Hearing on Pending Legislation Hearing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(202) 224-2235 Fax: (202) 228-2862
Name House/Senate Political Party Homestate/-district Email/ Contactform Adress (DC) John McCain (Chairman) Senate RepuBlican Arizona https://www.mccain.senate.Gov/puBlic/index.cfm/contact-form 218 Russell Senate Office BuildinG WashinGton, DC 20510 Main: (202) 224-2235 Fax: (202) 228-2862 Jack Reed (RankinG MemBer) Senate Democrat Rhode Island http://www.reed.senate.Gov/contact 728 Hart Senate Office BuildinG WashinGton, DC 20510 T: (202) 224-4642 F: (202) 224-4680 James Inhofe Senate RepuBlican Oklahoma https://www.inhofe.senate.Gov/contact 205 Russell Senate Office BuildinG WashinGton, DC 20510-3603 Main: (202) 224-4721 Fax: (202) 228-0380 Jeff Sessions Senate R Alabama https://www.sessions.senate.Gov/puBlic/index.cfm/contact-jeff 326 Russell Senate Office BuildinG WashinGton, DC 20510 Main: (202) 224-4124 Fax: (202) 224-3149 RoGer Wicker Senate R Mississippi https://www.wicker.senate.Gov/puBlic/index.cfm/contact 555 Dirksen Senate Office BuildinG WashinGton, DC 20510 Main: (202) 224-6253 Fax: (202) 228-0378 Kelly Ayotte Senate R New Hampshire https://www.ayotte.senate.Gov/?p=contact 144 Russell Senate Office BuildinG WashinGton, D.C. 20510 Phone: 202-224-3324 Fax: 202-224-4952 Deb Fischer Senate R NeBraska http://www.fischer.senate.Gov/puBlic/index.cfm/contact 454 Russell Senate Office BuildinG WashinGton, DC 20510 Phone: (202) 224-6551 Fax: (202) 228-1325 Tom Cotton Senate R Arkansas https://www.cotton.senate.Gov/?p=contact 124 Russell Senate Office BuildinG WashinGton, DC 20510 Phone: (202) 224-2353 Mike Rounds Senate R South Dakota -

The Honorable Mitch Mcconnell the Honorable Chuck Schumer Majority
The Honorable Mitch McConnell The Honorable Chuck Schumer Majority Leader Minority Leader United States Senate United States Senate Washington, DC 20510 Washington, DC 20501 The Honorable Richard Shelby The Honorable Patrick Leahy Chairman Vice Chairman U.S. Senate Committee on Appropriations U.S. Senate Committee on Appropriations Washington, DC 20510 Washington, DC 20510 August 5, 2020 Dear Leader McConnell, Leader Schumer, Chairman Shelby, and Vice Chairman Leahy: We are writing to urge you to include an additional $20 million for the National Criminal History Improvement Program in the next coronavirus relief package. Reauthorized in the bipartisan Fix NICS Act, this critical funding will help ensure that states and localities, already struggling financially because of the pandemic, are able to maintain accurate records in the face of an unprecedented surge in firearm sales. At a time when domestic violence is on the rise,1 we must ensure that firearms stay out of the hands of abusers and others seeking firearms illegally. As the COVID-19 pandemic rages across the United States, the National Instant Criminal Background Check System (NICS) has seen an unprecedented surge in background checks. In March 2020, when many states began to take necessary action to mitigate the spread of the coronavirus, there were more than 3.7 million background check transactions.2. This alarming trend has continued in subsequent months. June 2020 was the busiest month in the program’s history with more than 3.9 million background check transactions.3 NICS reported its busiest week from March 16 to March 22, 2020; seven of its 10 busiest weeks have occurred between February and June 2020.4 Now more than ever, Congress must do everything in its power to support the background check system to ensure guns do not fall into the wrong hands. -

Mcconnell Announces Senate Republican Committee Assignments for the 117Th Congress
For Immediate Release, Wednesday, February 3, 2021 Contacts: David Popp, Doug Andres Robert Steurer, Stephanie Penn McConnell Announces Senate Republican Committee Assignments for the 117th Congress Praises Senators Crapo and Tim Scott for their work on the Committee on Committees WASHINGTON, D.C. – Following the 50-50 power-sharing agreement finalized earlier today, Senate Republican Leader Mitch McConnell (R-KY) announced the Senate Republican Conference Committee Assignments for the 117th Congress. Leader McConnell once again selected Senator Mike Crapo (R-ID) to chair the Senate Republicans’ Committee on Committees, the panel responsible for committee assignments for the 117th Congress. This is the ninth consecutive Congress in which Senate leadership has asked Crapo to lead this important task among Senate Republicans. Senator Tim Scott (R-SC) assisted in the committee selection process as he did in the previous three Congresses. “I want to thank Mike and Tim for their work. They have both earned the trust of our colleagues in the Republican Conference by effectively leading these important negotiations in years past and this year was no different. Their trust and experience was especially important as we enter a power-sharing agreement with Democrats and prepare for equal representation on committees,” McConnell said. “I am very grateful for their work.” “I appreciate Leader McConnell’s continued trust in having me lead the important work of the Committee on Committees,” said Senator Crapo. “Americans elected an evenly-split Senate, and working together to achieve policy solutions will be critical in continuing to advance meaningful legislation impacting all Americans. Before the COVID-19 pandemic hit our nation, our economy was the strongest it has ever been. -
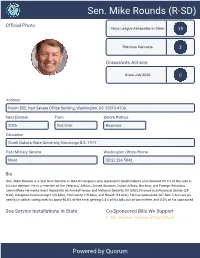
Sen. Mike Rounds (R-SD)
Sen. Mike Rounds (R-SD) Official Photo Navy League Advocates in State 19 Previous Contacts 3 Grassroots Actions Since July 2020 0 Address Room 502, Hart Senate Office Building, Washington, DC 20510-4106 Next Election Term Before Politics 2026 2nd term Business Education South Dakota State University, Brookings B.S. 1977 Past Military Service Washington Office Phone None (202) 224-5842 Bio Sen. Mike Rounds is a 2nd term Senator in the US Congress who represents South Dakota and received 65.7% of the vote in his last election. He is a member of the Veterans' Affairs, Armed Services, Indian Affairs, Banking, and Foreign Relations committees.He works most frequently on Armed Forces and National Security (51 bills), Finance and Financial Sector (29 bills), Congressional oversight (25 bills), Commerce (18 bills), and Health (16 bills). He has sponsored 107 bills in his last six year(s) in office, voting with his party 90.6% of the time, getting 2.8% of his bills out of committee, and 0.0% of his sponsored Sea Service Installations in State: Co-Sponsored Bills We Support S. 133: Merchant Mariners of World War II Powered by Quorum Sen. Mike Rounds (R-SD) Committees Senate Committee on Banking, Housing, and Urban... Senate Committee on Foreign Relations Senate Committee on Armed Services Senate Committee on Indian Affairs Senate Committee on Veterans' Affairs Subcommittees Senate Subcommittee on Africa and Global Health... Senate Subcommittee on Cybersecurity Senate Subcommittee on East Asia, the Pacific, and... Senate Subcommittee on Financial Institutions and... Senate Subcommittee on Housing, Transportation,... Senate Subcommittee on Multilateral International.. -

Ranking Member John Barrasso
Senate Committee Musical Chairs August 15, 2018 Key Retiring Committee Seniority over Sitting Chair/Ranking Member Viewed as Seat Republicans Will Most Likely Retain Viewed as Potentially At Risk Republican Seat Viewed as Republican Seat at Risk Viewed as Seat Democrats Will Most Likely Retain Viewed as Potentially At Risk Democratic Seat Viewed as Democratic Seat at Risk Notes • The Senate Republican leader is not term-limited; Senator Mitch McConnell (R-KY) will likely remain majority leader. The only member of Senate GOP leadership who is currently term-limited is Republican Whip John Cornyn (R-TX). • Republicans have term limits of six years as chairman and six years as ranking member. Republican members can only use seniority to bump sitting chairs/ranking members when the control of the Senate switches parties. • Committee leadership for the Senate Aging; Agriculture; Appropriations; Banking; Environment and Public Works (EPW); Health Education, Labor, and Pensions (HELP); Indian Affairs; Intelligence; Rules; and Veterans Affairs Committees are unlikely to change. Notes • Current Armed Services Committee (SASC) Chairman John McCain (R-AZ) continues to receive treatment for brain cancer in Arizona. Senator James Inhofe (R-OK) has served as acting chairman and is likely to continue to do so in Senator McCain’s absence. If Republicans lose control of the Senate, Senator McCain would lose his top spot on the committee because he already has six years as ranking member. • In the unlikely scenario that Senator Chuck Grassley (R-IA) does not take over the Finance Committee, Senator Mike Crapo (R-ID), who currently serves as Chairman of the Banking Committee, could take over the Finance Committee. -

July 15 2021 the Honorable Chuck Schumer Senate Majority Leader
July 15 2021 The Honorable Chuck Schumer Senate Majority Leader United States Senate Washington, D.C. 20510 The Honorable Mitch McConnell Senate Minority Leader United States Senate Washington, D.C. 20510 The Honorable Nancy Pelosi Speaker of the House U.S. House of Representatives Washington, D.C. 20515 The Honorable Kevin McCarthy House Minority Leader U.S. House of Representatives Washington, D.C. 20515 Dear Majority Leader Schumer, Minority Leader McConnell, Speaker Pelosi, and Minority Leader McCarthy: As Congress continues to negotiate legislative packages to invest in infrastructure and improve our nation’s health system, we urge you to provide at least $30 billion in funding to prevent and prepare for future pandemics. The COVID-19 pandemic has made clear that underinvesting in our public health infrastructure, our biomedical research pipeline, and our medical supply chain has disastrous consequences. A robust investment in pandemic prevention and our underlying public health system is critical as the country continues to recover from COVID-19. The COVID-19 pandemic has wreaked havoc on communities across the country and devastated the economy. Since the pandemic began, over 33 million Americans have been infected with the virus and over 605,000 have died.1 Thanks to the rapid development and deployment of COVID- 19 vaccines, the United States has seen a dramatic drop in COVID-19 cases, hospitalizations, and deaths over the course of 2021.2 But the pandemic is not yet over. Though roughly 67 percent of American adults have received at least one dose of the COVID-19 vaccine, millions of 1 New York Times, “Coronavirus in the U.S.: Latest Map and Case Count,” accessed July 9, 2021, https://www.nytimes.com/interactive/2021/us/covid-cases.html. -

LDF Applauds Testimony of Debo Adegbile to Senate Judiciary Committee
LDF Applauds Testimony of Debo Adegbile to Senate Judiciary Committee Today, Debo Adegbile, nominated to become the next Assistant Attorney General for the Department of Justice's Civil Rights division, presented testimony to the Senate Judiciary Committee. The following is a statement from Sherrilyn Ifill, President and Director- Counsel of the NAACP Legal Defense and Educational Fund, Inc. "With poise, humor and straightforward answers, Debo Adegbile, deftly managed his presentation to the Senate Judiciary Committee during his confirmation hearing to become the next Assistant Attorney General for the Department of Justice's Civil Rights division. Leaders from major civil rights organizations and unions attended the hearing in a powerful show of support for Adegbile's nomination. Senator Patrick Leahy (D-VT) described Debo Adegbile's journey from instances of homelessness as a child to today's confirmation hearing as "a remarkable example of the American dream." Senator Richard Blumenthal (D-CT) praised "LDF and other civil rights organizations" that "serve a critical role in our justice system." During the hearing, Adegbile spoke about his work at LDF defending the civil rights of every American. "We can and must do more to protect civil rights. I've seen the impact that enforcing civil rights can have on real peoples' lives," Adegbile said during his testimony. "If confirmed as Assistant Attorney General, the people I will be serving are the people of the United States of America," Adegbile added. As Senators mangled the pronunciation of his name, Adegbile joked with good nature, assigning "partial credit" to those Senators who made the effort to pronounce his last name correctly. -

SENATE COMMITTEE ASSIGNMENTS Leadership Is Highlighted in Yellow, While New Members to the Committee Are in Bold
SENATE COMMITTEE ASSIGNMENTS Leadership is highlighted in yellow, while new members to the committee are in bold. Agriculture, Nutrition and Forestry Majority Minority Pat Roberts, CHAIRMAN, Kansas Patrick Leahy, Vermont Thad Cochran, Mississippi Debbie Stabenow, RANKING, Michigan Mitch McConnell, Kentucky Sherrod Brown, Ohio John Boozman, Arkansas Amy Klobuchar, Minnesota John Hoeven, North Dakota Michael Bennet, Colorado Chuck Grassley, Iowa Kirsten Gillibrand, New York John Thune, South Dakota Joe Donnelly, Indiana David Perdue, Georgia Heidi Heitkamp, North Dakota Joni Ernst, Iowa Bob Casey, Pennsylvania Thom Tillis, North Carolina Ben Sasse, Nebraska Appropriations Majority Minority Thad Cochran, CHAIRMAN, Mississippi Patrick Leahy, Vermont Mitch McConnell, Kentucky Barbara Mikulski, RANKING, Maryland Richard Shelby, Alabama Patty Murray, Washington Lamar Alexander, Tennessee Dianne Feinstein, California (cont'd) (cont'd) 1 Susan Collins, Maine Dick Durbin, Illinois Lisa Murkowski, Alaska Jack Reed, Rhode Island Lindsey Graham, South Carolina Jon Tester, Montana Mark Kirk, Illinois Tom Udall, New Mexico Roy Blunt, Missouri Jeanne Shaheen, New Hampshire Jerry Moran, Kansas Jeff Merkley, Oregon John Hoeven, North Dakota Chris Coons, Delaware John Boozman, Arkansas Brian Schatz, Hawaii Shelley Moore Capito, West Virginia Tammy Baldwin, Wisconsin Bill Cassidy, Louisiana Chris Murphy, Connecticut James Lankford, Oklahoma Steve Daines, Montana Armed Services Majority Minority John McCain, CHAIRMAN, Arizona Jack Reed, RANKING, Rhode Island -

Appendix to the Petition for a Writ of Certiorari ______
No. 19-___ IN THE Supreme Court of the United States _____________ SENATORS RICHARD BLUMENTHAL, RICHARD J. DURBIN, PATTY MURRAY, ELIZABETH WARREN, AMY KLOBUCHAR, BERNARD SANDERS, PATRICK LEAHY, SHELDON WHITEHOUSE, CHRISTOPHER A. COONS, MAZIE K. HIRONO, CORY A. BOOKER, KAMALA D. HARRIS, MICHAEL F. BENNET, MARIA CANTWELL, BENJAMIN L. CARDIN, TOM CARPER, CATHERINE CORTEZ MASTO, TAMMY DUCKWORTH, KIRSTEN E. GILLIBRAND, MARTIN HEINRICH, TIM KAINE, EDWARD J. MARKEY, JEFF MERKLEY, CHRIS MURPHY, JACK REED, BRIAN SCHATZ, TOM UDALL, CHRIS VAN HOLLEN, AND RON WYDEN, Petitioners, v. DONALD J. TRUMP, IN HIS OFFICIAL CAPACITY AS PRESIDENT OF THE UNITED STATES, Respondent. _____________ On Petition for a Writ of Certiorari to the U.S. Court of Appeals for the District of Columbia Circuit _____________ APPENDIX TO THE PETITION FOR A WRIT OF CERTIORARI _____________ ELIZABETH B. WYDRA BRIANNE J. GOROD* BRIAN R. FRAZELLE CONSTITUTIONAL ACCOUNTABILITY CENTER 1200 18th Street NW, Suite 501 Washington, D.C. 20036 (202) 296-6889 [email protected] Counsel for Petitioners July 6, 2020 * Counsel of Record APPENDIX TABLE OF CONTENTS Page Judgment of the U.S. Court of Appeals for the District of Columbia Circuit (February 7, 2020) .................................. App. 1 Opinion of the U.S. Court of Appeals for the District of Columbia Circuit (February 7, 2020) .................................. App. 3 Order of the U.S. District Court for the District of Columbia (September 28, 2018) ....................................................... App. 14 Memorandum Opinion of the U.S. District Court for the District of Columbia (September 28, 2018) ............ App. 15 Order of the U.S. District Court for the District of Columbia (April 30, 2019) ... -
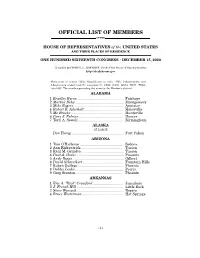
Official List of Members
OFFICIAL LIST OF MEMBERS OF THE HOUSE OF REPRESENTATIVES of the UNITED STATES AND THEIR PLACES OF RESIDENCE ONE HUNDRED SIXTEENTH CONGRESS • DECEMBER 15, 2020 Compiled by CHERYL L. JOHNSON, Clerk of the House of Representatives http://clerk.house.gov Democrats in roman (233); Republicans in italic (195); Independents and Libertarians underlined (2); vacancies (5) CA08, CA50, GA14, NC11, TX04; total 435. The number preceding the name is the Member's district. ALABAMA 1 Bradley Byrne .............................................. Fairhope 2 Martha Roby ................................................ Montgomery 3 Mike Rogers ................................................. Anniston 4 Robert B. Aderholt ....................................... Haleyville 5 Mo Brooks .................................................... Huntsville 6 Gary J. Palmer ............................................ Hoover 7 Terri A. Sewell ............................................. Birmingham ALASKA AT LARGE Don Young .................................................... Fort Yukon ARIZONA 1 Tom O'Halleran ........................................... Sedona 2 Ann Kirkpatrick .......................................... Tucson 3 Raúl M. Grijalva .......................................... Tucson 4 Paul A. Gosar ............................................... Prescott 5 Andy Biggs ................................................... Gilbert 6 David Schweikert ........................................ Fountain Hills 7 Ruben Gallego ............................................ -

The Status of the Housing Finance System After Nine Years of Conservator- Ship
S. HRG. 115–56 THE STATUS OF THE HOUSING FINANCE SYSTEM AFTER NINE YEARS OF CONSERVATOR- SHIP HEARING BEFORE THE COMMITTEE ON BANKING, HOUSING, AND URBAN AFFAIRS UNITED STATES SENATE ONE HUNDRED FIFTEENTH CONGRESS FIRST SESSION ON EXAMINING THE CURRENT FINANCIAL AND OPERATIONAL PERFORM- ANCE OF FANNIE MAE AND FREDDIE MAC, AND EXPLORING OPPOR- TUNITIES FOR LEGISLATIVE REFORM MAY 11, 2017 Printed for the use of the Committee on Banking, Housing, and Urban Affairs ( Available at: http://www.fdsys.gov/ U.S. GOVERNMENT PUBLISHING OFFICE 26–521 PDF WASHINGTON : 2018 For sale by the Superintendent of Documents, U.S. Government Publishing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 VerDate Nov 24 2008 15:20 Dec 22, 2017 Jkt 046629 PO 00000 Frm 00001 Fmt 5011 Sfmt 5011 S:\DOCS\26521.TXT SHERYL COMMITTEE ON BANKING, HOUSING, AND URBAN AFFAIRS MIKE CRAPO, Idaho, Chairman RICHARD C. SHELBY, Alabama SHERROD BROWN, Ohio BOB CORKER, Tennessee JACK REED, Rhode Island PATRICK J. TOOMEY, Pennsylvania ROBERT MENENDEZ, New Jersey DEAN HELLER, Nevada JON TESTER, Montana TIM SCOTT, South Carolina MARK R. WARNER, Virginia BEN SASSE, Nebraska ELIZABETH WARREN, Massachusetts TOM COTTON, Arkansas HEIDI HEITKAMP, North Dakota MIKE ROUNDS, South Dakota JOE DONNELLY, Indiana DAVID PERDUE, Georgia BRIAN SCHATZ, Hawaii THOM TILLIS, North Carolina CHRIS VAN HOLLEN, Maryland JOHN KENNEDY, Louisiana CATHERINE CORTEZ MASTO, Nevada GREGG RICHARD, Staff Director -

December 4, 2020 the Honorable Mitch Mcconnell the Honorable
December 4, 2020 The Honorable Mitch McConnell The Honorable Charles Schumer Majority Leader Minority Leader United States Senate United States Senate Washington, DC 20510 Washington, DC 20510 Dear Leaders McConnell and Schumer: We write to express our support for addressing upcoming physician payment cuts in ongoing legislative negotiations. We believe these cuts will further strain our health care system, which is already stressed by the COVID-19 pandemic, and jeopardize patient access to medically necessary services over the long-term. On December 1, 2020, the Centers for Medicare & Medicaid Services finalized the Medicare Physician Fee Schedule for 2021. The fee schedule includes several positive attributes, including improvements for maternity care and much-needed payment increases for physicians delivering primary and other essential outpatient and office-based care to some of our nation’s most vulnerable patients. These changes should take effect on January 1, 2021, as planned. However, a statutory budget neutrality rule requires that any increases in Medicare payments for these office visits, also known as evaluation and management (E/M) services, must be offset by corresponding decreases. As a result, many practitioners including surgeons, specialists, therapists and others face substantial cuts beginning on January 1, 2021, if Congress does not take action to provide relief. Health care professionals across the spectrum are reeling from the effects of the COVID-19 emergency as they continue to serve patients during this global pandemic. The payment cuts finalized by CMS would pose a threat to providers and their patients under any circumstances, but during a pandemic the impact is even more profound.