Cancer (WHO–EORTC) ’ Most Common Group of Extranodal Non-Hodgkin S Classification (Table 1)[1]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Bexarotene (Targretin) Capsules Reference Number: PA.CP.PHAR.75 Effective Date: 09/11 Revision Log Last Review Date: 04/18
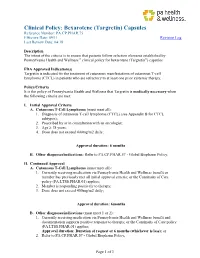
Clinical Policy: Bexarotene (Targretin) Capsules Reference Number: PA.CP.PHAR.75 Effective Date: 09/11 Revision Log Last Review Date: 04/18 Description The intent of the criteria is to ensure that patients follow selection elements established by Pennsylvania Health and Wellness ® clinical policy for bexarotene (Targretin®) capsules FDA Approved Indication(s) Targretin is indicated for the treatment of cutaneous manifestations of cutaneous T-cell lymphoma (CTCL) in patients who are refractory to at least one prior systemic therapy. Policy/Criteria It is the policy of Pennsylvania Health and Wellness that Targretin is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Cutaneous T-Cell Lymphoma (must meet all): 1. Diagnosis of cutaneous T-cell lymphoma (CTCL) (see Appendix B for CTCL subtypes); 2. Prescribed by or in consultation with an oncologist; 3. Age ≥ 18 years; 4. Dose does not exceed 400mg/m2 daily; Approval duration: 6 months B. Other diagnoses/indications: Refer to PA.CP.PHAR.57 - Global Biopharm Policy. II. Continued Approval A. Cutaneous T-Cell Lymphoma (must meet all): 1. Currently receiving medication via Pennsylvania Health and Wellness benefit or member has previously met all initial approval criteria; or the Continuity of Care policy (PA.LTSS.PHAR.01) applies; 2. Member is responding positively to therapy; 3. Dose does not exceed 400mg/m2 daily; Approval duration: 6months B. Other diagnoses/indications (must meet 1 or 2): 1. Currently receiving medication via Pennsylvania Health and Wellness benefit and documentation supports positive response to therapy; or the Continuity of Care policy (PA.LTSS.PHAR.01) applies; Approval duration: Duration of request or 6 months (whichever is less); or 2. -

Romidepsin (Istodax) Reference Number: ERX.SPA
Clinical Policy: Romidepsin (Istodax) Reference Number: ERX.SPA. 267 Effective Date: 12.01.18 Last Review Date: 11.20 Line of Business: Commercial, Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Romidepsin (Istodax®) is a histone deacetylase inhibitor. FDA Approved Indication(s) Istodax is indicated for the treatment of: • Cutaneous T-cell lymphoma (CTCL) in adult patients who have received at least one prior systemic therapy; • Peripheral T-cell lymphoma (PTCL) in adult patients who have received at least one prior therapy. o This indication is approved under accelerated approval based on response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. Health plan approved formularies should be reviewed for all coverage determinations. Requirements to use preferred alternative agents apply only when such requirements align with the health plan approved formulary. It is the policy of health plans affiliated with Envolve Pharmacy Solutions™ that Istodax and romidepsin injection solution are medically necessary when the following criteria are met: I. Initial Approval Criteria A. Cutaneous T-Cell Lymphoma (must meet all): 1. Diagnosis of CTCL (see Appendix D for examples of CTCL subtypes); 2. Prescribed by or in consultation with an oncologist or hematologist; 3. Age ≥ 18 years; 4. Request meets one of the following (a or b):* a. Dose does not exceed 14 mg/m2 for three days of a 28-day cycle; b. -

Message from the President
DermNewsletter of the American OsteopathicLine College of Dermatology Spring 2016 Vol. 32, No. 1 Message from the President Greetings from Houston, Texas - again! As President of the AOCD, I welcome you to another edition of DermLine. As I think about our recent past and the dramatic changes afoot, I recall Suzanne Sirota Rozenberg, DO, FAOCD, Past President of AOCD, commenting in the Spring 2014 edition of DermLine about the coming AOA/ACGME merger. As I stated previously, “Today, at this moment, we are living in yesterday’s future.” Our future has arrived. Because the AOA, along with the Accreditation Council for Graduate Medical Education and the American Association of Colleges of Osteopathic Medicine, have agreed to a single accreditation system for graduate medical education programs in the United States, our graduates of osteopathic institutions, along with graduates of allopathic medical schools will complete their residency and/or fellowship education in ACGME-accredited programs and demonstrate achievement of common milestones and competencies side-by-side. I hope you realize the power in the previous statement. Trained together, osteopathic and allopathic graduates will no longer be divided. Perhaps the most exciting news to share is the AAD vote that just passed last month. This has been a battle we have been fighting for generations. The vote suffered defeat in 2004 and 2010. On both occasions, a majority of the membership voted in favor, but the required two-thirds majority required to approve a change to the bylaws fell short. I was told I would never see this vote go through in my lifetime. -

Evaluation of Melanocyte Loss in Mycosis Fungoides Using SOX10 Immunohistochemistry
Article Evaluation of Melanocyte Loss in Mycosis Fungoides Using SOX10 Immunohistochemistry Cynthia Reyes Barron and Bruce R. Smoller * Department of Pathology and Laboratory Medicine, University of Rochester Medical Center, Rochester, NY 14642, USA; [email protected] * Correspondence: [email protected] Abstract: Mycosis fungoides (MF) is a subtype of primary cutaneous T-cell lymphoma (CTCL) with an indolent course that rarely progresses. Histologically, the lesions display a superficial lymphocytic infiltrate with epidermotropism of neoplastic T-cells. Hypopigmented MF is a rare variant that presents with hypopigmented lesions and is more likely to affect young patients. The etiology of the hypopigmentation is unclear. The aim of this study was to assess melanocyte loss in MF through immunohistochemistry (IHC) with SOX10. Twenty cases were evaluated, including seven of the hypopigmented subtype. The neoplastic epidermotropic infiltrate consisted predominantly of CD4+ T-cells in 65% of cases; CD8+ T-cells were present in moderate to abundant numbers in most cases. SOX10 IHC showed a decrease or focal complete loss of melanocytes in 50% of the cases. The predominant neoplastic cell type (CD4+/CD8+), age, race, gender, histologic features, and reported clinical pigmentation of the lesions were not predictive of melanocyte loss. A significant loss of melanocytes was observed in 43% of hypopigmented cases and 54% of conventional cases. Additional studies will increase our understanding of the relationship between observed pigmentation and the loss of melanocytes in MF. Citation: Barron, C.R.; Smoller, B.R. Evaluation of Melanocyte Loss in Keywords: mycosis fungoides; hypopigmented mycosis fungoides; SOX10; cutaneous T-cell lymphoma Mycosis Fungoides Using SOX10 Immunohistochemistry. -

Primary Cutaneous Lymphoma: ESMO Clinical Recommendations for Diagnosis, Treatment and Follow-Up R
Annals of Oncology 19 (Supplement 2): ii72–ii76, 2008 clinical recommendations doi:10.1093/annonc/mdn095 Primary cutaneous lymphoma: ESMO Clinical Recommendations for diagnosis, treatment and follow-up R. Dummer1 & M. Dreyling2 On behalf of the ESMO Guidelines Working Group* 1Department of Dermatology, University Hospital, Zu¨rich, Switzerland; 2Department of Medicine III, University Hospital Grosshadern, Munich, Germany introduction the quality of life due to their impact on skin appearance and annoying symptoms such as pruritus. In some cases they can Cutaneous lymphomas (CL) are the second most common already be disfiguring in early disease stages. In advanced stages, extranodal non-Hodgkin’s lymphomas. Their incidence is local skin problems are accompanied by systemic immune estimated at 1/100 000 yearly. Primary CL develop by definition suppression which results in an increased risk of infections and in the skin and remain confined to the skin for a long period of secondary malignancies. Some of the late-stage problems in time, while secondary CL reflect cutaneous spread from MF/SS patients might have been aggravated by earlier disseminated primary nodal or extranodal lymphomas. Primary therapeutic interventions, e.g. radiotherapy or phototherapy CL include a wide spectrum of clinically and histologically may contribute to mutations that increase the proliferative heterogeneous lymphoproliferative neoplasms: 75% of CL are and invasive capacity of the tumor cell populations. Cytotoxic cutaneous T-cell lymphomas (CTCL); 25% cutaneous B-cell drugs favor infectious complications. Most patients with lymphomas (CBCL); and a few percent other uncommon advanced disease may die due to secondary problems such as forms. CL and nodal or extracutaneous lymphomas with the infections. -

Treatment of Pagetoid Reticulosis with Intensity Modulated Radiation Therapy Charles Mount Washington University School of Medicine in St
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2014 Treatment of pagetoid reticulosis with intensity modulated radiation therapy Charles Mount Washington University School of Medicine in St. Louis Daniel Ferraro Washington University School of Medicine in St. Louis Alejandro Gru Washington University School of Medicine in St. Louis Matthew rB adbury Washington University School of Medicine in St. Louis Lynn Cornelius Washington University School of Medicine in St. Louis See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Mount, Charles; Ferraro, Daniel; Gru, Alejandro; Bradbury, Matthew; Cornelius, Lynn; and Gay, Hiram, ,"Treatment of pagetoid reticulosis with intensity modulated radiation therapy." Dermatology Online Journal.20,10. (2014). https://digitalcommons.wustl.edu/open_access_pubs/5149 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. Authors Charles Mount, Daniel Ferraro, Alejandro Gru, Matthew Bradbury, Lynn Cornelius, and Hiram Gay This open access publication is available at Digital Commons@Becker: https://digitalcommons.wustl.edu/open_access_pubs/5149 Dermatology Online Journal UC Davis Peer Reviewed Title: Treatment of pagetoid reticulosis with intensity modulated radiation therapy Journal Issue: Dermatology Online Journal, 20(10) Author: Mount, Charles, Washington University in St. Louis Ferraro, Daniel, Washington University in St. Louis Gru, Alejandro, Washington University in St. Louis; The Ohio State University Bradbury, Matthew, Washington University in St. Louis Cornelius, Lynn, Washington University in St. -

Histopathological Reporting of Malignant Lymphoma
Malaysian J Path01 1999; 21(1): 63 - 67 CONSENSUS REPORT Histopathological reporting of malignant lymphoma Suat-Cheng Peh and *Sibrand Poppema Chairman and *invited consultant, Organizing Committee, Slide Seminar-cum-Workshop on Malignant Lymphoma 1999 A consensus on histopathology reporting of malignant lymphoma was reached at the "Slide Seminar- cum-Workshop on Malignant Lymphoma," jointly organized by the Malaysian Society of Pathologists and the Department of Pathology, Faculty of Medicine, University of Malaya on 29 -30 April, 1999. I. CLASSIFICATION It was agreed that the newly proposed World Health Organization classification of Neoplastic Diseases of Hematopoietic and Lymphoid Tissue will be adopted (Table 1). Individual institutions may in addition include in their reports the classification currently in use in these centres in the initial phase, until clinicians are familiar with the entities listed in the WHO classification. 11. IMMUNOHISTOCHEMISTRY It was also agreed that immunohistological investigation is frequently essential for a correct lymphoma diagnosis. The following was recommended for the study on paraffin-embedded biopsy material: a. Panel of antibodies for routine application: CD20 (L26) or CD79a CD3 (polyclonal CD3) or CD43 (MT1) CD45RO (UCHL1) Kappa and Lambda light chains b. Panel of useful additional antibodies: CD15 CD30 CD45 (LCA) S loo CD68 Cytokeratin Bcl-2 Vimentin c. Others: CD5 CD21 CD23 CD56 ALK Malaysiun J Pathol June 1999 111. THE HISTOPATHOLOGY REPORT The following items should be included in the histology report: 1. Identification: Whether biopsy material is nodal or extra-nodal tissue. 2. Description of the lesion: i. Whether normal structure is preserved ii. Describe the pattern of architectural distortion, e.g. -

Mycosis Fungoides and Sézary Syndrome: an Integrative Review of the Pathophysiology, Molecular Drivers, and Targeted Therapy
cancers Review Mycosis Fungoides and Sézary Syndrome: An Integrative Review of the Pathophysiology, Molecular Drivers, and Targeted Therapy Nuria García-Díaz 1 , Miguel Ángel Piris 2,† , Pablo Luis Ortiz-Romero 3,† and José Pedro Vaqué 1,*,† 1 Molecular Biology Department, Universidad de Cantabria—Instituto de Investigación Marqués de Valdecilla, IDIVAL, 39011 Santander, Spain; [email protected] 2 Department of Pathology, Fundación Jiménez Díaz, CIBERONC, 28040 Madrid, Spain; [email protected] 3 Department of Dermatology, Hospital 12 de Octubre, Institute i+12, CIBERONC, Medical School, University Complutense, 28041 Madrid, Spain; [email protected] * Correspondence: [email protected] † Same contribution. Simple Summary: In the last few years, the field of cutaneous T-cell lymphomas has experienced major advances. In the context of an active translational and clinical research field, next-generation sequencing data have boosted our understanding of the main molecular mechanisms that govern the biology of these entities, thus enabling the development of novel tools for diagnosis and specific therapy. Here, we focus on mycosis fungoides and Sézary syndrome; we review essential aspects of their pathophysiology, provide a rational mechanistic interpretation of the genomic data, and discuss the current and upcoming therapies, including the potential crosstalk between genomic alterations Citation: García-Díaz, N.; Piris, M.Á.; and the microenvironment, offering opportunities for targeted therapies. Ortiz-Romero, P.L.; Vaqué, J.P. Mycosis Fungoides and Sézary Abstract: Primary cutaneous T-cell lymphomas (CTCLs) constitute a heterogeneous group of diseases Syndrome: An Integrative Review of that affect the skin. Mycosis fungoides (MF) and Sézary syndrome (SS) account for the majority the Pathophysiology, Molecular of these lesions and have recently been the focus of extensive translational research. -

A Patient's Guide to Understanding Cutaneous Lymphoma
WELCOME! If you or someone close to you has been given a diagnosis of cutaneous lymphoma, you probably have many questions and concerns. Living with cutaneous lymphoma and the many changes that this diagnosis brings to your life can leave you feeling overwhelmed, confused and lonely. You may not even be sure about what kinds of questions to ask. This guide was created so you can find valuable information to help you understand the disease, learn about available treatments and how to find specialists, access support, and ways to live the best life you can with cutaneous lymphoma. The Cutaneous Lymphoma Foundation is dedicated to providing patients, caregivers and loved ones with programs and services designed to help, support and provide hope to people who are given a diagnosis of cutaneous lymphoma. We are here for you. You are not alone. You are part of a knowledgeable, caring, resourceful, and compassionate community, and we’re here to help you. Get in touch anytime. We hope to hear from you or meet you in person at one of our patient events. We wish you all the best in your journey. The Staff and Board of Directors of the Cutaneous Lymphoma Foundation A Patient’s Guide to Understanding Cutaneous Lymphoma ACKNOWLEDGMENTS This guide is an educational resource published by the Cutaneous Lymphoma The Cutaneous Lymphoma Foundation acknowledges and thanks the Foundation providing general information on cutaneous lymphoma. Publication individuals listed below who have given generously of their time and expertise. of this information is not intended to take the place of medical care or the advice We thank them for their contributions, editorial wisdom and advice, which have of your physician(s). -

Patch, Plaque, Tumour - Mycosis Fungoides Anubha Bajaj*
Review Article iMedPub Journals Journal of Neoplasm 2018 www.imedpub.com ISSN 2576-3903 Vol.3 No.2:33 DOI: 10.21767/2576-3903.100033 Patch, Plaque, Tumour - Mycosis Fungoides Anubha Bajaj* Department of Histopathology, A.B. Diagnostics, India Abstract Corresponding author: Anubha Bajaj Mycosis fungoides is a frequent cutaneous lymphoma contributing to an estimated half (50%) of the emerging dermal lymphomas. As an epidermotropic primary [email protected] cutaneous T lymphoma (CTCL), it may comprise of miniature or medium sized lymphocytes containing cerebriform nuclei and a T helper cell immune phenotype, Consultant, Department of Histopathology, although variants of a cytotoxic T lymphocyte (CTL) component may commonly A.B. Diagnostics, India. arise. “Mycosis Fungoides “as a terminology is restricted to classical manifestation of a disorder characterized by the appearance of patches, plaques and tumours or Tel: +919811693956 the diverse cutaneous disorders with an identical clinical evolution. The prevalence of mycosis fungoides is at an estimated 60% of cutaneous tumours, though the incidence may be augmented in the Africans. The lesions may depict a prominent Citation: Bajaj A (2018) Patch, Plaque, regional variability. Elderly and adult individuals may be frequently incriminated Tumour - Mycosis Fungoides. J Neoplasm. with a male predominance (M:F: 2:1), although children and adolescents may Vol.3 No.2:33 similarly manifest the cutaneous lymphoma Keywords: Mycosis fungoides; Lymphoma; Chronic dermatosis; Cutaneous Received: October 10, 2018; Accepted: November 02, 2018; Published: November 05, 2018 Introduction lesions predominantly arising in the sun protected zones, especially buttocks and the female breasts. A variable scaling Mycosis fungoides is a condition of obscure aetiology. -

Download This PDF File
Journal of Tumor Online Submissions: http://www.ghrnet.org/index.php/jt Journal of Tumor 2020 May; 8(1): 555-559 10.17554/j.issn.1819-6187.2020.08.119 ISSN 1819-6187 CASE REPORT Long-standing CD4+/CD8+ Woringer-Kolopp Disease: A Report of A Rare Case Sin Siuew Lim1, Zuliatul Faizah Baharom1, A Mohd Affandi2 1 Department of Pathology, Hospital Kuala Lumpur, Jalan Pahang, CD8. Other relevant immunostains were negative. The proliferative Wilayah Persekutuan, 50586 Kuala Lumpur, Malaysia; index is high (> 80%). MRI of the right leg shows suspicious regional 2 Department of Dermatology, Hospital Kuala Lumpur, Jalan Pahang, tendon involvement. Staging CT scan shows no disseminated disease. Wilayah Persekutuan, 50586 Kuala Lumpur, Malaysia. No atypical lymphocytes seen in peripheral blood smear. Infective screenings are negative. Conflict-of-interest statement: The author(s) declare(s) that there DISCUSSION: PR is an indolent disease with excellent prognosis is no conflict of interest regarding the publication of this paper. as opposed to primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma (PCACTL), its disseminated form. Open-Access: This article is an open-access article which was Histopathologically, PR has to be distinguished from conditions selected by an in-house editor and fully peer-reviewed by external which are associated with pagetoid epidermotropic growth and other reviewers. It is distributed in accordance with the Creative Com- acral presentations of T-cell lymphomas such as MF palmaris et mons Attribution Non Commercial (CC BY-NC 4.0) license, which plantaris (MFPEP), PCACTL and Type-D lymphomatoid papulosis permits others to distribute, remix, adapt, build upon this work non- (LP-D). -

Mycosis Fungoides and Sézary Syndrome: Focus on The
Anais Brasileiros de Dermatologia 2021;96(4):458---471 Anais Brasileiros de Dermatologia www.anaisdedermatologia.org.br REVIEW Mycosis fungoides and Sézary syndrome: focus on the ଝ,ଝଝ current treatment scenario a,∗ a b José Antonio Sanches , Jade Cury-Martins , Rodrigo Martins Abreu , a c Denis Miyashiro , Juliana Pereira a Dermatology Clinic Division, Faculty of Medicine, Hospital das Clínicas, Universidade de São Paulo, São Paulo, SP, Brazil b Medical Department, Private Institution, São Paulo, SP, Brazil c Hematology Clinic Division, Faculty of Medicine, Hospital das Clínicas, Universidade de São Paulo, São Paulo, SP, Brazil Received 2 October 2020; accepted 6 December 2020 Available online 28 May 2021 Abstract Cutaneous T-cell lymphomas are a heterogeneous group of lymphoproliferative dis- KEYWORDS orders, characterized by infiltration of the skin by mature malignant T cells. Mycosis fungoides Lymphoma, T-cell, is the most common form of cutaneous T-cell lymphoma, accounting for more than 60% of cases. cutaneous; Mycosis fungoides in the early-stage is generally an indolent disease, progressing slowly from Mycosis fungoides; some patches or plaques to more widespread skin involvement. However, 20% to 25% of patients Sezary syndrome; progress to advanced stages, with the development of skin tumors, extracutaneous spread and Therapeutics poor prognosis. Treatment modalities can be divided into two groups: skin-directed therapies and systemic therapies. Therapies targeting the skin include topical agents, phototherapy and radiotherapy. Systemic therapies include biological response modifiers, immunotherapies and chemotherapeutic agents. For early-stage mycosis fungoides, skin-directed therapies are pre- ferred, to control the disease, improve symptoms and quality of life. When refractory or in advanced-stage disease, systemic treatment is necessary.