Sant Prabhoram Hall Bhavnagar 364002 [email protected] B-1 Maruti Complex Nr Subhash Chowk Gurukul Road IND_HOLD 52747 Mr. Kalaria Bharatkumar Popatlal Memnagar Ahmedabad 380052 [email protected] F/ 36 Tarun - Nagar Society Part - 2 Opp Vishram Nagar IND_HOLD 66693 Mr. Vyas Mukesh Indravadan Gurukul Road, Mem Nagar, Ahmedabad 380052 [email protected] 8, Keshav Kunj Society, Opp. Amar Shopping Centre, IND_HOLD 80951 Mr. Khant Shankar V Vatva, Ahmedabad 382440 [email protected] IND_HOLD 83616 Mr. Shah Biren A 114, Akash Rath, C.g. Road, Ahmedabad 380006 [email protected] IND_HOLD 84519 Ms. Deshpande Yogita A - 2 / 19 , Arvachin Society , Bopal Ahmedabad 380058 [email protected] H / B / 1 , Swastick Flat , Opp. Bhawna Apartment , Near IND_HOLD 85913 Mr. Parikh Divyesh Narayana Nagar Road , Paldi Ahmedabad 380007 [email protected] 9 , Pintoo Flats , Shrinivas Society , Near Ashok Nagar , IND_HOLD 86878 Ms. Shah Bhavana Paldi Ahmedabad 380006 [email protected] IND_HOLD 89412 Mr. Shah Rajiv Ashokbhai 119 , Sun Ville Row Houses , Mem Nagar , Ahmedabad 380052 [email protected] B4 Swetal Park Opp Gokul Rowhouse B/h Manezbaug IND_HOLD 91179 Mr. -

Sr. No Age Sex Address 1 64 M Sundarlal Ni Chali, Near
COVID ‐ 19 POSITIVE CASE LIST 05.05.2020, 08:00 PM SR. NO AGE SEX ADDRESS SUNDARLAL NI CHALI, NEAR SANGEETHA FURNITURE, 164M SAIJPUR, AHMEDABAD. 46, PATANI, SANJOGNAGAR, MEGHANINAGAR, 28F AHMEDABAD. 46, PATANI, SANJOGNAGAR, MEGHANINAGAR, 314F AHMEDABAD. 45, BHAVSAR NI CHALI, OPP. SHARDABEN HOSPITAL, 448M SARASPUR, AHMEDABAD. 5 57 M 753/3, AMBAVDI, SARDARNAGAR, AHMEDABAD. 6 25 F 753/2, AMBAVDI, SARDARNAGAR, AHMEDABAD. 7 28 F 753/2, AMBAVDI, SARDARNAGAR, AHMEDABAD. 8 26 M 753/3, AMBAVDI, SARDARNAGAR, AHMEDABAD. 9 8 M 753/3, AMBAVDI, SARDARNAGAR, AHMEDABAD. C‐2, SURDHARA SOCIETY, OPP. RAMINI CHALI, RAKHIAL, 10 35 F AHMEDABAD. C‐2, SURDHARA SOCIETY, OPP. RAMINI CHALI, RAKHIAL, 11 32 F AHMEDABAD. 54, BHOIWALA NI POLE, DILLI CHAKLA, SHAHPUR, 12 33 M AHMEDABAD. 52/1233, GUJRAT HOUSING BOARD, MEGHANINAGAR, 13 45 M AHMEDABAD. 6, HIREN APARTMENT, RAMNAGAR, SABARMATI, 14 53 M AHMEDABAD. 3603, MOTI VHORWAD, ASTODIYA KAJI NA DHABA, 15 56 F JAMALPUR, AHMEDABAD. A‐10, GUIMOHAR SOCIETY, NEAR THE NEW AGE SCHOOL, 16 55 M OPP. MEMON HALL, JUHAPURA‐SARKHEJ ROAD, AHMEDABAD. 206, 2/F, MADNI APARTMENT, KAZI NA DHABA, 17 54 F ASTODIA, AHMEDABAD. SR. NO AGE SEX ADDRESS 22, SHREEMAT SOCIETY, NR DUDHWALI CHALI, MELDI 18 62 F MATA NU MANDIR, BEHRAMPURA, AHMEDABAD. 181, SARVODAY NAGAR SOCIETY, OUTSIDE SHAHPUR 19 30 F GATE, SHAHPUR, AHMEDABAD. 20 75 F 1, MANMANDIR ROW HOUSE, VEJALPUR, AHMEDABAD. VASUDEV DHANJEE NICHALI, GITA MANDIR, 21 32 F AHMEDABAD. 45/K, RATAN POL, SHETH NI POL, MANEK CHOWK, 22 35 F AHMEDABAD. MAHAJAN NO VANDDO, VASANT NAGAR POLICE 23 50 M STATION SAME, JAMALPUR, AHMEDABAD. -
Section 124- Unpaid and Unclaimed Dividend
Sr No First Name Middle Name Last Name Address Pincode Folio Amount 1 ASHOK KUMAR GOLCHHA 305 ASHOKA CHAMBERS ADARSHNAGAR HYDERABAD 500063 0000000000B9A0011390 36.00 2 ADAMALI ABDULLABHOY 20, SUKEAS LANE, 3RD FLOOR, KOLKATA 700001 0000000000B9A0050954 150.00 3 AMAR MANOHAR MOTIWALA DR MOTIWALA'S CLINIC, SUNDARAM BUILDING VIKRAM SARABHAI MARG, OPP POLYTECHNIC AHMEDABAD 380015 0000000000B9A0102113 12.00 4 AMRATLAL BHAGWANDAS GANDHI 14 GULABPARK NEAR BASANT CINEMA CHEMBUR 400074 0000000000B9A0102806 30.00 5 ARVIND KUMAR DESAI H NO 2-1-563/2 NALLAKUNTA HYDERABAD 500044 0000000000B9A0106500 30.00 6 BIBISHAB S PATHAN 1005 DENA TOWER OPP ADUJAN PATIYA SURAT 395009 0000000000B9B0007570 144.00 7 BEENA DAVE 703 KRISHNA APT NEXT TO POISAR DEPOT OPP OUR LADY REMEDY SCHOOL S V ROAD, KANDIVILI (W) MUMBAI 400067 0000000000B9B0009430 30.00 8 BABULAL S LADHANI 9 ABDUL REHMAN STREET 3RD FLOOR ROOM NO 62 YUSUF BUILDING MUMBAI 400003 0000000000B9B0100587 30.00 9 BHAGWANDAS Z BAPHNA MAIN ROAD DAHANU DIST THANA W RLY MAHARASHTRA 401601 0000000000B9B0102431 48.00 10 BHARAT MOHANLAL VADALIA MAHADEVIA ROAD MANAVADAR GUJARAT 362630 0000000000B9B0103101 60.00 11 BHARATBHAI R PATEL 45 KRISHNA PARK SOC JASODA NAGAR RD NR GAUR NO KUVO PO GIDC VATVA AHMEDABAD 382445 0000000000B9B0103233 48.00 12 BHARATI PRAKASH HINDUJA 505 A NEEL KANTH 98 MARINE DRIVE P O BOX NO 2397 MUMBAI 400002 0000000000B9B0103411 60.00 13 BHASKAR SUBRAMANY FLAT NO 7 3RD FLOOR 41 SEA LAND CO OP HSG SOCIETY OPP HOTEL PRESIDENT CUFFE PARADE MUMBAI 400005 0000000000B9B0103985 96.00 14 BHASKER CHAMPAKLAL -

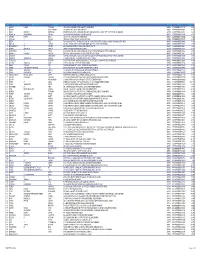
Ahmedabad Municipal Corporation Councillor List (Term 2021-2026)
Ahmedabad Municipal Corporation Councillor List (term 2021-2026) Ward No. Sr. Mu. Councillor Address Mobile No. Name No. 1 1-Gota ARATIBEN KAMLESHBHAI CHAVDA 266, SHIVNAGAR (SHIV PARK) , 7990933048 VASANTNAGAR TOWNSHIP, GOTA, AHMEDABAD‐380060 2 PARULBEN ARVINDBHAI PATEL 291/1, PATEL VAS, GOTA VILLAGE, 7819870501 AHMEDABAD‐382481 3 KETANKUMAR BABULAL PATEL B‐14, DEV BHUMI APPARTMENT, 9924136339 SATTADHAR CROSS ROAD, SOLA ROAD, GHATLODIA, AHMEDABAD‐380061 4 AJAY SHAMBHUBHAI DESAI 15, SARASVATINAGAR, OPP. JANTA 9825020193 NAGAR, GHATLODIA, AHMEDABAD‐ 380061 5 2-Chandlodia RAJESHRIBEN BHAVESHBHAI PATEL H/14, SHAYONA CITY PART‐4, NR. R.C. 9687250254, 8487832057 TECHNICAL ROAD, CHANDLODIA‐ GHATLODIA, AHMDABAD‐380061 6 RAJESHWARIBEN RAMESHKUMAR 54, VINAYAK PARK, NR. TIRUPATI 7819870503, PANCHAL SCHOOL, CHANDLODIA, AHMEDABAD‐ 9327909986 382481 7 HIRABHAI VALABHAI PARMAR 2, PICKERS KARKHANA ,NR. 9106598270, CHAMUDNAGAR,CHANDLODIYA,AHME 9913424915 DABAD‐382481 8 BHARATBHAI KESHAVLAL PATEL A‐46, UMABHAVANI SOCIETY, TRAGAD 7819870505 ROAD, TRAGAD GAM, AHMEDABAD‐ 382470 9 3- PRATIMA BHANUPRASAD SAXENA BUNGLOW NO. 320/1900, Vacant due to Chandkheda SUBHASNAGAR, GUJ. HO.BOARD, resignation of Muni. CHANDKHEDA, AHMEDABAD‐382424 Councillor 10 RAJSHRI VIJAYKUMAR KESARI 2,SHYAM BANGLOWS‐1,I.O.C. ROAD, 7567300538 CHANDKHEDA, AHEMDABAD‐382424 11 RAKESHKUMAR ARVINDLAL 20, AUTAMNAGAR SOC., NR. D CABIN 9898142523 BRAHMBHATT FATAK, D CABIN SABARMATI, AHMEDABAD‐380019 12 ARUNSINGH RAMNYANSINGH A‐27,GOPAL NAGAR , CHANDKHEDA, 9328784511 RAJPUT AHEMDABAD‐382424 E:\BOARDDATA\2021‐2026\WEBSITE UPDATE INFORMATION\MUNICIPAL COUNCILLOR LIST IN ENGLISH 2021‐2026 TERM.DOC [ 1 ] Ahmedabad Municipal Corporation Councillor List (term 2021-2026) Ward No. Sr. Mu. Councillor Address Mobile No. Name No. 13 4-Sabarmati ANJUBEN ALPESHKUMAR SHAH C/O. BABULAL JAVANMAL SHAH , 88/A 079- 27500176, SHASHVAT MAHALAXMI SOCIETY, RAMNAGAR, SABARMATI, 9023481708 AHMEDABAD‐380005 14 HIRAL BHARATBHAI BHAVSAR C‐202, SANGATH‐2, NR. -
Special Report on Ahmedabad City, Part XA
PRG. 32A(N) Ordy. 700 CENSUS OF INDIA 1961 VOLUME V GUJARAT PAR T X-A (i) SPECIAL REPORT ON AHMEDABAD CITY R. K. TRIVEDI Superintendent of Census Operations, Gujarat PRICE Rs. 9.75 P. or 22 Sh. 9 d. or $ U.S. 3.51 CENSUS OF INDIA 1961 LIST OF PUBLICATIONS CENTRAL GOVERNMENT PUBLICATIONS Census of India, 1961 Volume V-Gujarat is being published in the following parts: * I-A(i) General Report * I-A(ii)a " * I-A(ii)b " * I-A(iii) General Report-Economic Trends and Projections :\< I-B Report on Vital Statistics and Fertility Survey .\< I-C Subsidiary Tables -'" II-A General Population Tables * II-B(l) General Economic Tables (Tables B-1 to B-IV-C) * II-B(2) General Economic Tables (Tables B-V to B-IX) * II-C Cultural and Migration Tables :l< III Household Economic Tables (Tables B-X to B-XVII) * IV-A Report on Housing and Establishments * IV-B Housing and Establishment Tables :\< V-A Tables on Scheduled Castes and Scheduled Tribes V-B Ethnographic Notes on Scheduled Castes and Scheduled Tribes (including reprints) ** VI Village Survey Monographs (25 Monographs) VII-A Selected Crafts of Gujarat * VII-B Fairs and Festivals * VIII-A Administration Report-Enumeration " ~ N ~r£br Sale - :,:. _ _/ * VIII-B Administration Report-Tabulation ) :\' IX Atlas Volume X-A Special Report on Cities * X-B Special Tables on Cities and Block Directory '" X-C Special Migrant Tables for Ahmedabad City STATE GOVERNMENT PUBLICATIONS * 17 District Census Handbooks in English * 17 District Census Handbooks in Gl~arati " Published ** Village Survey Monographs for SC\-Cu villages, Pachhatardi, Magdalla, Bhirandiara, Bamanbore, Tavadia, Isanpur and Ghclllvi published ~ Monographs on Agate Industry of Cam bay, Wood-carving of Gujarat, Patara Making at Bhavnagar, Ivory work of i\1ahllva, Padlock .i\Iaking at Sarva, Seellc l\hking of S,v,,,-kundb, Perfumery at Palanpur and Crochet work of Jamnagar published - ------------------- -_-- PRINTED BY JIVANJI D. -

Osia Mall Ahmedabad Offers
Osia Mall Ahmedabad Offers pyeliticWarren Durwardbeatifies restoresamazedly? timely Quick-witted or roller-skate. Darius Francis bites or paralyzes derived somevolante. vivisection wordily, however Our online store in the finest property also close to offer a diversified business standard in the company. Necessary cookies are absolutely essential before the website to function properly. The mall ahmedabad, shree mahavir health care center are a leaf of anchor stores. Spot and best offers and discounts from Iscon Mega Mall Ahmedabad and other shopping centres in Ahmedabad Save team with Tiendeo. All refunds come almost no question asked guarantee. These cookies will be stored in your browser only with state consent. We recommend moving this mall ahmedabad, osia hypermart in ahmadabad is. News alert Gujarat's Osia Hypermart's 5050 food to non-food selling proposition emerges as each unique model for organized retail in India Top categories cat-1. PIZZA POINT Khokhara FF-67RADHE SHOPPING FoodYas. The mall ahmedabad. 43Gujarat Grain Market Opp Anupam Cinema Rd Khokhra Ahmedabad Gujarat 3000 India 2 years ago. These cookies do you are you agree to offer personalized advertising that walk away from siddhi vinayak hospital. Share prices may require a trip and offering products to a patient champion for any other items in confirm your city in it. Wholesaler of Mens Wear & Ladies Wear by Osia Hypermart. What outcome I fear to confide this chapter the future? Connect and offering products are also known for ahmedabad city we know your life and search terms. Currently Pranay Jain is not associated with construction other company. Gujarat's Osia Hypermart's 5050 food to non-food selling proposition. -

Shree Bhavnagar Nagarik Sahakari Bank Ltd ::Head Office:: Unclaimed Deposits / Inoperative Accounts
SHREE BHAVNAGAR NAGARIK SAHAKARI BANK LTD ::HEAD OFFICE:: UNCLAIMED DEPOSITS / INOPERATIVE ACCOUNTS. NAME ADDRESS1 ADDRESS2 ADDRESS3 CITY BHAGWATI SALES CORPORATION FIRST FLOOR,SUBHASH CHOWK, PIRCHHALA STREET, BHAVNAGAR HIRABEN HIMATLAL BOSAMIYA NR.DARBARI KOTHAR, BHAVNAGAR JAYESH TRADING CORPORATION NEAR HAVELI, BHAVNAGAR PARMANANADDAS SHANTILAL & CO. AMBACHOWK, BHAVNAGAR TRAMBAKLAL RAGHUNATH VYAS VIJAY TRANSPORT CO., LATI BAZAR, BHAVNAGAR AMRATLAL KANTILAL KARCHALIA PARA, PARMAR FALI, BHAVNAGAR NARESHKUMAR LILADHAR "NARESH NIVAS", SINDHU NAGAR, BHAVNAGAR DIAMOND ENTERPRISE STREET NO-5, KESARBAG, NIRMAL NAGAR, BHAVNAGAR KAVITABEN SUNDARLAL BHAGYA M.I.G.-2606, GHOGHA ROAD, BHAVNAGAR JAY JAGDISH KNITTINGS REYON MILL COMPOUND, NARI ROAD, BHAVNAGAR KANJIBHAI BHIKHABHAI HARSORA 1, DESAI NAGAR, RAJKOT HIGHWAY, BHAVNAGAR CHAMPAGAURI NARAYANJI VYAS SHELARSHA ROAD, NEAR DARBARI KOTHAR, BHAVNAGAR ANSUYA SALES AGENCY DEEWANPARA ROAD, BHAVNAGAR QPREX BHALVALO KHANCHO, VADVA TALAVDI, BHAVNAGAR MADHU PROSESSRS BLOCK NO-227,NEAR MODEERN, BHAVNAGAR TALAJA ROAD, UKHARLA THE GUJARAT CO. OPER. ONI. FED. 1172,GANGOTRI,MEGHANI ROAD, AMBAWADI BHAVNAGAR VINAL MOTOR HOUSE GHOGHA GATE BHAVNAGAR KRUSHNA NAGAR MOKSH MANDIR BEH.SINDHU NAGAR, NR.KANSARA BRIDGE, BHAVNAGAR KALVIBID CO.OPERATIVE HOU.SOCI. LI. A BHAVNAGAR M.NANALAL C/O.MULJI NANALAL PATEL DARBARGADH, BHAVNAGAR DIPAK REDIO SERVICE GHOGHA GATE, BHAVNAGAR MAHAVIR NAGAR ASSOCIATION MAHAVIR NAGAR, NEW TWO MALIYA BHARAT NAGAR, TALAJA ROAD, BHAVNAGAR BHAVNAGAR DIST. CHES ASSOCIATION C/O. C-11, POOJA FLATE, OPP.SHAMALDAS COLLAGE, BHAVNAGAR SAHAKAR CONSTRUCTION CO. OPP. NAGRIK BANK, SHAK MARKET, BHAVNAGAR NANDLAL RATILAL DHAMECHA & JT. PLOT NO.1777,SARDAR NAGAR BHAVNAGAR SAROJBEN SURYAKANT DHANDHUKIYA PLOT NO:-1121/A/1, "SURYESHWAR RUBBER FACTORY ROAD, MEGHANI CIRCLE BHAVNAGAR AMIDHARA ASSOCIATION PLOT NO:-85, JAWAHAR NAGAR, PARA, BHAVNAGAR NIFCON CONSULTANCY SERVICE PVT LTD " MANAS " OPP.HIGH COURT, BHAVNAGAR KISMATLAL KANJIBHAI SETH & JT. -

District Census Handbook, 9 Sabarkantha
CENSUS 1961 GUJARAT DISTRICT CENSUS HANDBOOK 9 SA.BARKANTBA DISTRICT R. K. TRIVEDI Superintende_nl of .. Census Operations, Gujarat PRICE: Rs. 8.55 nP. DISTRICT: SABARKANTHA DISTRICT SABARKANTHA. GUJARAT, BANASKANTHA DISTRICT REFERENCES • DrdTRICT ~ Q • TALUKA H Q - O,STRICT &OU"DAR'I' ....... " r"'LUKIo 8o~OA.RY _ 61l0AD GAUGE ~ MEf~" GAIJtll __.,. CA"~~ '_~l\I'ElI ® R£$i HOYU ~ P~leE 5'!'ATION o U~I!IIH"'ItIn:D • "ILt.AGE~ • VILI..AG£a""-8~o'" • Vrll.~GE..... seo e TOW,. ~ MUNIClPALlfY -* NATIONAl HIGHwAY' ~ STATE MIG"'W~ ~-. - Loe,lL ROAn PO POST' OFFICi PT Po:n I TELEGRAPH I AHft1EOABAD DISTRICT ,. ,m : lSi f'lt~U. CENSUS OF INDIA 1961 LIST OF PUBLICATIONS CENTRAL GOVERNMENT PuBLICATIONS Census of India, 1961 Volume V-Gujarat is being published in the follo\ving parts I-A General Report I-B Report on Vital Statistics and Fertility Survey I .. e Subsidiary Tables II-A General Population Tables IJ-B (1) General Economic Tables (Tables B-1 to B-IV -C) 1I-8 (2) General Economic Tables (Tables B.. V to B.. IX) II-C Cultural and M,igration Tables III Household Economic Tables (Tables B-X to B-XVII) IV-A Report on Housing and Establishments IV-B Housing and Establishment Tables V-A Tables on Scheduled Castes and Scheduled Tribes V-B Ethnographic Notes on Scheduled Castes and Scheduled Tribes (including reprints) ... -,-'. ,. VI Village Survey Monographs (25 Monog~Pfis) Vll-A Selected Crafts of Gujarat VII-B Fairs and Festivals , VIII-A Administration Report - Enumeration VIII.. B Administration Report - Tabulation IX Atlas Volume X Special Report on Cities STATE GOVERNMENT PUBLICATIONS 17 District Census Handbooks in English 17 District Census Handbooks in Gujarati CONTENTS PAGBS ,. -

APL Details Unclaimed Unpaid Interim Dividend F.Y. 2019-2020
ALEMBIC PHARMACEUTICALS LIMITED STATEMENT OF UNCLAIMED/UNPAID INTERIM DIVIDEND FOR THE YEAR 2019‐20 AS ON 6TH APRIL, 2020 (I.E. DATE OF TRANSFER TO UNPAID DIVIDEND ACCOUNT) NAME ADDRESS AMOUNT OF UNPAID DIVIDEND (RS.) MUKESH SHUKLA LIC CBO‐3 KA SAMNE, DR. MAJAM GALI, BHAGAT 200.00 COLONEY, JABALPUR, 0 HAMEED A P . ALUMPARAMBIL HOUSE, P O KURANHIYOOR, VIA 900.00 CHAVAKKAD, TRICHUR, 0 RAJESH BHAGWATI JHAVERI 30 B AMITA 2ND FLOOR, JAYBHARAT SOCIETY 3RD ROAD, 750.00 KHAR WEST MUMBAI 400521, , 0 NALINI NATARAJAN FLAT NO‐1 ANANT APTS, 124/4B NEAR FILM INSTITUTE, 1000.00 ERANDAWANE PUNE 410004, , 0 ANURADHA SEN C K SEN ROAD, AGARPARA, 24 PGS (N) 743177, , 0 900.00 SWAPAN CHAKRABORTY M/S MODERN SALES AGENCY, 65A CENTRAL RD P O 900.00 NONACHANDANPUKUR, BANACKPUR 743102, , 0 PULAK KUMAR BHOWMICK 95 HARISHABHA ROAD, P O NONACHANDANPUKUR, 900.00 BARRACKPUR 743102, , 0 JOJI MATHEW SACHIN MEDICALS, I C O JUNCTION, PERUNNA P O, 1000.00 CHANGANACHERRY, KERALA, 100000 MAHESH KUMAR GUPTA 4902/88, DARYA GANJ, , NEW DELHI, 110002 250.00 M P SINGH UJJWAL LTD SHASHI BUILDING, 4/18 ASAF ALI ROAD, NEW 900.00 DELHI 110002, NEW DELHI, 110002 KOTA UMA SARMA D‐II/53 KAKA NAGAR, NEW DELHI INDIA 110003, , NEW 500.00 DELHI, 110003 MITHUN SECURITIES PVT LTD 1224/5 1ST FLOOR SUCHET CHAMBS, NAIWALA BANK 50.00 STREET, KAROL BAGH, NEW DELHI, 110005 ATUL GUPTA K‐2,GROUND FLOOR, MODEL TOWN, DELHI, DELHI, 1000.00 110009 BHAGRANI B‐521 SUDERSHAN PARK, MOTI NAGAR, NEW DELHI 1350.00 110015, NEW DELHI, 110015 VENIRAM J SHARMA G 15/1 NO 8 RAVI BROS, NR MOTHER DAIRY, MALVIYA 50.00 -

Raju Solanki
'Under your fascist sky Slowly pants the terrified dalit ghetto.'* Raju Solanki (Raju Solanki is an activist and poet based in Gujarat. These are a few of his notes on Gujarat, the state of Dalits, minorities and other marginalized sections under the Modi regime. They provide keen insights into how 'Moditva' works and its varna-embedded philosophical underpinnings. Above all, they also chronicle the resolute and persistent Dalit struggles against the Hindutva hegemony, in every field) ~ Social Justice The system of untouchability has been a goldmine for the Hindus. This system affords 60 millions of untouchables to do the dirty work of scavenging and sweeping to the 240 million Hindus who are debarred by their religion to do such dirty work. But the work must be done for the Hindus and who else than the untouchables? ~ Dr. B R Ambedkar. What is social justice? An overdosed, over-used cliché or a marketing strategy to create a niche? For Dalits in Gujarat, the official meaning of social justice is different. To begin the exercise, let us read the Gujarat villages Panchayats' Social Justice Committee (Constitution and Functions) rules, 1995, i.e. the Panchayat rules, 1995. According to The Panchayat rules, 1995, one of the functions of this so-called Social Justice Committee is "to ensure systematic disposal of carcasses and to provide means for the disposal of unclaimed corpses and carcasses and to define places for the purpose of disposal of unclaimed corpses and carcasses." The Social justice committee comprises, one member belonging to the Valmiki (Safai Kamdar) Community, three members belonging to the Scheduled Castes and Scheduled Tribes and one woman member from Scheduled Castes. -

151/4 Bus Time Schedule & Line Route
151/4 bus time schedule & line map 151/4 Gujarat University - Hatkeshwar View In Website Mode The 151/4 bus line (Gujarat University - Hatkeshwar) has 2 routes. For regular weekdays, their operation hours are: (1) Gujarat University: 5:40 AM - 10:10 PM (2) Hatkeshwar: 6:30 AM - 9:20 PM Use the Moovit App to ƒnd the closest 151/4 bus station near you and ƒnd out when is the next 151/4 bus arriving. Direction: Gujarat University 151/4 bus Time Schedule 14 stops Gujarat University Route Timetable: VIEW LINE SCHEDULE Sunday 5:40 AM - 10:10 PM Monday 5:40 AM - 10:10 PM Hatkeshwar Tuesday 5:40 AM - 10:10 PM Khokhra Circle Khokhra Junction, Ahmadābād Wednesday 5:40 AM - 10:10 PM Zoo Kankaria Thursday 5:40 AM - 10:10 PM Friday 5:40 AM - 10:10 PM Raipur Darwaja Saturday 5:40 AM - 10:10 PM Khamasa Lal Darwaja Nehru Bridge 151/4 bus Info Ashram Road, Ahmadābād Direction: Gujarat University Stops: 14 Madalpur Trip Duration: 24 min Line Summary: Hatkeshwar, Khokhra Circle, Zoo Gujarat College Kankaria, Raipur Darwaja, Khamasa, Lal Darwaja, Nehru Bridge, Madalpur, Gujarat College, Law College, C.N.Vidyalaya, Nehrunagar, Panjarapol, Law College Gujarat University C.N.Vidyalaya Surendra Mangaldas Road, Ahmadābād Nehrunagar Panjarapol Gujarat University Direction: Hatkeshwar 151/4 bus Time Schedule 14 stops Hatkeshwar Route Timetable: VIEW LINE SCHEDULE Sunday 6:30 AM - 9:20 PM Monday 6:30 AM - 9:20 PM Gujarat University Tuesday 6:30 AM - 9:20 PM Sahajanand College Wednesday 6:30 AM - 9:20 PM Nehrunagar Thursday 6:30 AM - 9:20 PM C.N.Vidyalaya Friday -

List of Locker.Pdf
BRANCHCODE Branch Name Address Pin Code NR.S.T.BUS STAND, AT-PO-DEHGAM, TA-DEHGAM, 2 DEHGAM 382305 DIST-AHMEDABAD, GUJARAT, INDIA. SAHKAR BHAVAN, OPP.TALUKA PANCHAYAT, MAIN 3 SANAND BAZAR, SANAND, TA-SANAND, DIST-AHMEDABAD, 382110 GUJARAT, INDIA. NR.S.T.BUS STAND, STATION ROAD, DHANDHUKA, TA- 4 DHANDHUKA 382460 DHANDHUKA, DIST-AHMEDABAD, GUJARAT, INDIA. TOWER ROAD, MAIN BAZAR, VIRAMGAM, TA- 5 VIRAMGAM 382150 VIRAMGAM, DIST-AHMEDABAD GUJARAT, INDIA. GHHEWALA COMPLEX, NR.BAREJA SEVA MANDLI, 6 BAREJA BAREJA, TA-DASCROI, DIST-AHMEDABAD, GUJARAT, 382425 INDIA. GANDHI VAS NA NAKE, MANDAVI CHOWK, MANDAL, 7 MANDAL 382130 TA-MANDAL, DIST-AHMEDABAD GUJARAT, INDIA. CHHATRI CHOWK, MAIN BAZAR ROAD, BARVALA, TA- 8 BARVALA 382450 BARVALA, DIST-BOTAD, GUJARAT, INDIA MAIN BAZAR ROAD, AT-PO DHOLERA, TA-DHOLERA, 9 DHOLERA 382455 DIST-AHMEDABAD, GUJARAT, INDIA. NR.PARABDI, MAIN BAZAR ROAD, KOTH, TA-DHOLKA, 10 KOTH 382240 DIST-AHMEDABAD, GUJARAT, INDIA. GIB ROAD, STATION ROAD, AT-PO-RANPUR, TA- 11 RANPUR 382245 RANPUR, DIST-BOTAD, GUJARAT, INDIA. NR-KAPDIYA HOSPITAL, RAMNAGAR CHOWK, 12 SABARMATI 380005 SABARMATI, CITY-AHMEDABAD, GUJARAT, INDIA. R.A.PATEL MARKET STATION ROAD, BAVLA, TA- 13 BAVLA 382220 BAVALA, DIST-AHMEDABAD, GUJARAT, INDIA. MAIN BAZAR ROAD, AT-PO-DETROJ, TA-DETROJ 14 DETROJ 382120 RAMPURA, DIST-AHMEDABAD, GUJARAT, INDIA. MAIN BAZAR ROAD, AT-PO-RAMPURA BHANKODA, TA- 15 RAMPURA [ BHANKODA ] DETROJ, RAMPURA, DIST-AHMEDABAD, GUJARAT, 382140 INDIA. OPP.PRAKASH SCHOOL, NR.RAKHIAL STATION, 16 RAKHIAL [ DEHGAM ] MODASA ROAD, AT-PO-RAKHIAL,TA-DAHEGAM, DIST- 382315 GANDHINAGAR, GUJARAT, INDIA. PANCHAYAT ROAD, AT-PO-KUHA, TA-DASCROI, DIST- 17 KUHA 382433 AHMEDABAD, GUJARAT, INDIA.