Ulnarneur.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Occupational Therapy Guide for Entry
University of North Dakota UND Scholarly Commons Occupational Therapy Capstones Department of Occupational Therapy 2008 An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries Ryan Edwards University of North Dakota Follow this and additional works at: https://commons.und.edu/ot-grad Part of the Occupational Therapy Commons Recommended Citation Edwards, Ryan, "An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries" (2008). Occupational Therapy Capstones. 57. https://commons.und.edu/ot-grad/57 This Scholarly Project is brought to you for free and open access by the Department of Occupational Therapy at UND Scholarly Commons. It has been accepted for inclusion in Occupational Therapy Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. AN OCCUPATIONAL THERAPY GUIDE FOR ENTRY-LEVEL THERAPISTS NOT SPECIALIZING IN THE TREATMENT OF UPPER EXTREMITY DYSFUNCTION: THREE COMMON CUMULATIVE TRAUMA INJURIES by Ryan Edwards Advisor: Anne Haskins PhD, OTR/L A Scholarly Project Submitted to the Occupational Therapy Department of the University of North Dakota In partial fulfillment of the requirements for the degree of Master’s of Occupational Therapy Grand Forks, North Dakota August 1, 2008 This Scholarly Project Paper, submitted by Ryan Edwards in partial fulfillment of the requirement for the Degree of Master’s of Occupational Therapy from the University of North Dakota, has been read by the Faculty Advisor under whom the work has been done and is hereby approved. -

An Improved Technique for Radial Nerve Conduction Studies
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.30.4.332 on 1 August 1967. Downloaded from J. Neurol. Neurosurg. Psychiat., 1967, 30, 332 An improved technique for radial nerve conduction studies ALLAN W. DOWNIE1 AND THOMAS R. SCOTT From the Division of Neurology, Department of Medicine, School of Medicine, University ofNorth Carolina, Chapel Hill, North Carolina, U.S.A. A technique for recording evoked sensory potentials MATERIALS AND METHOD from the radial nerve has already been reported by us (Downie and Scott, 1964). This technique, The apparatus used was a TECA two-channel electro- myograph. The recording electrodes consisted of a pair although reliable, is time consuming and occasion- of chlorided silver discs 1 cm. in diameter, mounted ally difficult and the amplitude of potentials may be 2 5 cm. apart on a plastic base. The active recording as low as 1 to 2 microvolts. The purpose of this electrode was placed over the largest palpable branch communication is to describe a simpler technique by of the radial nerve as it crossed the tendon of the extensor which potentials of greater amplitude can be pollicis longus. The distal recording electrode was placed obtained. In addition, the segment of nerve tested is over the first dorsal interosseous muscle but not neces- Protected by copyright. one which can be readily identified and biopsied if sarily over the nerve, of which the position in this area so desired without causing unpleasant or disturbing cannot be precisely determined (Fig. 1). An experiment sensory loss to the subject. made to assess the importance of the position of this electrode showed no significant difference in latency to The location of a nerve which is to be tested is peak when it was placed in turn on three points along usually determined by stimulating its motor fibres a line between the tendons of the extensor pollicis and finding the stimulus site from which maximal longus and extensor indicis provided the interelectrode muscle contraction is obtained. -

Ultrasound of Radial, Ulnar, and Median Nerves
Ultrasound of Radial, Ulnar, Disclosures • Consultant: Bioclinica and Median Nerves • Contractor: POCUS PRO • Advisory Board: Philips Jon A. Jacobson, M.D. • Book Royalties: Elsevier • Not relevant to this lecture Professor of Radiology See www.jacobsonmskus.com for syllabus other educational material Nerve Compression Nerve Entrapment • Experimental model (rat, sciatic nv): • US findings: – Compression causes ischemia – Nerve enlargement proximal to entrapment – First pathologic change: edema • Best appreciated transverse to nerve • Correlated with severity of axonal injury – Abnormally hypoechoic – Mild compression: demyelination • Especially the connective tissue layers – Severe compression: axonal damage – Variable enlargement or flattening at entrapment site Powell, Laboratory Investigation 1986; 55:91 Atrophy Denervation Nerve Entrapment Syndromes • Edema: hyperechoic • Fatty degeneration: • Median: – Hyperechoic – Carpal tunnel syndrome – Echogenic interfaces – Pronator teres syndrome • Atrophy: Asymptomatic – Hyperechoic with • Ulnar: decreased muscle size – Ulnar tunnel syndrome • Compare to other side! – Cubital tunnel syndrome J Ultrasound Med 1993; 2:73 Extensor Muscles: leg 1 Volar Wrist Normal Peripheral Nerve • Ultrasound appearance: – Hypoechoic nerve fascicles – Hyperechoic connective tissue • Transverse: – Honeycomb appearance Silvestri et al. Radiology 1995; 197:291 Median Nerve From: Netter’s Atlas of Human Anatomy Volar Wrist: median nerve & flexors Peripheral Nerves • More coarse compared to tendon T – Fascicular -

Neuropathy, Radiculopathy & Myelopathy
Neuropathy, Radiculopathy & Myelopathy Jean D. Francois, MD Neurology & Neurophysiology Purpose and Objectives PURPOSE Avoid Confusing Certain Key Neurologic Concepts OBJECTIVES • Objective 1: Define & Identify certain types of Neuropathies • Objective 2: Define & Identify Radiculopathy & its causes • Objective 3: Define & Identify Myelopathy FINANCIAL NONE DISCLOSURE Basics What is Neuropathy? • The term 'neuropathy' is used to describe a problem with the nerves, usually the 'peripheral nerves' as opposed to the 'central nervous system' (the brain and spinal cord). It refers to Peripheral neuropathy • It covers a wide area and many nerves, but the problem it causes depends on the type of nerves that are affected: • Sensory nerves (the nerves that control sensation>skin) causing cause tingling, pain, numbness, or weakness in the feet and hands • Motor nerves (the nerves that allow power and movement>muscles) causing weakness in the feet and hands • Autonomic nerves (the nerves that control the systems of the body eg gut, bladder>internal organs) causing changes in the heart rate and blood pressure or sweating • It May produce Numbness, tingling,(loss of sensation) along with weakness. It can also cause pain. • It can affect a single nerve (mononeuropathy) or multiple nerves (polyneuropathy) Neuropathy • Symptoms usually start in the longest nerves in the body: Feet & later on the hands (“Stocking-glove” pattern) • Symptoms usually spread slowly and evenly up the legs and arms. Other body parts may also be affected. • Peripheral Neuropathy can affect people of any age. But mostly people over age 55 • CAUSES: Neuropathy has a variety of forms and causes. (an injury systemic illness, an infection, an inherited disorder) some of the causes are still unknown. -

Hereditary Spastic Paraparesis: a Review of New Developments
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.69.2.150 on 1 August 2000. Downloaded from 150 J Neurol Neurosurg Psychiatry 2000;69:150–160 REVIEW Hereditary spastic paraparesis: a review of new developments CJ McDermott, K White, K Bushby, PJ Shaw Hereditary spastic paraparesis (HSP) or the reditary spastic paraparesis will no doubt Strümpell-Lorrain syndrome is the name given provide a more useful and relevant classifi- to a heterogeneous group of inherited disorders cation. in which the main clinical feature is progressive lower limb spasticity. Before the advent of Epidemiology molecular genetic studies into these disorders, The prevalence of HSP varies in diVerent several classifications had been proposed, studies. Such variation is probably due to a based on the mode of inheritance, the age of combination of diVering diagnostic criteria, onset of symptoms, and the presence or other- variable epidemiological methodology, and wise of additional clinical features. Families geographical factors. Some studies in which with autosomal dominant, autosomal recessive, similar criteria and methods were employed and X-linked inheritance have been described. found the prevalance of HSP/100 000 to be 2.7 in Molise Italy, 4.3 in Valle d’Aosta Italy, and 10–12 Historical aspects 2.0 in Portugal. These studies employed the In 1880 Strümpell published what is consid- diagnostic criteria suggested by Harding and ered to be the first clear description of HSP.He utilised all health institutions and various reported a family in which two brothers were health care professionals in ascertaining cases aVected by spastic paraplegia. The father was from the specific region. -

A Guide to Transthyretin Amyloidosis
A Guide to Transthyretin Amyloidosis Authored by Teresa Coelho, Bo-Goran Ericzon, Rodney Falk, Donna Grogan, Shu-ichi Ikeda, Mathew Maurer, Violaine Plante-Bordeneuve, Ole Suhr, Pedro Trigo 2016 Edition Edited by Merrill Benson, Mathew Maurer What is amyloidosis? Amyloidosis is a systemic disorder characterized by extra cellular deposition of a protein-derived material, known as amyloid, in multiple organs. Amyloidosis occurs when native or mutant poly- peptides misfold and aggregate as fibrils. The amyloid deposits cause local damage to the cells around which they are deposited leading to a variety of clinical symptoms. There are at least 23 different proteins associated with the amyloidoses. The most well-known type of amyloidosis is associated with a hematological disorder, in which amyloid fibrils are derived from monoclonal immunoglobulin light-chains (AL amyloidosis). This is associated with a clonal plasma cell disorder, closely related to and not uncommonly co-existing with multiple myeloma. Chronic inflammatory conditions such as rheumatoid arthritis or chronic infections such as bronchiectasis are associated with chronically elevated levels of the inflammatory protein, serum amyloid A, which may misfold and cause AA amyloidosis. The hereditary forms of amyloidosis are autosomal dominant diseases characterized by deposition of variant proteins, in dis- tinctive tissues. The most common hereditary form is transthyretin amyloidosis (ATTR) caused by the misfolding of protein monomers derived from the tetrameric protein transthyretin (TTR). Mutations in the gene for TTR frequently re- sult in instability of TTR and subsequent fibril formation. Closely related is wild-type TTR in which the native TTR protein, particu- larly in the elderly, can destabilize and re-aggregate causing non- familial cases of TTR amyloidosis. -

Ultrasound of Peripheral Nerve and Muscle
ULTRASOUND OF PERIPHERAL NERVE AND MUSCLE Steven Shook, MD Cleveland Clinic Cleveland, OH INTRODUCTION Advances in field of ultrasound over the past twenty years have generated increasing interest in utilizing the technology in neuromuscular assessment and diagnosis. High-resolution ultrasound offers a noninvasive, real- time, static and dynamic examination of the peripheral nervous system, yielding information which complements the neurological examination, electrodiagnostic testing (EDX), and other established imaging modalities such as Magnetic Resonance Imaging (MRI). ULTRASOUND BASICS Ultrasonography involves transmitting sound-wave pulses into tissue and analyzing the temporal and acoustic properties of the reflected wave, or echo. Echoes occur at tissue interfaces. Reflected energy is a product of the difference in adjacent tissue densities (acoustic impedance), as well the angle of the ultrasound beam (angle of incidence) relative to the interface.(1) A fraction of a transmitted sound-wave energy is reflected whenever there is a change in acoustic impedance within tissue. Larger differences in acoustic impedance result in more profound reflection. Unreflected sound travels deeper into the tissue, generating echos from layers at a greater depth. A portion of the ultrasound energy never returns to the transducer, either being transformed into heat (absorption), refracted or scattered at nonperpendicular tissue interfaces. When the sound wave encounters a significantly different tissue density, analysis of deeper structures is not possible. For example, ultrasound cannot evaluate structures deep to air- filled cavities or bone due to the acoustic impedance of these regions.(2) An ultrasound probe (transducer) is capable of both emitting and receiving these pulses and converting them into electrical signals for analysis. -

Expert Consensus Recommendations to Improve Diagnosis of ATTR Amyloidosis with Polyneuropathy
Journal of Neurology https://doi.org/10.1007/s00415-019-09688-0 REVIEW Expert consensus recommendations to improve diagnosis of ATTR amyloidosis with polyneuropathy David Adams1 · Yukio Ando2 · João Melo Beirão3 · Teresa Coelho4 · Morie A. Gertz5 · Julian D. Gillmore6 · Philip N. Hawkins6 · Isabelle Lousada7 · Ole B. Suhr8 · Giampaolo Merlini9,10 Received: 10 December 2019 / Revised: 20 December 2019 / Accepted: 23 December 2019 © The Author(s) 2020 Abstract Amyloid transthyretin (ATTR) amyloidosis with polyneuropathy (PN) is a progressive, debilitating, systemic disease wherein transthyretin protein misfolds to form amyloid, which is deposited in the endoneurium. ATTR amyloidosis with PN is the most serious hereditary polyneuropathy of adult onset. It arises from a hereditary mutation in the TTR gene and may involve the heart as well as other organs. It is critical to identify and diagnose the disease earlier because treatments are available to help slow the progression of neuropathy. Early diagnosis is complicated, however, because presentation may vary and family history is not always known. Symptoms may be mistakenly attributed to other diseases such as chronic infammatory demyelinating polyradiculoneuropathy (CIDP), idiopathic axonal polyneuropathy, lumbar spinal stenosis, and, more rarely, diabetic neuropathy and AL amyloidosis. In endemic countries (e.g., Portugal, Japan, Sweden, Brazil), ATTR amyloidosis with PN should be suspected in any patient who has length-dependent small-fber PN with autonomic dysfunction and a family history of ATTR amyloidosis, unexplained weight loss, heart rhythm disorders, vitreous opacities, or renal abnormali- ties. In nonendemic countries, the disease may present as idiopathic rapidly progressive sensory motor axonal neuropathy or atypical CIDP with any of the above symptoms or with bilateral carpal tunnel syndrome, gait disorders, or cardiac hypertro- phy. -

Hereditary Spastic Paraplegia
8 Hereditary Spastic Paraplegia Notes and questions Hereditary Spastic Paraplegia What is Hereditary Spastic Paraplegia? Hereditary Spastic Paraplegia (HSP) is a medical term for a condition that affects muscle function. The terms spastic and paraplegia comes from several words in Greek: • ‘spastic’ means afflicted with spasms (an alteration in muscle tone that results in affected movements) • ‘paraplegia’ meaning an impairment in motor or sensory function of the lower extremities (from the hips down) What are the signs and symptoms of HSP? Muscular spasticity • Individuals with HSP commonly will have lower extremity weakness, spasticity, and muscle stiffness. • This can cause difficulty with walking or a “scissoring” gait. We are grateful to an anonymous donor for making a kind and Other common signs or symptoms include: generous donation to the Neuromuscular and Neurometabolic Centre. • urinary urgency • overactive or over responsive “brisk” reflexes © Hamilton Health Sciences, 2019 PD 9983 – 01/2019 Dpc/pted/HereditarySpasticParaplegia-trh.docx dt/January 15, 2019 ____________________________________________________________________________ 2 7 Hereditary Spastic Paraplegia Hereditary Spastic Paraplegia HSP is usually a chronic or life-long disease that affects If you have any questions about DM1, please speak with your people in different ways. doctor, genetic counsellor, or nurse at the Neuromuscular and Neurometabolic Centre. HSP can be classified as either “Uncomplicated HSP” or “Complicated HSP”. Notes and questions Types of Hereditary Spastic Paraplegia 1. Uncomplicated HSP: • Individuals often experience difficulty walking as the first symptom. • Onset of symptoms can begin at any age, from early childhood through late adulthood. • Symptoms may be non-progressive, or they may worsen slowly over many years. -
Practical Neurology: Peripheral Neuropathy for the Internist
Practical Neurology: Polyneuropathy for the Non-Neurologist Steven A. Day, MD Providence Neurological Specialties Definitions Foundational Principle: With neurological problems think of LOCALIZATION before SYNDROME Definitions • Neuronopathy – Motor neuronopathy – Sensory neuronopathy • Radiculopathy • Plexopathy • Neuropathy – Mononeuropathy – Polyneuropathy The Netter Collection of Medical Illustrations, Volume 1, Nervous System, 2002 “ROOTS” C4 TRUNKS C5 Dorsal scapular n. C6 TRUNKS C7 Suprascapular n. T1 DIVISIONS Musculocut- aneous n. CCF CORDS 2002 Long thoracic n. TERMINAL NERVES CCF ©2002 Axillary n. Radial n. Median n. Ulnar n. Definitions ‘Neuropathy’ is a diagnosis which specifies the location of pathology, not a symptom Definitions • Axonal = axon loss pathology • Demyelinating = myelin loss pathology Topical Diagnosis in Neurology, 3rd ed. 1998 Topical Diagnosis in Neurology, 3rd ed. 1998 Duss’ Topical Diagnosis in Neurology, 4th ed. 2005 Polyneuropathy Polyneuropathy: Typical Presentation • Insidious onset • Distal (toes, pads of feet) • Gradual progression • Complaints are primarily sensory Polyneuropathy: Key Exam Features • Sensory – Distal gradient of sensory loss • Pin prick or cold • Monofilament • Cotton wisp • Vibration at toes and ankles • Proprioception: toe movements Polyneuropathy: Key Exam Features • Motor – Is there intrinsic foot or hand muscle atrophy? – Weakness pattern • Distal • Proximal and distal • Asymmetric – Able to stand/elevate on toes and heels? Polyneuropathy: Key Exam Features • Reflexes – Distal -
Peripheral Neuropathy
Peripheral Neuropathy U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health Peripheral Neuropathy What is peripheral neuropathy? n estimated 20 million people in A the United States have some form of peripheral neuropathy, a condition that develops as a result of damage to the peripheral nervous system — the vast communications network that transmits information between the central nervous system (the brain and spinal cord) and every other part of the body. (Neuropathy means nerve disease or damage.) Symptoms can range from numbness or tingling, to pricking sensations (paresthesia), or muscle weakness. Areas of the body may become abnormally sensitive leading to an exaggeratedly intense or distorted experience of touch (allodynia). In such cases, pain may occur in response to a stimulus that does not normally provoke pain. Severe symptoms may include burning pain (especially at night), muscle wasting, paralysis, or organ or gland dysfunction. Damage to nerves that supply internal organs may impair digestion, sweating, sexual function, and urination. In the most extreme cases, breathing may become difficult, or organ failure may occur. Peripheral nerves send sensory information back to the brain and spinal cord, such as a message that the feet are cold. Peripheral 1 nerves also carry signals from the brain and spinal cord to the muscles to generate movement. Damage to the peripheral nervous system interferes with these vital connections. Like static on a telephone line, peripheral neuropathy distorts and sometimes interrupts messages between the brain and spinal cord and the rest of the body. Peripheral neuropathies can present in a variety of forms and follow different patterns. -
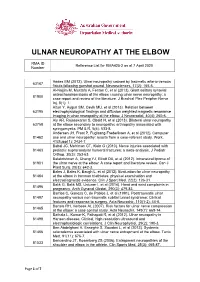
Reference List for RMA425-2 As at 7 April 2020 Number
ULNAR NEUROPATHY AT THE ELBOW RMA ID Reference List for RMA425-2 as at 7 April 2020 Number Addas BM (2012). Ulnar neuropathy caused by traumatic arterio-venous 63167 fistula following gunshot wound. Neurosciences, 17(2): 165-6. Al-Najjim M, Mustafa A, Fenton C, et al (2013). Giant solitary synovial osteochondromatosis of the elbow causing ulnar nerve neuropathy: a 81900 case report and review of the literature. J Brachial Plex Peripher Nerve Inj, 8(1): 1. Altun Y, Aygun SM, Cevik MU, et al (2013). Relation between 63195 electrophysiological findings and diffusion weighted magnetic resonance imaging in ulnar neuropathy at the elbow. J Neuroradiol, 40(4): 260-6. Aly AR, Rajasekaran S, Obaid H, et al (2013). Bilateral ulnar neuropathy 63758 at the elbow secondary to neuropathic arthropathy associated with syringomyelia. PM & R, 5(6): 533-8. Andersen JH, Frost P, Fuglsang-Frederiksen A, et al (2012). Computer 81462 use and ulnar neuropathy: results from a case-referent study. Work, 41(Suppl 1): 2434-7. Babal JC, Mehlman CT, Klein G (2010). Nerve injuries associated with 81463 pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop, 30(3): 253-63. Balakrishnan A, Chang YJ, Elliott DA, et al (2012). Intraneural lipoma of 81901 the ulnar nerve at the elbow: A case report and literature review. Can J Plast Surg, 20(3): e42-3. Bales J, Bales K, Baugh L, et al (2012). Evaluation for ulnar neuropathy 81464 at the elbow in Ironman triathletes: physical examination and electrodiagnostic evidence. Clin J Sport Med, 22(2): 126-31. Balik G, Balik MS, Ustuner I, et al (2014).