Evaluating Patient Outcomes When Adding Licensed Practical Nurses to the Staffing Mix Isabel C.M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Facts About the Shortage of Nurses in Virginia
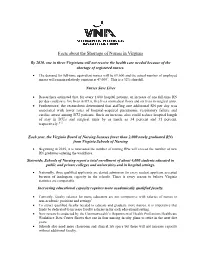
Facts about the Shortage of Nurses in Virginia By 2020, one in three Virginians will not receive the health care needed because of the shortage of registered nurses. • The demand for full-time equivalent nurses will be 69,600 and the actual number of employed nurses will remain relatively constant at 47,0001. This is a 32% shortfall. Nurses Save Lives • Researchers estimated that, for every 1,000 hospital patients, an increase of one full-time RN per day could save five lives in ICUs, five lives on medical floors and six lives in surgical units. • Furthermore, the researchers determined that staffing one additional RN per day was associated with lower rates of hospital-acquired pneumonia, respiratory failure and cardiac arrest among ICU patients. Such an increase also could reduce hospital length of stay in ICUs and surgical units by as much as 34 percent and 31 percent, respectively." 2 Each year, the Virginia Board of Nursing licenses fewer than 2,000 newly graduated RNs from Virginia Schools of Nursing • Beginning in 2015, it is forecasted the number of retiring RNs will exceed the number of new RN graduates entering the workforce. Statewide, Schools of Nursing report a total enrollment of about 6,000 students educated in public and private colleges and universities and in hospital settings. • Nationally, three qualified applicants are denied admission for every student applicant accepted because of inadequate capacity in the schools. There is every reason to believe Virginia statistics are comparable. Increasing educational capacity requires more academically qualified faculty. • Currently, faculty salaries for nurse educators are not competitive with salaries of nurses in non-academic positions and settings3. -

Nursing Research: Challenges
NURSING RESEARCH: CHALLENGES AND OPPORTUNITIES PRESENTED BY OPARA HOPE CHIZOLUM AT GLOBAL RESEARCH NURSES WORKSHOP 24th and 25th May 2021 NNAMDI AZIKIWE UNIVERSITY TEACHING HOSPITAL, NNEWI OUTLINE FOR THE PRESENTATION INTRODUCTION WHAT IS NURSING RESEARCH? IMPORTANCE OF RESEARCH TO NURSING WHAT ARE THE OPPORTUNITIES? CHALLENGES FACED BY NURSE RESEARCHERS WAY FORWARD CONCLUSION INTRODUCTION Research is a way of thinking: examining critically the various aspects of your day-to-day work; understanding and formulating guiding principles that govern a procedure; and developing and, testing new theories that contribute to the advancement of your practice and profession (Odunze, 2019). It is a habit of questioning what you do, and a systematic examination of clinical observations to explain and find answers for what you perceive, with a view to instituting appropriate changes for a more effective professional service (Kumar et al, 2016) Today’s healthcare system is complex, and patients have increasingly varied needs. Developing solutions for the health issues of diverse populations requires providers with many different perspectives (National Institute of Nursing Research, 2016). Nurses provide direct care to their patients on a daily basis, so they know which approaches work well and which need adjusting. Nursing concerns are the heart of nursing research. even when nurses want to improve care through research findings, several barriers have hindered the progress. WHAT IS NURSING RESEARCH? Nursing research is research that provides a body of knowledge and evidence used to support nursing practices (the American Association of Colleges of Nursing, 2016) . Evidence-based practice requires using research outcomes to drive clinical decisions and care. -

Nursing Students' Perspectives on Telenursing in Patient Care After
Clinical Simulation in Nursing (2015) 11, 244-250 www.elsevier.com/locate/ecsn Featured Article Nursing Students’ Perspectives on Telenursing in Patient Care After Simulation Inger Ase Reierson, RN, MNSca,*, Hilde Solli, RN, MNSc, CCNa, Ida Torunn Bjørk, RN, MNSc, Dr.polit.a,b aFaculty of Health and Social Studies, Institute of Health Studies, Telemark University College, 3901 Porsgrunn, Norway bFaculty of Medicine, Institute of Health and Society, Department of Nursing Science, University of Oslo, 0318 Oslo, Norway KEYWORDS Abstract telenursing; Background: This article presents the perspectives of undergraduate nursing students on telenursing simulation; in patient care after simulating three telenursing scenarios using real-time video and audio nursing education; technology. information and Methods: An exploratory design using focus group interviews was performed; data were analyzed us- communication ing qualitative content analysis. technology; Results: Five main categories arose: learning a different nursing role, influence on nursing assessment qualitative content and decision making, reflections on the quality of remote comforting and care, empowering the pa- analysis tient, and ethical and economic reflections. Conclusions: Delivering telenursing care was regarded as important yet complex activity. Telenursing simulation should be integrated into undergraduate nursing education. Cite this article: Reierson, I. A., Solli, H., & Bjørk, I. T. (2015, April). Nursing students’ perspectives on telenursing in patient care after simulation. Clinical Simulation in Nursing, 11(4), 244-250. http://dx.doi.org/ 10.1016/j.ecns.2015.02.003. Ó 2015 International Nursing Association for Clinical Simulation and Learning. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/ by-nc-nd/4.0/). -

Strategies to Overcome the Nursing Shortage Edward A
Walden University ScholarWorks Walden Dissertations and Doctoral Studies Walden Dissertations and Doctoral Studies Collection 2017 Strategies to Overcome the Nursing Shortage Edward A. Mehdaova Walden University Follow this and additional works at: https://scholarworks.waldenu.edu/dissertations Part of the Health and Medical Administration Commons This Dissertation is brought to you for free and open access by the Walden Dissertations and Doctoral Studies Collection at ScholarWorks. It has been accepted for inclusion in Walden Dissertations and Doctoral Studies by an authorized administrator of ScholarWorks. For more information, please contact [email protected]. Walden University College of Management and Technology This is to certify that the doctoral study by Edward Mehdaova has been found to be complete and satisfactory in all respects, and that any and all revisions required by the review committee have been made. Review Committee Dr. Mohamad Hammoud, Committee Chairperson, Doctor of Business Administration Faculty Dr. Michael Campo, Committee Member, Doctor of Business Administration Faculty Dr. Roger Mayer, University Reviewer, Doctor of Business Administration Faculty Chief Academic Officer Eric Riedel, Ph.D. Walden University 2017 Abstract Strategies to Overcome the Nursing Shortage by Edward Mehdaova MBA, Indiana Wesleyan University, 2012 BSBA, Indiana Wesleyan University, 2009 Doctoral Study Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Business Administration Walden University December 2017 Abstract Nursing shortage is a growing problem in the healthcare industry as hospital leaders are experiencing difficulties recruiting and retaining nurses. Guided by the PESTEL framework theory, the purpose of this case study was to explore strategies healthcare leaders use to overcome a nursing shortage. -

SYLLABUS-NURSING 3304-110 NURSING RESEARCH Texas A&M University - Central Texas Spring 2021 Texas A&M University-Central Texas
SYLLABUS-NURSING 3304-110 NURSING RESEARCH Texas A&M University - Central Texas Spring 2021 Texas A&M University-Central Texas COURSE DATES, MODALITY, AND LOCATION Course Dates- January 19-May 14 web-based course taught online through the TAMUCT Canvas Learning Management System: [https://tamuct.instructure.com] INSTRUCTOR AND CONTACT INFORMATION Instructor: Lee Ogburn-Russell Office: On line Phone: 512-864-5090 Email: [email protected]. This is the preferred e-mail. Office Hours: Phone or synchronous online interaction can be arranged by appointment to accommodate student needs. Student-instructor interaction: Emails and messages within Canvas are checked daily. Students may expect a response within 24 to 48 hours. Office hours may also include synchronous online interaction to meet student’s learning needs and serving as a resource person to guide the student in the learning process. Other teaching strategies include online assignments, online discussion boards, a scholarly paper, and quizzes. WARRIOR SHIELD Emergency Warning System for Texas A&M University-Central Texas Warrior Shield is an emergency notification service that gives Texas A&M University-Central Texas the ability to communicate health and safety emergency information quickly via email, text message, and social media. All students are automatically enrolled in Warrior Shield through their myCT email account. Connect to Warrior Shield by 911Cellular [https://portal.publicsafetycloud.net/Account/Login] to change where you receive your alerts or to opt out. By staying enrolled in Warrior Shield, university officials can quickly pass on safety-related information, regardless of your location. COVID-19 SAFETY MEASURES To promote public safety and protect students, faculty, and staff during the coronavirus pandemic, Texas A&M University-Central Texas has adopted policies and practices to minimize virus transmission. -

Nursing and Allied Health Shortages: TBR Responds. INSTITUTION Tennessee State Board of Regents, Nashville
DOCUMENT RESUME ED 480 709 CE 085 492 AUTHOR Berryman, Treva TITLE Nursing and Allied Health Shortages: TBR Responds. INSTITUTION Tennessee State Board of Regents, Nashville. PUB DATE 2002-12-00 NOTE 12p. AVAILABLE FROM For full text: http://www.tbr.state.tn.us/academic_affairs/ news/nrsah.htm. PUB TYPE Information Analyses (070) Opinion Papers (120) EDRS PRICE EDRS Price MF01/PC01 Plus Postage. DESCRIPTORS Allied Health Occupations; Allied Health Occupations Education; Demand Occupations; Education Work Relationship; Educational Finance; Educational Planning; Employment Patterns; *Labor Needs; Labor Turnover; Nurses; *Nursing; *Nursing Education; *Policy Formation; Postsecondary Education; *Public Policy; Role of Education; Secondary Education; Statewide Planning; Student Financial Aid; *Student Recruitment IDENTIFIERS Health Personnel Shortage; Nursing Shortage; *Tennessee ABSTRACT Staff members of the Tennessee Board of Regents (TBR) and the Tennessee Higher Education Commission worked jointly to establish a task force to investigate and develop recommendations for addressing the workforce shortages in nursing and allied health in Tennessee. The investigation established that Tennessee already has a workforce shortage of health care professionals, especially registered nurses, and that the shortage will become critical over the next 10 to 15 years. The task force recommended that TBR institutions apply for the federal grants available through the Nursing Reinvestment Act. The following are among the eight recommendations addressed -

The Nursing Shortage
THE STATE EDUCATION DEPARTMENT / THE UNIVERSITY OF THE STATE OF NEW YORK / ALBANY, NY 12234 TO: The Honorable the Members of the Board of Regents FROM: Johanna Duncan-Poitier COMMITTEE: Full Board TITLE: The Nursing Shortage DATE OF SUBMISSION: April 16, 2001 PROPOSED HANDLING: Discussion RATIONALE FOR ITEM: To inform the Regents about an emerging public protection issue and gain support of recommended actions STRATEGIC GOAL: Goal 3 AUTHORIZATION(S): EXECUTIVE SUMMARY This is the eighth in a series of reports to the Board of Regents on emerging issues in professional regulation. The report deals with a potential crisis that may seriously affect all New Yorkers in the next few years – the nursing shortage. Previous reports in this series include corporate practice of the professions, telepractice, cross- jurisdictional professional practice, continuing competence, effective professional regulation and discipline, illegal (unlicensed) practice of the professions, and rising consumer expectations. This report describes a fundamental health care issue that is basic to the Regents public protection mission. The critical shortage of qualified nurses projected within the next five years will have a profound effect on health care for New York’s consumers well into this new century. Failure to successfully address the problem will threaten the quality and safety of the entire health care system in this State, the welfare of consumers who depend on this system for patient care, and the future of the professionals who practice within this system. Research points to a nursing shortage that, if unaddressed, will be more severe and longer in duration than those previously experienced in New York. -

E-Health and Telehealth for Consumer Empowerment: Issues and Trends
Summer Institute in Nursing Informatics (SINI) 2008 Part I Item Type Poster/Presentation; Conference/Congress Authors Nobumoto, Tak; Coates, Jean, M.S., R.N.; McCasky, Teresa; Staggs, Stuart; Currie, Leanne; Murphy, Judy; Shapiro, Jason; Staggers, Nancy; Alexander, Gregory Lynn, 1961-; Smith, Kathleen, M.Sc.Ed., R.N.-B.C.; Tyler, Denise, M.S.N., M.B.A., R.N.- B.C.; Warren, Judith J., Ph.D., R.N.; Elfrink, Victoria L.; Elenberg, K. J.; Crilly, John Publication Date 2008 Keywords Medical protocols; Nursing informatics; Patient Care; Telemedicine Download date 24/09/2021 21:17:32 Item License https://creativecommons.org/licenses/by-nc-nd/4.0/ Link to Item http://hdl.handle.net/10713/3973 E-Health and Telehealth for Consumer Empowerment: Issues and Trends Victoria L. Elfrink, PhD, RN-BC Loretta Schlachta-Fairchild, RN, PhD, FACHE, LTC(ret), AN www.itelehealthinc.com [email protected] or [email protected] [email protected] Copyright © iTelehealth Inc. 2008 Objectives Identify categories of emerging personal telehealth technologies Identify nursing practice implications of emerging telehealth and consumer technologies Identify principles for safe patient care and data management using emerging telehealth and consumer technologies Copyright © iTelehealth Inc. 2008 Definitions Telehealth encompasses the use of telephonic, telehealth, Internet, sensors, video, remote diagnostics and/or other interactive technologies which allow interchange between patients and nurses or between nurses and other healthcare providers. -

Education Standards and Curriculum Guidelines for Neonatal Nurse Practitioner Programs
Education Standards and Curriculum Guidelines for Neonatal Nurse Practitioner Programs National Association of Neonatal Nurses 8735 West Higgins Road, Suite 300 Chicago, IL 60631 Phone 800.451.3795, 847.375.3660 Fax 866.927.5321 www.nann.org NANN Board of Directors (2013-2014) Cheryl Ann Carlson, PhD APRN NNP-BC, President Pamela Spivey, MSN RN CCNS, President-Elect Joan Rikli, MSN RN CPNP-PC NE-BC, Secretary-Treasurer Suzanne Staebler, DNP APRN NNP-BC, NANNP Council Chair Lori Brittingham, BSN RN Kimberly Guglielmo, BSN RNC-NIC Pamela Heaberlin, MS RN NNP-BC Karen McDonald, DNPc NNP-BC Donna J. Ryan, DNP RN NANNP Council (2013-2014) Suzanne Staebler, DNP APRN NNP-BC, Chair Mary Beth Bodin, DNP CRNP NNP-BC Terri A. Cavaliere, DNP RN NNP-BC Mary Mikolajcik Kaminski, MS RN NNP-BC Donna LoSasso, DNP NNP-BC Susan R. Meier, DNP APRN NNP-BC Lorraine Arriola Shields, MN RNC NNP-BC CNS Roxanne Stahl, MS NNP-BC Task Force for Revision of NNP Education Standards (2013–2014) Debra A. Sansoucie, EdD APRN NNP-BC, Co-Chair Paula M. Timoney, DNP ARNP NNP-BC, Co-Chair Mary Beth Bodin, DNP CRNP NNP-BC, Council Liaison Debbie Armentrout, PhD RNC NNP Carol Botwinski, EdD ARNP NNP-BC Terri Cavaliere, DNP RN NNP-BC Amy Koehn, PhD(c) NNP-BC Darlene Moore, MN RN NNP-BC Leanne Nantais-Smith, PhD RNC NNP-BC Patricia Thomas, PhD RN NNP-BC Copyright © 2014 by the National Association of Neonatal Nurses. No part of this document may be reproduced without the written consent of the National Association of Neonatal Nurses. -

Download Article
Guest Editorial MSW, LCSW examine the value of IT in the homecare venue. Their article describes the HOUSE (Home Operations Utilizing Safety Education) Program, which uses patient assessment, education, and other interventions to adjust the home environment to meet patients’ needs. It explains how assessment and education cost-effectively and efficiently link inpatient, ambulatory, and homecare while reducing preventable injuries in a predominantly rural setting—all by using a handheld telephone. This is Diane J. Skiba Roy L. Simpson a perfect example of a simple technological solution to address patient safety issues in the home. Will Technology Change Our Practice? In another example of the value of handheld technology, “The Transforming Effect of Handheld To measure blood pressure in 1847, you Computers on Nursing Practice,”Brent W. inserted catheters directly into the artery. To draw Thompson, DNSc, RN, explains how handheld blood in 1860, you perforated the skin with 12 computers have the power to transform nursing small lancets, placed a hot cupping glass over the care. He points to increasingly decentralized wound, extracted 3 to 5 oz of blood, and then communication, electronic health records, and dressed the wound with lint and plaster. Today, nurses’ greater need for information at the we have automatic noninvasive blood pressure point-of-care as the reasons behind and for this monitors and, in the not so distant future, we will new technology. Access to information at your have a technique that will use sound to painlessly fingertips allows nurses to practice as knowledge extract a number of important molecules through workers. He discusses the effects of handheld the skin and render the familiar needle prick resources, calculators, databases, electronic obsolete. -

The Benefits of Using Standardized Nursing Terminology
Page 1 of 20 Selecting a Standardized Terminology for the Electronic Health Record that Reveals the Impact of Nursing on Patient Care By Cynthia B. Lundberg, R.N., BSN; SNOMED Terminology Solutions; Judith J. Warren, PhD, RN, BC, FAAN, FACMI; University of Kansas; Jane Brokel, PhD, RN, NANDA International; Gloria M. Bulechek, PhD, RN, FAAN; Nursing Interventions Classification; Howard K. Butcher, PhD, RN, APRN, BC; Nursing Interventions Classification; Joanne McCloskey Dochterman, PhD, RN, FAAN; Nursing Interventions Classification; Marion Johnson, PhD, RN; Nursing Outcomes Classification; Meridean Maas PhD, RN; Nursing Outcomes Classification; Karen S. Martin, RN, NSN, FAAN; Omaha System; Sue Moorhead PhD, RN, Nursing Outcomes Classification; Christine Spisla, RN, MSN; SNOMED Terminology Solutions; Elizabeth Swanson, PhD, RN; Nursing Outcomes Classification, Sharon Giarrizzo-Wilson, RN, BSN/MS, CNOR, Association of PeriOperative Registered Nurses Citation: Lundberg, C., Warren, J.., Brokel, J., Bulechek, G., Butcher, H., McCloskey Dochterman, J., Johnson, M., Mass, M., Martin, K., Moorhead, S., Spisla, C., Swanson, E., & Giarrizzo-Wilson, S. (June, 2008). Selecting a Standardized Terminology for the Electronic Health Record that Reveals the Impact of Nursing on Patient Care. Online Journal of Nursing Informatics (OJNI), 12, (2). Available at http:ojni.org/12_2/lundberg.pdf Page 2 of 20 Abstract Using standardized terminology within electronic health records is critical for nurses to communicate their impact on patient care to the multidisciplinary team. The universal requirement for quality patient care, internal control, efficiency and cost containment, has made it imperative to express nursing knowledge in a meaningful way that can be shared across disciplines and care settings. The documentation of nursing care, using an electronic health record, demonstrates the impact of nursing care on patient care and validates the significance of nursing practice. -

Nursing Research Society of India
NURSING RESEARCH SOCIETY OF INDIA NURSING RESEARCH GUIDELINES BOOKLET- 1 PREPARED BY: Dr. Assuma Beevi.T.M. M.Sc(N). Ph.D. Dip.Med.Edn. DHM., CHPE. Cert.HRM VICE PRESIDENT, NRSI Joint Director, MIMS Academy & Principal, MIMS College of Nursing, Puthukode, Malappuram Dt.Kerala ENDORSED BY: NRSI EXECUTIVES NURSING RESEARCH SOCIETY OF INDIA ESTABLISHED IN THE YEAR 1982. OCTOBER, 2016 HALDWANI 2 THE SPIRIT OF PROFESSIONAL GUIDELINES FOR NURSING RESEARCH IN INDIA Practice as a nurse is based upon a relationship of mutual trust between patients and health care practitioners. Nursing, a service profession demands much dedication. The promise or the commitment the nurse made to the public upon graduation through the oath to provide compassionate humanistic care with sound professional and ethical principles in their practice. This means that nurse is committed to the society and the service provided is a moral enterprise. Nurse, being a professional has the moral responsibility to develop health care practices that are affordable, and cost effective state of the art interventions. For developing such knowledge, the nurse is committed to conduct research. Evidences created by good quality research only will yield scientific knowledge. The nurse is destined to follow the moral and ethical principles along with scientific vigor while conducting research. Nursing Research Society of India takes it as a privilege to submit such guidelines to fellow nurses as the only organizations for nurse researchers in India. 3 Table of contents 1. Preamble 2. Introduction 3. Professional competence 4. Participant priority 5. Preserve safety 6. Promote confidentiality 7. Ethical code of conduct 8.