The Challenges of Delivering Continuing Care in First Nations Communities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Annual Report
Treaty 8 First Nations of Alberta 18178 - 102 Ave., Edmonton, Alberta T5S 1S7 2012-2013 T: 780-444-9366 F: 780-484-1465 www.treaty8.ca Annual Report Treaty 8 First Nations of Alberta Report prepared by Victor Horseman Treaty 8 Nations of Alberta 24 First Nations in Treaty No. 8 (Alberta) Athabasca Chipewyan Loon River First Nation First Nation Lubicon Lake Band Beaver First Nation Mikisew Cree First Nation Bigstone Cree Nation Peerless Trout First Nation Chipewyan Prairie First Nation Dene Tha’ First Nation Sawridge First Nation Driftpile Cree Nation Sturgeon Lake Cree Nation Duncan’s First Nation Smith’s Landing First Nation Fort McKay First Nation Sucker Creek First Nation Fort McMurray First Nation Swan River First Nation Horse Lake First Nation Tallcree Tribal Government Kapawe’no First Nation Whitefish Lake First Nation Little Red River Cree Woodland Cree First Nation First Nation CONTENTS Message from The Grand Chief 2 Message from The Chief Operating Officer 4 Intergovernmental Initiatives 6 Treaty Relations 10 Livelihood 15 Education 20 Health 29 Children’s Agenda 34 Message from The Grand Chief Grand Chief Roland Twinn When I was elected as Grand Chief for Treaty 8 First Nations of Alberta I was honored with a drum song which was sung by Chief Leslie Joe Laboucan! The beat of the drum and his powerful voice echoed throughout the gymnasium. The people of Treaty 8 then lined to congratulate me and the Chiefs gave extended words of encouragement. Elders, Chiefs, ladies and gentlemen, it’s been an honour to have served as the Grand Chief, it’s been quite the experience and humbling. -
Debates of the House of Commons
43rd PARLIAMENT, 1st SESSION House of Commons Debates Official Report (Hansard) VOLUME 149 NUMBER 010 Wednesday, January 29, 2020 Speaker: The Honourable Anthony Rota CONTENTS (Table of Contents appears at back of this issue.) 623 HOUSE OF COMMONS Wednesday, January 29, 2020 The House met at 2 p.m. UKRAINE INTERNATIONAL AIRLINES FLIGHT PS752 Mr. Kerry Diotte (Edmonton Griesbach, CPC): Mr. Speaker, I want to commemorate the victims of Ukraine International Airlines Prayer flight PS752. One hundred and seventy-six innocent people lost their lives ● (1405) when this plane was shot down by the Iranian military. Fifty-seven [Translation] were Canadians; of those, 13 were Edmontonians. The Speaker: It being Wednesday, we will now have the singing Loved ones of these victims deserve immediate answers. Howev‐ of the national anthem, led by the member for Charlesbourg— er, their grief has been compounded because they are not getting Haute-Saint-Charles. those answers. Instead, they have suffered through a cover-up since day one. [Members sang the national anthem] Iranian authorities must be transparent and fully co-operate with independent agencies investigating this horrific event. Families also deserve that the remains of their loved ones are allowed to be repa‐ STATEMENTS BY MEMBERS triated to Canada as soon as possible. Anything less is completely unacceptable. These loved ones have suffered enough. [English] * * * INTERNATIONAL HOLOCAUST REMEMBRANCE DAY TAMIL HERITAGE MONTH Mr. Michael Levitt (York Centre, Lib.): Mr. Speaker, this past Monday was International Holocaust Remembrance Day, when we Ms. Jennifer O'Connell (Pickering—Uxbridge, Lib.): Mr. remembered the murder of over six million Jews during World War Speaker, four years ago, the House unanimously approved Motion II. -

National Women's Liberal Commission Our Politics - Our Future
2005 Biennial Convention Liberal Party of Canada NATIONAL WOMEN'S LIBERAL COMMISSION OUR POLITICS - OUR FUTURE THURSDAY, MARCH 3, 2005 WESTIN HOTEL, OTTAWA I am delighted to extend my warmest greetings to you on the occasion of the Liberal Party of Canada’s 2005 Biennial Policy Convention in Ottawa from March 3 to 6, 2005. As Leader of the Liberal Party, I am tremendously proud to see so many Liberal Women in attendance, and am grateful for the enthusiasm and ability you will bring to this event. Indeed, I am proud to say that we have accomplished much of what we have set out to do, and our progress has been more than impressive. In fact, we have asserted our country’s role on the international stage, increased transparency and accountability, signed a historic Health Accord with the provinces and presented a clear picture of the Canada we envision for the future. One can measure our Party’s success by the devotion of individuals, such as yourselves, and we are very thankful to have such a wonderful group of dedicated women working for the betterment of our country. You can all take great pride in having upheld our Party’s principles, while contributing to the advancement of the political initiatives on behalf of all women in Canada. I look forward to joining you and discussing our objectives while renewing several ties of friendship with many members and organizers present. Please accept my warmest regards and best wishes for a most productive and exciting Convention. Le très honorable Paul Martin Chef du Parti libéral du Canada O T T A W A The Right Honourable Paul Martin, P.C., M.P. -
Core 1..48 Committee
Standing Committee on Fisheries and Oceans FOPO Ï NUMBER 119 Ï 1st SESSION Ï 42nd PARLIAMENT EVIDENCE Thursday, November 8, 2018 Chair Mr. Ken McDonald 1 Standing Committee on Fisheries and Oceans Thursday, November 8, 2018 The NunatuKavut Community Council is the representative government of approximately 6,000 southern Inuit who belong to (1105) Ï this territory. Do you see this lady here? People ask, “Why do you [English] put her there?” Women are strong in our culture. They're the culture The Chair (Mr. Ken McDonald (Avalon, Lib.)): Good morning, carriers. This is a woman who was obviously the head of her everyone. household. In our tradition, she would be fishing and she would probably do a little bit of hunting at the same time, providing for her Pursuant to Standing Order 108(2), we are doing a study of the family, and in some regards, for her community. That's what we want current state of the Department of Fisheries and Oceans' small craft to do as a government—provide for our community. harbours. I'd like to welcome our guests this morning. By video conference, We have a vision to be self-governing. We will provide and care we have Mr. Alex Patterson from the community services and for one another, our families and communities, while nurturing our tourism division of the Municipality of Wawa. Here in person, from relationship with our land, ice and waters. We try to keep that vision the NunatuKavut Community Council, we have the president, Todd firmly in front of us as we do our work on behalf of our people. -
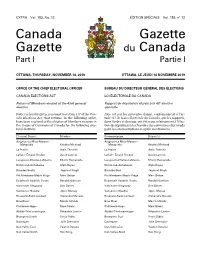
Canada Gazette, Part I
EXTRA Vol. 153, No. 12 ÉDITION SPÉCIALE Vol. 153, no 12 Canada Gazette Gazette du Canada Part I Partie I OTTAWA, THURSDAY, NOVEMBER 14, 2019 OTTAWA, LE JEUDI 14 NOVEMBRE 2019 OFFICE OF THE CHIEF ELECTORAL OFFICER BUREAU DU DIRECTEUR GÉNÉRAL DES ÉLECTIONS CANADA ELECTIONS ACT LOI ÉLECTORALE DU CANADA Return of Members elected at the 43rd general Rapport de député(e)s élu(e)s à la 43e élection election générale Notice is hereby given, pursuant to section 317 of the Can- Avis est par les présentes donné, conformément à l’ar- ada Elections Act, that returns, in the following order, ticle 317 de la Loi électorale du Canada, que les rapports, have been received of the election of Members to serve in dans l’ordre ci-dessous, ont été reçus relativement à l’élec- the House of Commons of Canada for the following elec- tion de député(e)s à la Chambre des communes du Canada toral districts: pour les circonscriptions ci-après mentionnées : Electoral District Member Circonscription Député(e) Avignon–La Mitis–Matane– Avignon–La Mitis–Matane– Matapédia Kristina Michaud Matapédia Kristina Michaud La Prairie Alain Therrien La Prairie Alain Therrien LaSalle–Émard–Verdun David Lametti LaSalle–Émard–Verdun David Lametti Longueuil–Charles-LeMoyne Sherry Romanado Longueuil–Charles-LeMoyne Sherry Romanado Richmond–Arthabaska Alain Rayes Richmond–Arthabaska Alain Rayes Burnaby South Jagmeet Singh Burnaby-Sud Jagmeet Singh Pitt Meadows–Maple Ridge Marc Dalton Pitt Meadows–Maple Ridge Marc Dalton Esquimalt–Saanich–Sooke Randall Garrison Esquimalt–Saanich–Sooke -

Core 1..16 Journalweekly (PRISM::Advent3b2 17.25)
HOUSE OF COMMONS OF CANADA CHAMBRE DES COMMUNES DU CANADA 42nd PARLIAMENT, 1st SESSION 42e LÉGISLATURE, 1re SESSION Journals Journaux No. 22 No 22 Monday, February 22, 2016 Le lundi 22 février 2016 11:00 a.m. 11 heures PRAYER PRIÈRE GOVERNMENT ORDERS ORDRES ÉMANANT DU GOUVERNEMENT The House resumed consideration of the motion of Mr. Trudeau La Chambre reprend l'étude de la motion de M. Trudeau (Prime Minister), seconded by Mr. LeBlanc (Leader of the (premier ministre), appuyé par M. LeBlanc (leader du Government in the House of Commons), — That the House gouvernement à la Chambre des communes), — Que la Chambre support the government’s decision to broaden, improve, and appuie la décision du gouvernement d’élargir, d’améliorer et de redefine our contribution to the effort to combat ISIL by better redéfinir notre contribution à l’effort pour lutter contre l’EIIL en leveraging Canadian expertise while complementing the work of exploitant mieux l’expertise canadienne, tout en travaillant en our coalition partners to ensure maximum effect, including: complémentarité avec nos partenaires de la coalition afin d’obtenir un effet optimal, y compris : (a) refocusing our military contribution by expanding the a) en recentrant notre contribution militaire, et ce, en advise and assist mission of the Canadian Armed Forces (CAF) in développant la mission de conseil et d’assistance des Forces Iraq, significantly increasing intelligence capabilities in Iraq and armées canadiennes (FAC) en Irak, en augmentant theatre-wide, deploying CAF medical personnel, -

A Parliamentarian's
A Parliamentarian’s Year in Review 2018 Table of Contents 3 Message from Chris Dendys, RESULTS Canada Executive Director 4 Raising Awareness in Parliament 4 World Tuberculosis Day 5 World Immunization Week 5 Global Health Caucus on HIV/AIDS, Tuberculosis and Malaria 6 UN High-Level Meeting on Tuberculosis 7 World Polio Day 8 Foodies That Give A Fork 8 The Rush to Flush: World Toilet Day on the Hill 9 World Toilet Day on the Hill Meetings with Tia Bhatia 9 Top Tweet 10 Forging Global Partnerships, Networks and Connections 10 Global Nutrition Leadership 10 G7: 2018 Charlevoix 11 G7: The Whistler Declaration on Unlocking the Power of Adolescent Girls in Sustainable Development 11 Global TB Caucus 12 Parliamentary Delegation 12 Educational Delegation to Kenya 14 Hearing From Canadians 14 Citizen Advocates 18 RESULTS Canada Conference 19 RESULTS Canada Advocacy Day on the Hill 21 Engagement with the Leaders of Tomorrow 22 United Nations High-Level Meeting on Tuberculosis 23 Pre-Budget Consultations Message from Chris Dendys, RESULTS Canada Executive Director “RESULTS Canada’s mission is to create the political will to end extreme poverty and we made phenomenal progress this year. A Parliamentarian’s Year in Review with RESULTS Canada is a reminder of all the actions decision makers take to raise their voice on global poverty issues. Thank you to all the Members of Parliament and Senators that continue to advocate for a world where everyone, no matter where they were born, has access to the health, education and the opportunities they need to thrive. “ 3 Raising Awareness in Parliament World Tuberculosis Day World Tuberculosis Day We want to thank MP Ziad Aboultaif, Edmonton MPs Dean Allison, Niagara West, Brenda Shanahan, – Manning, for making a statement in the House, Châteauguay—Lacolle and Senator Mobina Jaffer draw calling on Canada and the world to commit to ending attention to the global tuberculosis epidemic in a co- tuberculosis, the world’s leading infectious killer. -

List of Mps on the Hill Names Political Affiliation Constituency
List of MPs on the Hill Names Political Affiliation Constituency Adam Vaughan Liberal Spadina – Fort York, ON Alaina Lockhart Liberal Fundy Royal, NB Ali Ehsassi Liberal Willowdale, ON Alistair MacGregor NDP Cowichan – Malahat – Langford, BC Anthony Housefather Liberal Mount Royal, BC Arnold Viersen Conservative Peace River – Westlock, AB Bill Casey Liberal Cumberland Colchester, NS Bob Benzen Conservative Calgary Heritage, AB Bob Zimmer Conservative Prince George – Peace River – Northern Rockies, BC Carol Hughes NDP Algoma – Manitoulin – Kapuskasing, ON Cathay Wagantall Conservative Yorkton – Melville, SK Cathy McLeod Conservative Kamloops – Thompson – Cariboo, BC Celina Ceasar-Chavannes Liberal Whitby, ON Cheryl Gallant Conservative Renfrew – Nipissing – Pembroke, ON Chris Bittle Liberal St. Catharines, ON Christine Moore NDP Abitibi – Témiscamingue, QC Dan Ruimy Liberal Pitt Meadows – Maple Ridge, BC Dan Van Kesteren Conservative Chatham-Kent – Leamington, ON Dan Vandal Liberal Saint Boniface – Saint Vital, MB Daniel Blaikie NDP Elmwood – Transcona, MB Darrell Samson Liberal Sackville – Preston – Chezzetcook, NS Darren Fisher Liberal Darthmouth – Cole Harbour, NS David Anderson Conservative Cypress Hills – Grasslands, SK David Christopherson NDP Hamilton Centre, ON David Graham Liberal Laurentides – Labelle, QC David Sweet Conservative Flamborough – Glanbrook, ON David Tilson Conservative Dufferin – Caledon, ON David Yurdiga Conservative Fort McMurray – Cold Lake, AB Deborah Schulte Liberal King – Vaughan, ON Earl Dreeshen Conservative -

Metis Settlements and First Nations in Alberta Community Profiles
For additional copies of the Community Profiles, please contact: Indigenous Relations First Nations and Metis Relations 10155 – 102 Street NW Edmonton, Alberta T5J 4G8 Phone: 780-644-4989 Fax: 780-415-9548 Website: www.indigenous.alberta.ca To call toll-free from anywhere in Alberta, dial 310-0000. To request that an organization be added or deleted or to update information, please fill out the Guide Update Form included in the publication and send it to Indigenous Relations. You may also complete and submit this form online. Go to www.indigenous.alberta.ca and look under Resources for the correct link. This publication is also available online as a PDF document at www.indigenous.alberta.ca. The Resources section of the website also provides links to the other Ministry publications. ISBN 978-0-7785-9870-7 PRINT ISBN 978-0-7785-9871-8 WEB ISSN 1925-5195 PRINT ISSN 1925-5209 WEB Introductory Note The Metis Settlements and First Nations in Alberta: Community Profiles provide a general overview of the eight Metis Settlements and 48 First Nations in Alberta. Included is information on population, land base, location and community contacts as well as Quick Facts on Metis Settlements and First Nations. The Community Profiles are compiled and published by the Ministry of Indigenous Relations to enhance awareness and strengthen relationships with Indigenous people and their communities. Readers who are interested in learning more about a specific community are encouraged to contact the community directly for more detailed information. Many communities have websites that provide relevant historical information and other background. -

Annual Report 2020
Annual Report 2020 FERTILIZERCANADA.CA Table of Contents 01 Who We Are 02 Message from the Chair 04 Message from the President 06 Advocacy and Communications 16 Policy and Regulatory Affairs 19 Safety and Security 22 Stewardship – 4R’s 33 Members and Partners 34 Leadership and Staff 907 – 350 Sparks, Ottawa ON K1R 7S8 @FertilizerCA T (613) 230-2600 | [email protected] fertilizercanada.ca FERTILIZER CANADA Who We Are Fertilizer Canada represents manufacturers, wholesale and retail distributors of nitrogen, phosphate, potash and sulphur fertilizers. The fertilizer industry plays an essential role in Canada’s economy, contributing over $23 billion annually and employing 76,000 workers throughout the supply chain. In order to remain globally competitive, we are committed to supporting our industry with innovative research and programming. We take pride in advocating for sustainability, stewardship, safety and security through our industry- leading standards and Codes of Practice. As the foundation of Canada’s agri-food sector, we apply innovative solutions that positively impact the environment, the economy, and the social fabrics of Canadian life. ECONOMIC GDP JOBS WAGES IMPACT $23.6B $12.7B 76,830 $5.1B $10B $4.5B 28,933 $1.9B $7B $4.6B 15,128 $1.2B $1.8B $878.2M 7,451 $475.1M $1.6B $881.7M 8,440 $490M $3.2B $1.8B 16,878 $980M MANUFACTURING MINING & PROCESSING TRANSPORT & STORAGE WHOLESALE RETAIL 1 ANNUAL REPORT 2020 Message from the Chair As Chair of Fertilizer Canada’s Board of Directors, I am proud to be playing an active role in the Canadian agriculture sector to help the fertilizer industry achieve its economic, social, and environmental goals in both Canada and around the world. -

Lib2021 • Program
LIB2021 • PROGRAM From April 8-10, Canadians from coast to coast to coast are joining Justin Trudeau and our Liberal team for our 2021 Liberal National Convention, featuring special keynote panels and speakers, virtual policy discussions, innovating campaign training, and much more. Thursday Sessions Time Session Type Speakers Convention 7:00 PM Opening and Welcome Business Keynote 7:25 PM President’s Opening Remarks Remarks • Suzanne Cowan Supporting Canadians, and building Keynote 7:55 PM a real and fair chance to succeed: Remarks • Hon. Ahmed Hussen Remarks by the Hon. Ahmed Hussen Shaping our future for the Keynote 8:30 PM better: Remarks by the Remarks • Hon. Steven Guilbeault Hon. Steven Guilbeault A Better, Stronger, and More Resilient Canada: In Conversation with the Keynote • Hon. Chrystia Freeland 8:50 PM Hon. Chrystia Freeland and Conversation • Hon. Ken Dryden the Hon. Ken Dryden Subject to change and confirmation | All times EDT 1 Updated as of 1 PM / Saturday / 10/04/2021 - Latest program updates at Lib2021.ca/program Friday Sessions Time Session Type Speakers Convention • Mira Ahmad 10:00 AM Convention 101 Business • Élise Bartlett • Hon. Carolyn Bennett • Hon. Marc Miller 10:00 AM Indigenous Peoples’ Commission Commission • Jaime Battiste • Suzanne Cowan Organizing 11:00 AM Safe and Inclusive Campaigns • Jess Spindler & Readiness 11:00 AM Senior Liberals’ Commission Commission • Stéphane Lauzon • Suzanne Cowan • Hon. Carla Qualtrough 11:00 AM Young Liberals of Canada Commission • Hon. Bardish Chagger • Hon. Karina Gould • Nathaniel Erskine-Smith National Women’s 12:00 PM Commission • Suzanne Cowan Liberal Commission Official Convention Convention 12:30 PM Business Opening Business • Hon. -

63 Priority Districts for 2019
63 Priority Districts for 2019 These Federal Electoral Districts were the ones in which the 2016 Census Population of First Nations 18+ was either: a) larger than the margin of victory in the 2015 federal election b) within 5% of the margin of victory and at least 1% of the total vote eligible population in the district Legend Underline indicates previous winner (If only the party is underlined the incumbent is not running) Bold Candidates Indicates a First Nations Candidate FN 18+ = Total number of First Nations Eligible Voters MOV = Margin of Victory in total votes in 2015 1 Alberta (Five Districts) 5. Edmonton Mill Woods (Click for Map of District) 1. Calgary Confederation (Click for Map of District) Candidates: Candidates: CPC Tim Uppal GRN Tanya Herbert CPC Len Webber LIB Amarjeet Sohi GRN Natalie AM Odd NDP Nigel Logan LIB Jordan Stein PPC Annie Young NDP Gurcharan Sidhu[ PPC Colin C. Korol FN 18+: 1230 MOV: 92 FN 18+: 1095 MOV: 1586 2. Calgary Centre (Click for Map of District) Candidates: CPC Gary McLean GRN Thana Boolert LIB Kent Hehr NDP essica Buresi PPC Chevy Johnston FN 18+: 1110 MOV: 750 3. Edmonton Centre (Click for Map of District) Candidates: CPC James Cumming GRN Grad Murray LIB Randy Boissonnault NDP Katherine Swampy PPC Paul J. Hookham FN 18+: 2800 MOV: 1199 4. Edmonton Griesbach (Click for Map of District) Candidates: CPC Kerry Diotte GRN Safi Khan LIB Habiba Mohamud NDP Mark W.J. Cherington PPC Barbara Nichols FN 18+: 3465 MOV: 2848 2 British Columbia (15 Districts) 1. Burnaby South (Click for Map of District) 5.