Supplement 3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetically Determined Hypoalbuminemia As a Risk Factor for Hypertension: Instrumental Variable Analysis Jong Wook Choi1, Joon‑Sung Park2* & Chang Hwa Lee2*
www.nature.com/scientificreports OPEN Genetically determined hypoalbuminemia as a risk factor for hypertension: instrumental variable analysis Jong Wook Choi1, Joon‑Sung Park2* & Chang Hwa Lee2* Hypoalbuminemia is associated with vascular endothelial dysfunction and the development of chronic cardiovascular diseases. However, the relationship between serum albumin concentration and blood pressure changes remains controversial. Community‑based longitudinal cohort data collected from Korean Genome and Epidemiology Study were used in this study. Hypoalbuminemia was defned as a serum albumin concentration of ≤ 4.0 g/dL. A total of 4325 participants were categorized into control (n = 3157) and hypoalbuminemia (n = 1168) groups. Serum albumin had a non‑linear relationship with the risk of hypertension development. A genome‑wide association study revealed 71 susceptibility loci associated with hypoalbuminemia. Among susceptibility loci, genetic variations at rs2894536 in LOC107986598 and rs10972486 in ATP8B5P were related to elevated blood pressure. Serum albumin (HR = 0.654, 95% CI 0.521–0.820) and polymorphisms of rs2894536 (HR = 1.176, 95% CI 1.015–1.361) and rs10972486 (HR = 1.152, 95% CI 1.009–1.316) were signifcant predictors of hypertension development. Increased albumin concentration instrumented by 2 hypoalbuminemia‑associated SNPs (rs2894536 and rs10972486) was associated with decreased HRs for hypertension development (HR = 0.762, 95% CI 0.659–0.882 and HR = 0.759, 95% CI 0.656–0.878). Our study demonstrated that genetically determined hypoalbuminemia is a signifcant predictor of incipient hypertension. Albumin, one of the major serum proteins, has multiple important physiological functions involving stabilization of plasma colloid osmotic pressure, transportation of diverse substances, and signifcant antioxidant activity, and its concentration is fnely regulated by various systems in the physiologic state 1. -

Glycated Hemoglobin and Glycated Albumin in Patients with Diabetes
Kitajima et al. Renal Replacement Therapy (2020) 6:10 https://doi.org/10.1186/s41100-020-0260-5 RESEARCH Open Access Glycated hemoglobin and glycated albumin in patients with diabetes undergoing hemodiafiltration Yukie Kitajima1*, Shunichiro Urabe2, Takashi Hosono2, Satoshi Yoshikawa3, Yuzuru Sato3 and Toru Hyodo2 Abstract Background: Online hemodiafiltration (OHDF), which results in high albumin leakage, is now widely used in Japan for dialysis, since the national insurance system began reimbursing its costs in 2012. Glycated albumin (GA) levels are affected by albumin leakage into effluent dialysate fluid. Therefore, GA levels in patients requiring diabetes- related dialysis undergoing OHDF require monitoring. However, there have been no previous reports on glycemic control indicators of patients with diabetes undergoing OHDF. We aimed to develop a glycemic control index for patients requiring diabetes-related dialysis undergoing OHDF. Methods: This study comprised 133 diabetic patients undergoing OHDF. We examined the correlation between GA and glycated hemoglobin (HbA1c) levels. We analyzed effluent dialysate fluid samples from 41 patients classified into 3 groups, namely, group A, non-protein-leaking OHDF (n = 20); group B, protein-leaking OHDF (n = 14); and group C, highly efficient protein-leaking OHDF (n = 7). We examined the association between GA and HbA1c levels in each group and among patients. Results: A significant positive correlation was observed between GA and HbA1c levels (r = 0.562, p < 0.0001). There was no significant correlation between pre-dialysis blood glucose levels and HbA1c or GA levels as observed on regular blood tests performed under non-fasting conditions. Patients were classified into 2 groups based on their mean albumin levels (3.4 g/dL cutoff). -

Hba1c %, Total Serum Protein and Albumin Levels in Type 2 Diabetes Mellitus Patients: a Case-Control Study Dr
European Journal of Molecular & Clinical Medicine (EJMCM) ISSN: 2515-8260 Volume 07, Issue 11, 2020 Original research article HbA1c %, total serum protein and albumin levels in type 2 diabetes mellitus patients: a case-control study Dr. Shweta Kumari1*, Dr. Supriya2 1Junior Resident (Academic), Department of Pathology Darbhanga Medical College and Hospital, Laheriasarai, Darbhanga, Bihar, India 2Junior Resident (Academic), Department of Pathology Darbhanga Medical College and Hospital, Laheriasarai, Darbhanga, Bihar, India Corresponding Author: Dr. Shweta Kumari Abstract Aim: the aim of the study to assessment of glycated haemoglobin, total protein and albumin levels in patients with type 2 diabetes mellitus. Methods: This case control study was done the Department of Pathology Darbhanga Medical College and Hospital, Laheriasarai, Darbhanga, Bihar, India, for 1 year. The research enlisted 100 participants, 50 of whom were diabetic and 50 of whom were not, all of whom were between the ages of 40 and 70. Every patient's blood sample was obtained in 5mls, with 1ml dispensed into EDTA for glycated haemoglobin estimation and 4ml dispensed into clear containers for serum albumin and total protein estimation. Normal procedures were used to determine the amount of glycated haemoglobin, estimate serum albumin, and estimate total protein. Results: The mean level of HbA1c was significantly higher in the diabetic subjects when compared with control group (10.11±1.41Vs 6.18±0.71; p=0.000). There was no significant differences observed between the age, the serum levels of Albumin and Total protein in the test and control subjects (p>0.05). Conclusion: The present study showed significantly higher mean levels of HbA1c in the diabetic patients compared with the control subjects. -

Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: a Retrospective Case Series (1999–2018) †
animals Article Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: A Retrospective Case Series (1999–2018) † Maria Alfonsa Cavalera 1, Floriana Gernone 1, Annamaria Uva 1, Paola D’Ippolito 2, Xavier Roura 3 and Andrea Zatelli 1,* 1 Department of Veterinary Medicine, University of Bari, 70010 Valenzano, Italy; [email protected] (M.A.C.); fl[email protected] (F.G.); [email protected] (A.U.) 2 Veterinary diagnostic Lab ACV Triggiano, 70019 Triggiano, Italy; [email protected] 3 Hospital Clínic Veterinari, Universitat Autònoma de Barcelona, 08193 Bellaterra, Spain; [email protected] * Correspondence: [email protected]; Tel.: +39-080-4679804 † This study was partially presented as oral communication at the 11th ECVIM-CA/ESVIM Congress, Dublin (Ireland) as “Congenital nephrotic syndrome with renal glomerular immaturity in 7 Boxer dogs”. Zatelli, A., Domenech, O., Bussadori, C., Lubas, G., Del Piero, F. Simple Summary: This study describes clinical findings in Boxer dogs with renal maldevelopment and proposes a possible mode of inheritance. Medical records of 9 female Boxer dogs, older than 5 months and with a clinical diagnosis of proteinuric chronic kidney disease prior to one year of age, showed the presence of polyuria and polydipsia, decreased appetite, weight loss, lethargy and weakness in all affected dogs. Common laboratory findings were proteinuria and diluted urine, non- regenerative anemia, azotemia, hyperphosphatemia, hypoalbuminemia and hypercholesterolemia. Citation: Cavalera, M.A.; Gernone, Histopathology of the kidneys identified the presence of immature glomeruli in all dogs. In 7 out F.; Uva, A.; D’Ippolito, P.; Roura, X.; of 9 related dogs, the pedigree analysis showed that a simple autosomal recessive trait may be a Zatelli, A. -

International Journal of Medical and Biomedical Studies (IJMBS)
|| ISSN(online): 2589-8698 || ISSN(print): 2589-868X || International Journal of Medical and Biomedical Studies Available Online at www.ijmbs.info PubMed (National Library of Medicine ID: 101738825) Index Copernicus Value 2018: 75.71 Original Research Article Volume 4, Issue 3; March: 2020; Page No. 209-213 EVALUATION OF CHANGES IN LEVELS OF GLYCATED HEMOGLOBIN, TOTAL PROTEIN AND ALBUMIN IN PATIENTS DIAGNOSED WITH TYPE 2 DIABETES MELLITUS Dr. Vivek Kumar1, Dr. Neeraj Kumar2, Dr. Jaideo Prasad3 1Tutor, Dept. of Pathology, Anugrah Narayan Magadh Medical College and Hospital, Gaya, Bihar, India. 2Senior Resident, Dept. of Medicine, Anugrah Narayan Magadh Medical College and Hospital, Gaya, Bihar, India. 3Prof & HOD, Dept. of Pathology, Anugrah Narayan Magadh Medical College and Hospital, Gaya, Bihar, India. Article Info: Received 07 February 2020; Accepted 26 March 2020 DOI: https://doi.org/10.32553/ijmbs.v4i3.1099 Corresponding author: Dr. Neeraj Kumar Conflict of interest: No conflict of interest. Abstract Insulin resistance in Type 2 diabetes mellitus metabolism of carbohydrates, lipids and proteins gives an estimate of the average blood glucose the previous three months in diabetes. Protein and HbA1c have been shown to be involved complications of diabetes mellitus. Hence based on above findings the present study was planned for Evaluation of Changes in Levels of Glycated Hemoglobin, Total Protein and Albumin in Patients Diagnosed with Type 2 Diabetes Mellitus. The present study was planned in Anugrah Narayan Magadh Medical College and Hospital, Gaya, Bihar, India. In the present study 50 cases were evaluated. The 25 cases were enrolled on the Group A as normal cases in Control group. -

Plasma Protein Binding Structure Activity Relationship Related to the N-Terminus of Daptomycin
Monash Institute of Pharmaceutical P1318 Sciences ECCMID 2017, Plasma protein binding structure activity relationship related to the N-terminus of daptomycin 381 Royal Parade, Parkville, VIC 3052 Melbourne, Australia Vienna 1 2 3 2 4 1 Tel: +61 3 9903 9539 Elena K. Schneider , Johnny X. Huang , Vincenzo Carbone , Matthew A. Cooper , Jian Li *, Tony Velkov * [email protected] 1Drug Development and Innovation, Drug Delivery, Disposition and Dynamics. Monash Institute of Pharmaceutical Sciences, Monash University, Australia. 2Institute for Molecular Bioscience, The University of Queensland St Lucia QLD 4072. 3Animal Nutrition and Health, Ag Research Limited, Grasslands Research Centre, Palmerston North, New Zealand. 4Monash Biomedicine Discovery Institute, Department of Microbiology, Monash University, Australia. Abstract Methods Results Background: Daptomycin is a lipopeptide antibiotic that is highly bound to plasma proteins. To date the plasma components and • Flourometric binding assay: • SPR: structure-activity relationships responsible for the plasma protein binding profile of daptomycin remain uncharacterized. We used the site selective fluorescent probes . Native daptomycin binds in order of decreasing Methods: dansylamide (site 1) and dansylsarcosine affinity to: HSA >> α-1-antitrypsin > low density (site 2) on HSA. As the control we employed lipoprotein (LDL) ≥ haemoglobin > sex hormone • In the present study we have employed surface plasmon resonance (SPR) and fluorescence displacement assay to Nifedipine for site 1 and ibuprofen -

Increasing Ferritin Predicts Early Death in Adult Hemophagocytic Lymphohistiocytosis
Henry Ford Health System Henry Ford Health System Scholarly Commons Pathology Articles Pathology 2-17-2021 Increasing ferritin predicts early death in adult hemophagocytic lymphohistiocytosis Rand Abou Shaar Charles S. Eby Suzanne van Dorp Theo de Witte Zaher K. Otrock Follow this and additional works at: https://scholarlycommons.henryford.com/pathology_articles Received: 13 November 2020 | Accepted: 29 January 2021 DOI: 10.1111/ijlh.13489 ORIGINAL ARTICLE Increasing ferritin predicts early death in adult hemophagocytic lymphohistiocytosis Rand Abou Shaar1 | Charles S. Eby2 | Suzanne van Dorp3 | Theo de Witte3 | Zaher K. Otrock1 1Department of Pathology and Laboratory Medicine, Henry Ford Hospital, Detroit, MI, Abstract USA Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare syndrome of 2 Department of Pathology and Immunology, pathologic immune activation. Most studies on adult HLH have evaluated prognostic Washington University School of Medicine, St. Louis, MO, USA factors for overall survival; factors predicting early mortality have not been suffi- 3Radboud University Medical Center, ciently investigated. Nijmegen, Netherlands Methods: This was a collaborative study between Henry Ford Hospital and Barnes- Correspondence Jewish Hospital. We identified all adult HLH patients with at least 2 ferritin levels Zaher K. Otrock, Transfusion Medicine Division, Department of Pathology and within 30 days from admission. Laboratory Medicine, Henry Ford Hospital, Results: One- hundred twenty- four patients were identified. There were -
Of Treatment of Hyperuricemia on Effect
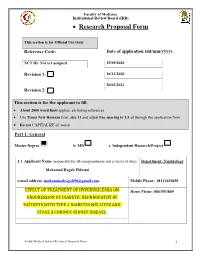
Faculty of Medicine Institutional Review Board (IRB) • Research Proposal Form This section is for Official Use Only Reference Code: Date of application (dd/mm/yyyy): NCT ID: Not yet assigned 15/09/2020 Revision 1: 10/12/2020 20/02/2021 Revision 2: This section is for the applicant to fill. • About 2000 word limit applies, excluding references. • Use Times New Romans Font, size 11 and adjust line spacing to 1.5 all through the application form • Do not CAPITALIZE all words Part 1: General Master Degree b. MD c. Independent Research/Project 1.1 Applicant Name (responsible for all correspondences and accuracy of data): Department: Nephrology Mohamed Ragab Eldremi email address: [email protected] Mobile Phone: 01114430050 EFFECT OF TREATMENT OF HYPERURICEMIA ON Home Phone: 0863553849 PROGRESSION OF DIABETIC NEPHROPATHY IN PATIENTS WITH TYPE 2 DIABETES MELLITUS AND STAGE 3 CHRONIC KIDNEY DISEASE. Assiut Medical School Research Proposal Form 1 Faculty of Medicine Institutional Review Board (IRB) 1.2 English Title of research project: EFFECT OF TREATMENT OF HYPERURICEMIA ON PROGRESSION OF DIABETIC NEPHROPATHY IN PATIENTS WITH TYPE 2 DIABETES MELLITUS AND STAGE 3 CHRONIC KIDNEY DISEASE. 1.3 Do you need funding from Assiut Medical School Grants Office? Yes No (If no, skip and delete Part 4) Mention other sponsoring agent(s) if any: ………………no…………………………... Part 2: Research Details Assiut Medical School Research Proposal Form 2 Faculty of Medicine Institutional Review Board (IRB) 2.1 Background (Research Question, Available Data from the literature, Current strategy for dealing with the problem, Rationale of the research that paves the way to the aim(s) of the work). -

Serum Uric Acid Concentrations and Risk of Adverse Outcomes in Patients with COVID-19
ORIGINAL RESEARCH published: 06 May 2021 doi: 10.3389/fendo.2021.633767 Serum Uric Acid Concentrations and Risk of Adverse Outcomes in Patients With COVID-19 † † † † † Bo Chen 1 , Chenyang Lu 1 , Hong-Qiu Gu 2,3 , Yang Li 4 , Guqin Zhang 5 , Jonathan Lio 6, Xiongyan Luo 1, Lingshu Zhang 1, Yidan Hu 1, Xiaomeng Lan 7, Zerong Chen 7, Qibing Xie 1* and Huaqin Pan 8,9,10* 1 Department of Rheumatology and Immunology, West China Hospital, Sichuan University, Chengdu, China, 2 China National Clinical Research Center for Neurological Diseases, Beijing Tiantan Hospital, Capital Medical University, Beijing, China, 3 National Center for Healthcare Quality Management in Neurological Diseases, Beijing Tiantan Hospital, Capital Medical University, Beijing, China, 4 Department of Endocrinology, West China Hospital, Sichuan University, Chengdu, China, 5 Department of Respiratory and Critical Care Medicine, Zhongnan Hospital of Wuhan University, Wuhan, China, 6 Internal Medicine, University of Chicago, Chicago, IL, United States, 7 West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China, 8 Department of Critical Care Medicine, Zhongnan Hospital of Wuhan University, Wuhan, China, 9 Department of Critical Care Medicine, Leishenshan Hospital, Wuhan, China, 10 Clinical Research Edited by: Center of Hubei Critical Care Medicine, Wuhan, China Jeff M. P. Holly, University of Bristol, United Kingdom Background: Although hyperuricemia frequently associates with respiratory diseases, Reviewed by: Yu Sun, patients with severe coronavirus disease 2019 (COVID-19) and severe acute respiratory Shandong University, China syndrome (SARS) can show marked hypouricemia. Previous studies on the association of Ma. Cecilia Opazo, Andres Bello University, Chile serum uric acid with risk of adverse outcomes related to COVID-19 have produced *Correspondence: contradictory results. -

Detailed Structure and Pathophysiological Roles of the Iga-Albumin Complex in Multiple Myeloma
International Journal of Molecular Sciences Article Detailed Structure and Pathophysiological Roles of the IgA-Albumin Complex in Multiple Myeloma Yuki Kawata 1, Hisashi Hirano 1, Ren Takahashi 1, Yukari Miyano 1, Ayuko Kimura 1, Natsumi Sato 1, Yukio Morita 2, Hirokazu Kimura 1,* and Kiyotaka Fujita 1 1 Department of Health Sciences, Gunma Paz University Graduate School of Health Sciences, 1-7-1, Tonyamachi, Takasaki-shi, Gunma 370-0006, Japan; [email protected] (Y.K.); [email protected] (H.H.); [email protected] (R.T.); [email protected] (Y.M.); [email protected] (A.K.); [email protected] (N.S.); [email protected] (K.F.) 2 Laboratory of Public Health II, Azabu University School of Veterinary Medicine, 1-17-71, Fuchinobe, Chuo-ku, Sagamihara, Kanagawa 252-5201, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-27-365-3366; Fax: +81-27-388-0386 Abstract: Immunoglobulin A (IgA)-albumin complexes may be associated with pathophysiology of multiple myeloma, although the etiology is not clear. Detailed structural analyses of these protein– protein complexes may contribute to our understanding of the pathophysiology of this disease. We analyzed the structure of the IgA-albumin complex using various electrophoresis, mass spectrom- etry, and in silico techniques. The data based on the electrophoresis and mass spectrometry showed that IgA in the sera of patients was dimeric, linked via the J chain. Only dimeric IgA can bind to albumin molecules leading to IgA-albumin complexes, although both monomeric and dimeric forms of IgA were present in the sera. -

Serum Total Protein, Albumin, Globulin Population of Various Ages and Sex in Karachi and Their Ratio in Apparently Healthy
SERUM TOTAL PROTEIN, ALBUMIN, GLOBULIN POPULATION OF VARIOUS AGES AND SEX IN KARACHI AND THEIR RATIO IN APPARENTLY HEALTHY Pages with reference to book, From 12 To 16 Khushnaseeb Ibrahim, Sarwar Jehan Zuberi ( PMRC Research Centre, Jinnah Postgraduate Medical Centre, Karachi. ) Syed Naznil Husnain ( Department of Biochemistry, University of Karachi, Karachi. ) Abstract Serum proteins, albumin and globulin in 456 (274 males and 182 females) subjects were within the normal range and showed unifornt distribution. Mean protein levels were low in infants under 0—1 year of age. No significant change was noted with age and sex in other groups. These values were considered to be normal for our population as all protein values fell within 2.5 and 97.5 percentile (95% of the total population) irrespective of age and sex except babies under 0—1 year. The average intake of protein/kg body weight was almost upto the recommended allowances(JPMA 39: 12, 1989). INTRODUCTION Serum protein levels in normals vary from 63—8 g% and albumin 4—6 g% 1-4 . This study repbrts levels of serum proteins, albumin, globulins and albumin/globulin ratios in healthy subjects and their relationship with age, sex and protein intake. SUBJECTS AND METHOD One thousand and thirty-six (526 males and 510 females) healthy subjects were selected from the hospital staff, well baby clinics, MCH Centres, primary and secondary schools, colleges and various organizations according to percentage distribution of age and sex in the Karachi population (Census, 1972). Information regarding age, sex, general physical health, dietary history, height and weight were recorded on a preceded proforma. -

Calcium and Phosphorus Metabolism of Bone Tissue
ÚSTAV LÉKAŘSKÉ BIOCH EMIE A LABORATORNÍ DIAGNO STIKY 1. LF UK Calcium and phosphorus Metabolism of bone tissue General Medicine Lenka Fialová & Martin Vejražka translated and edited by Jan Pláteník 2018/2019 1 Bone Tissue Bone provides mechanical support and protection to soft organs, enables movement, hosts hematopoietic tissue, and serves as storage of calcium, phosphate, and magnesium ions. From one third it consists of protein matrix , and from two thirds of the bone mineral . • The bone protein matrix contains mostly type I collagen (90 %); together with other proteins such as osteocalcin, osteonectin, osteopontin, etc. (10 %). • The bone mineral is composed from small crystals of hydroxyapatite Ca 10 (PO 4)6(OH) 2. Other compounds, such as calcium carbonate, calcium fluoride and magnesium phosphate, are present as well. The metabolic activity of bone tissue is provided by bone cells. Osteoblasts form osteoid (the bone protein matrix), into which mineral salts are deposited. Other cell types include osteoclasts , whose main function is bone resorption, and osteocytes , which complement activity of osteoclasts by providing fine tuning of bone resorption. During lifetime of an individual, the bone tissue is subject of perpetual remodelation , encompassing osteoclastic bone resorption followed by osteoblastic bone formation . Osteoclasts dissolve mineral components and degrade the bone matrix. On the other hand, osteoblasts intracellularly synthesize precursors of the bone matrix proteins. Functional coupling of bone resorption and formation ensures that the living bone tissue is constantly renewed. Metabolism of bones is tightly coupled to metabolism of calcium and phosphorus. 2 Calcium 2.1 Homeostasis of calcium Human body contains about 1,000 g of calcium.