Program Supported by Malaria Consortium in Burkina Faso, A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Givedirectly
GiveDirectly GiveDirectly provides unconditional cash transfers using cell phone technology to some of the world’s poorest people, as well as refugees, urban youth, and disaster victims. They also are currently running a historic Universal Basic Income initiative, delivering a basic income to 20,000+ people in Kenya in a 12-year study. United States (USD) Donate to GiveDirectly Please select your country & currency. Donations are tax-deductible in the country selected. Founded in Moved Delivered cash to 88% of donations sent to families 2009 US$140M 130K in poverty families Other ways to donate We recommend that gifts up to $1,000 be made online by credit card. If you are giving more than $1,000, please consider one of these alternatives. Check Bank Transfer Donor Advised Fund Cryptocurrencies Stocks or Shares Bequests Corporate Matching Program The problem: traditional methods of international giving are complex — and often inefficient Often, donors give money to a charity, which then passes along the funds to partners at the local level. This makes it difficult for donors to determine how their money will be used and whether it will reach its intended recipients. Additionally, charities often provide interventions that may not be what the recipients actually need to improve their lives. Such an approach can treat recipients as passive beneficiaries rather than knowledgeable and empowered shapers of their own lives. The solution: unconditional cash transfers Most poverty relief initiatives require complicated infrastructure, and alleviate the symptoms of poverty rather than striking at the source. By contrast, unconditional cash transfers are straightforward, providing funds to some of the poorest people in the world so that they can buy the essentials they need to set themselves up for future success. -

Cost-Effectiveness of District-Wide Seasonal
Diawara et al. Malar J (2021) 20:128 https://doi.org/10.1186/s12936-021-03653-x Malaria Journal RESEARCH Open Access Cost-efectiveness of district-wide seasonal malaria chemoprevention when implemented through routine malaria control programme in Kita, Mali using fxed point distribution Halimatou Diawara1* , Patrick Walker2, Matt Cairns3, Laura C. Steinhardt4, Fatou Diawara1, Beh Kamate5, Laeticia Duval2, Elisa Sicuri2, Issaka Sagara1, Aboubacar Sadou6, Jules Mihigo7, Erin Eckert8, Alassane Dicko1 and Lesong Conteh9 Abstract Background: Seasonal malaria chemoprevention (SMC) is a strategy for malaria control recommended by the World Health Organization (WHO) since 2012 for Sahelian countries. The Mali National Malaria Control Programme adopted a plan for pilot implementation and nationwide scale-up by 2016. Given that SMC is a relatively new approach, there is an urgent need to assess the costs and cost efectiveness of SMC when implemented through the routine health system to inform decisions on resource allocation. Methods: Cost data were collected from pilot implementation of SMC in Kita district, which targeted 77,497 children aged 3–59 months. Starting in August 2014, SMC was delivered by fxed point distribution in villages with the frst dose observed each month. Treatment consisted of sulfadoxine-pyrimethamine and amodiaquine once a month for four consecutive months, or rounds. Economic and fnancial costs were collected from the provider perspective using an ingredients approach. Efectiveness estimates were based upon a published mathematical transmission model calibrated to local epidemiology, rainfall patterns and scale-up of interventions. Incremental cost efectiveness ratios were calculated for the cost per malaria episode averted, cost per disability adjusted life years (DALYs) averted, and cost per death averted. -
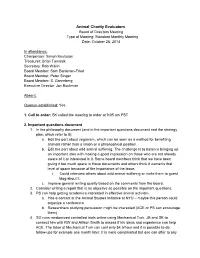
October 26, 2014
Animal Charity Evaluators Board of Directors Meeting Type of Meeting: Standard Monthly Meeting Date: October 26, 2014 In attendance: Chairperson: Simon Knutsson Treasurer: Brian Tomasik Secretary: Rob Wiblin Board Member: Sam BankmanFried Board Member: Peter Singer Board Member: S. Greenberg Executive Director: Jon Bockman Absent: Quorum established: Yes 1. Call to order: SK called the meeting to order at 9:05 am PST 2. Important questions document 1. In the philosophy document (and in the important questions document and the strategy plan, which refer to it): a. Edit the part about veganism, which can be seen as a method for benefiting animals rather than a vision or a philosophical position. b. Edit the part about wild animal suffering. The challenge is to balance bringing up an important idea with making a good impression on those who are not already aware of it or interested in it. Some board members think that we have been giving it too much space in these documents and others think it warrants that level of space because of the importance of the issue. i. Could interview others about wild animal suffering or invite them to guest blog about it. c. Improve general writing quality based on the comments from the board. 2. Consider writing a report that is as objective as possible on the important questions. 3. PS can help getting academics interested in effective animal activism. a. Has a contact at the Animal Studies Initiative at NYU – maybe this person could organize a conference b. Researchers studying persuasion might be interested (ACE or PS can encourage them) 4. -

Against 'Effective Altruism'
Against ‘Effective Altruism’ Alice Crary Effective Altruism (EA) is a programme for rationalising for the most part adopt the attitude that they have no charitable giving, positioning individuals to do the ‘most serious critics and that sceptics ought to be content with good’ per expenditure of money or time. It was first for- their ongoing attempts to fine-tune their practice. mulated – by two Oxford philosophers just over a decade It is a posture belied by the existence of formidable ago–as an application of the moral theory consequential- critical resources both inside and outside the philosoph- ism, and from the outset one of its distinctions within ical tradition in which EA originates. In light of the undis- the philanthropic world was expansion of the class of puted impact of EA, and its success in attracting idealistic charity-recipients to include non-human animals. EA young people, it is important to forcefully make the case has been the target of a fair bit of grumbling, and even that it owes its success primarily not to the – question- some mockery, from activists and critics on the left, who able – value of its moral theory but to its compatibility associate consequentialism with depoliticising tenden- with political and economic institutions responsible for cies of welfarism. But EA has mostly gotten a pass, with some of the very harms it addresses. The sincere ded- many detractors concluding that, however misguided, its ication of many individual adherents notwithstanding, efforts to get bankers, tech entrepreneurs and the like to reflection on EA reveals a straightforward example of give away their money cost-effectively does no serious moral corruption. -

EA Course: Overview and Future Plans
EA Course: Overview and Future Plans Note: I encourage you to first read the One Page Summary at the bottom and then skip to the sections you’re interested in. ❖ Background ❖ Goals ➢ For the class ➢ For the club ➢ Ideal student ❖ Class Structure ➢ Basics ➢ Giving games ➢ Final project ➢ Potential changes ❖ Course Content ❖ Advertising and Recruiting ❖ Speakers ❖ Financial Management ➢ Banking ➢ Sources of Money ➢ Financial management issues ■ Communication Issues ■ Payment Issues ■ Reimbursement Issues ➢ Potential changes ❖ Website ❖ Final Project ➢ Goals ➢ Winning project ➢ Potential changes ❖ Evidence of Impact ➢ Collection ➢ Outcomes ➢ Potential changes ❖ Future Plans ❖ Funding Goals ❖ One Page Summary Background ● Oliver Habryka and I taught a studentled class (“DeCal”) during the Spring 2015 semester at UC Berkeley called The Greater Good, on effective altruism ● The class was taught under the banner of Effective Altruists of Berkeley, a student organization we founded the previous semester ● Overall, I think it was a success and satisfied most of our initial goals (details below) Goals ● Goals for the class: ○ Primarily, we wanted to recruit people for our newly created Effective Altruists of Berkeley club ■ Having to engage with/debate EA for a semester beforehand would allow people to really understand if they wanted to become involved in it ■ It would also allow them to contribute to the club’s projects without having to be given a whole lot of background first ■ We also felt that going through a class together first would -

Givewell NYC Research Event, December 14, 2015 – Top Charities
GiveWell NYC Research Event, December 14, 2015 – Top Charities GiveWell NYC Research Event, December 14, 2015 – Top Charities GiveWell NYC Research Event, December 14, 2015 – Top Charities This transcript was compiled by an outside contractor, and GiveWell did not review it in full before publishing, so it is possible that parts of the audio were inaccurately transcribed. If you have questions about any part of this transcript, please review the original audio recording that was posted along with these notes. Elie: All right. Well, thanks everyone for coming. I'm Elie Hassenfeld. I'm one of Givewell's co- founders. This is Natalie Crispin. Natalie: Hi. I'm a senior research analyst at Givewell. Elie: We're really happy that you joined us tonight. I just want to quickly go through some of the logistics and the basic plan for the evening. Then I'll turn it over to Natalie to talk a little bit. Just first, like we do with pretty much everything that Givewell does, we're going to try to share as much of this evening as we can with our audience. That means that we're going to record the audio of the session and publish a transcript on our website. If you say anything that you would prefer not be included in the audio or transcript, just email me, [email protected] or [email protected] or just come find me at the end of the night, and we can make sure to cut that from the event. You should feel free to speak totally freely this evening. -

OFTW's 2020 Annual Report
August 2020 One for the World Annual Report [email protected] Executive Summary Introduction Current state of play | Performance | Lessons learnt | Outstanding questions Financial Metrics Donations in Year | Impact Snapshot | Recruitment | Donor Retention & Activation | Chapter Performance Our Growth FY20 & FY21 Financials | School Expansion | Our Partners Looking Ahead The Next Year | Lessons Learnt | Outstanding Questions | SWOT Analysis Our Charities Charity selection process | Our charities FY21 Strategy | July 2020 Dear Friends and Supporters Welcome to OFTW’s 2019/2020 annual report! I’m going to be honest - it’s a little hard to know what to say about this year. On the one hand, the world was turned upside down by coronavirus and our operating model was suddenly no longer viable. Then the Black Lives Matter protests brought home the searing consequences of social injustice in the US and elsewhere, and our passionate volunteers were understandably moved to get involved. One for the World HQ hasn’t met face-to-face since March and I was personally unable to move to the US as planned and now find myself in Berlin, waiting to see when American visas become available again. However, in amongst these extraordinary, unprecedented times, One for the World continues to offer thousands of genuinely heart-warming reminders that, together, we can revolutionize charitable giving to end extreme poverty. Our wonderful, passionate, relentless chapter leaders brought 750 new pledgers onboard in the Fall semester alone. Our inspiring members contributed $312k to the world’s most cost-effective charities (a 40% year-on-year increase). 42 new chapters started the setting up process during a global pandemic. -

Strengthening Malaria Surveillance for Data- Driven Decision Making in Mozambique
MALARIA CONSORTIUM PROJECT BRIEF Strengthening malaria surveillance for data- driven decision making in Mozambique Accelerating efforts to reduce the malaria burden by improving data quality and use across all transmission strata Background Country Mozambique Although Mozambique has made some progress in scaling up malaria control activities and aligning its malaria elimination efforts with neighbouring countries Donor Bill & Melinda Gates Foundation in southern Africa over the last decade, it remains the fourth largest contributor of malaria cases globally.[1] Length of project May 2019 – May 2022 To accelerate efforts to reduce the malaria burden, Mozambique urgently needs a fit-for-purpose surveillance system to provide the necessary intelligence to identify Partners bottlenecks in malaria control and elimination activities, target interventions more Clinton Health Access Initiative efficiently and respond when the impact of National Malaria Control Programme Goodbye Malaria/LSDI2 activities is jeopardised. Manhica Health Research Centre Ministry of Health A malaria surveillance system is considered functional and responsive when it World Health Organization can produce evidence-based information from quality data that is routinely used Collaborator for planning and decision making. The 2018 national malaria surveillance system U.S. President’s Malaria Initiative assessment identified the following main obstacles: • poor malaria data quality (DQ) and data use (DU) • lack of an integrated malaria information storage system (iMISS) • -

UGANDA Who We Are
UGANDA WHO WE ARE The principal aim of The organisation works to monitoring and evaluation Malaria Consortium is the improve not only the health and operational research. of the individual, but also the Since then, the Malaria Consortium prevention and treatment of capacity of national health disease, particularly but not Uganda programme has expanded systems and communities, its focus to include tuberculosis, exclusively malaria, among which contributes towards pneumonia, diarrhoea and the poorest and most at risk. poverty relief and improved neglected tropical diseases. Malaria Consortium works economic prosperity. Cross cutting aspects such as in a variety of settings Malaria Consortium started health system strengthening, accross Africa and Asia, its Uganda programme in 2003 private sector support, maternal to provide technical assistance and child health are also becoming using innovative strategies to the Ministry of Health (MoH) important priorities. Contributing and approaches. and partners in malaria strategy quality work to the evidence base and policy development, for disease control interventions implementation support, remains a critical focus. Uganda has the third highest malaria burden in Africa, with the disease being the cause of 50 percent of out-patient cases and 14 percent of in-patient deaths. Malaria Consortium is registered in the UK as Charity No. 1099776. WHat WE DO The Uganda programme DISEASE PREVENTION CASE managEMENT has reached almost all of Preventive activities aim to & DIagnOSTICS the more than one hundred rapidly reduce the incidence Technical assistance to the MoH districts in Uganda. of malaria and other diseases. focuses on policies and guidelines, Activities include the distribution training, supply chain management of millions of long lasting to distribute drugs and supplies, insecticidal nets through mass and diagnostic support including campaigns and routinely through the introduction of external quality health facilities, the promotion of assurance systems. -

Beyond Feel-Good Philanthropy by Dr Michael Liffman, Director of the Asia-Pacific Centre for Social Investment and Philanthropy at Swinburne University
Beyond feel-good Philanthropy By Dr Michael Liffman, Director of the Asia-Pacific Centre for Social Investment and Philanthropy at Swinburne University. am sure we have all experienced social investment is effective, and can be shown to be so. This is, that strange feeling when driving, in my view, a very good place for the debate to have moved to. of arriving at the other side of a difficult intersection with no recollection Encouragingly, a similar focus is emerging in Australia too. of how we crossed it. The current debate The Centre for Social Impact is offering useful resources for overseas about the importance of impact the measurement of social return through the December in giving reminds me a little of that feeling. issue of its publication Knowledge Connect, and its Suddenly, instead of talking about the forthcoming short course: http://csi.edu.au/latest-csi-news/ virtue of giving, the commentators csi-march-newsletter/#Social are talking about ‘social return’. “ I contend that a mature philanthropic Typical is the December 2009 issue of that especially useful UK-based journal, Alliance which draws attention sector is one which recognises that to commentators who urge that outcomes are more generosity does not exonerate virtuous important than donor intentions. people from the responsibility to A discussion at the European Foundation Centre Conference consider the effectiveness of their in Rome last year led to leading British consultant (and one of APCSIP’s early Waislitz Visiting Fellows) David Carrington actions, by ensuring that their gift, being commissioned to produce a report asking whether better if not maximising the good it can do, research into philanthropy and social investment could improve is at least is doing some real good.” the practice of philanthropy. -

Integrating Neglected Tropical Diseases Into Primary Healthcare
ADVOCACY BRIEF Untapped potential: Integrating neglected tropical diseases into primary healthcare • Mass drug administration for neglected tropical diseases (NTDs) should be accompanied by cross-sectoral complementary interventions. • Integrating NTDs with primary healthcare structures offers a sustainable approach. • This integration must be government-owned and engage a wide range of stakeholders. Background NTDs are a diverse group of 20 diseases that affect adopted by 193 countries, call for an 'end to the epidemic' more than a billion people in low and middle-income of NTDs by 2030.[8] countries[1] and disproportionately impact the most vulnerable: women, children, refugees and those living To date, global efforts to reduce the prevalence of NTDs in poverty. Collectively, they are thought to account for have largely focused on providing chemoprevention to 26.06 million disability-adjusted life years.[2] Their social at-risk populations in endemic areas through mass drug administration (MDA). While this has achieved impressive and economic impacts are also significant. Many NTDs [9] cause suffering, disability and disfigurement, which can results in breaking some disease transmission cycles and lead to social stigma,[3] exclusion and discrimination,[4] will remain key to prevention and control programmes, marginalisation of women and girls[5] and lack of there is a need for other complementary interventions as opportunities such as employment.[6] MDA: [10] In recent years, NTDs have received more attention from • is only available and recommended for five NTDs the global development community. The 2012 London • will cease to be as cost-effective as testing and treating Declaration saw decision makers endorse the World affected individuals as the prevalence of NTDs Health Organization’s (WHO) ambitious NTD roadmap[7] decreases that sought to enhance the control, prevention, and elimination of NTDs and to eradicate at least two by 2020. -

Mission Variety and Industry Equilibrium in Decentralized Public Good Provision
The Dark Side of Transparency: Mission Variety and Industry Equilibrium in Decentralized Public Good Provision Gani Aldashev Esteban Jaimovichy Thierry Verdierz January 2021 Abstract We study the implications of transparency policies on decentralized public good provision. The moral hazard inside non-profits interacts with the competitive struc- ture of the sector under alternative informational regimes. More transparency on the use of funds has an ambiguous effect on the total public good provision and donor’s welfare. Transparency encourages non-profits to more actively curb rent-seeking in- side organizations, but it also tilts the playing field against non-profit managers facing higher monitoring costs, inducing them to abandon their missions and reducing non- profit diversity. Donors’welfare is lower under transparency for intermediate levels of asymmetry in monitoring costs. Keywords: non-profit organizations, charitable giving, altruism, transparency. JEL codes: L31, D64, D43, D23. ECARES, SBS-EM, Université libre de Bruxelles (ULB), and Ronald Coase Visiting Professor at TILEC, Tilburg University. Mailing address: 50 Avenue Roosevelt, CP 114, 1050 Brussels, Belgium. Email: [email protected]. yUniversity of Surrey. Mailing address: School of Economics, Guildford, Surrey, GU2 7XH, UK. Email: [email protected]. zCorresponding author. Ecole des Ponts - Paris Tech, PUC-Rio, and CEPR. Mailing address: PSE, 48 Boulevard Jourdan, 75014 Paris, France. Email: [email protected]. 1 1 Introduction The traditional view in economics considers private profit-oriented firms as the main channel of provision of private goods, and governments as the main providers of public goods. This view is an imperfect representation of real-life economies.