Association of XRCC3 and XRCC4 Gene Polymorphisms, Family History
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model
Downloaded from http://www.jimmunol.org/ by guest on September 25, 2021 T + is online at: average * The Journal of Immunology , 34 of which you can access for free at: 2016; 197:1477-1488; Prepublished online 1 July from submission to initial decision 4 weeks from acceptance to publication 2016; doi: 10.4049/jimmunol.1600589 http://www.jimmunol.org/content/197/4/1477 Molecular Profile of Tumor-Specific CD8 Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. Waugh, Sonia M. Leach, Brandon L. Moore, Tullia C. Bruno, Jonathan D. Buhrman and Jill E. Slansky J Immunol cites 95 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2016/07/01/jimmunol.160058 9.DCSupplemental This article http://www.jimmunol.org/content/197/4/1477.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 25, 2021. The Journal of Immunology Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. -

1 AGING Supplementary Table 2
SUPPLEMENTARY TABLES Supplementary Table 1. Details of the eight domain chains of KIAA0101. Serial IDENTITY MAX IN COMP- INTERFACE ID POSITION RESOLUTION EXPERIMENT TYPE number START STOP SCORE IDENTITY LEX WITH CAVITY A 4D2G_D 52 - 69 52 69 100 100 2.65 Å PCNA X-RAY DIFFRACTION √ B 4D2G_E 52 - 69 52 69 100 100 2.65 Å PCNA X-RAY DIFFRACTION √ C 6EHT_D 52 - 71 52 71 100 100 3.2Å PCNA X-RAY DIFFRACTION √ D 6EHT_E 52 - 71 52 71 100 100 3.2Å PCNA X-RAY DIFFRACTION √ E 6GWS_D 41-72 41 72 100 100 3.2Å PCNA X-RAY DIFFRACTION √ F 6GWS_E 41-72 41 72 100 100 2.9Å PCNA X-RAY DIFFRACTION √ G 6GWS_F 41-72 41 72 100 100 2.9Å PCNA X-RAY DIFFRACTION √ H 6IIW_B 2-11 2 11 100 100 1.699Å UHRF1 X-RAY DIFFRACTION √ www.aging-us.com 1 AGING Supplementary Table 2. Significantly enriched gene ontology (GO) annotations (cellular components) of KIAA0101 in lung adenocarcinoma (LinkedOmics). Leading Description FDR Leading Edge Gene EdgeNum RAD51, SPC25, CCNB1, BIRC5, NCAPG, ZWINT, MAD2L1, SKA3, NUF2, BUB1B, CENPA, SKA1, AURKB, NEK2, CENPW, HJURP, NDC80, CDCA5, NCAPH, BUB1, ZWILCH, CENPK, KIF2C, AURKA, CENPN, TOP2A, CENPM, PLK1, ERCC6L, CDT1, CHEK1, SPAG5, CENPH, condensed 66 0 SPC24, NUP37, BLM, CENPE, BUB3, CDK2, FANCD2, CENPO, CENPF, BRCA1, DSN1, chromosome MKI67, NCAPG2, H2AFX, HMGB2, SUV39H1, CBX3, TUBG1, KNTC1, PPP1CC, SMC2, BANF1, NCAPD2, SKA2, NUP107, BRCA2, NUP85, ITGB3BP, SYCE2, TOPBP1, DMC1, SMC4, INCENP. RAD51, OIP5, CDK1, SPC25, CCNB1, BIRC5, NCAPG, ZWINT, MAD2L1, SKA3, NUF2, BUB1B, CENPA, SKA1, AURKB, NEK2, ESCO2, CENPW, HJURP, TTK, NDC80, CDCA5, BUB1, ZWILCH, CENPK, KIF2C, AURKA, DSCC1, CENPN, CDCA8, CENPM, PLK1, MCM6, ERCC6L, CDT1, HELLS, CHEK1, SPAG5, CENPH, PCNA, SPC24, CENPI, NUP37, FEN1, chromosomal 94 0 CENPL, BLM, KIF18A, CENPE, MCM4, BUB3, SUV39H2, MCM2, CDK2, PIF1, DNA2, region CENPO, CENPF, CHEK2, DSN1, H2AFX, MCM7, SUV39H1, MTBP, CBX3, RECQL4, KNTC1, PPP1CC, CENPP, CENPQ, PTGES3, NCAPD2, DYNLL1, SKA2, HAT1, NUP107, MCM5, MCM3, MSH2, BRCA2, NUP85, SSB, ITGB3BP, DMC1, INCENP, THOC3, XPO1, APEX1, XRCC5, KIF22, DCLRE1A, SEH1L, XRCC3, NSMCE2, RAD21. -

The Genetic Bases of Uterine Fibroids; a Review
Review Article The Genetic Bases of Uterine Fibroids; A Review Veronica Medikare 1, Lakshmi Rao Kandukuri 2, Venkateshwari Ananthapur 3, Mamata Deenadayal 4, Pratibha Nallari 1* 1- Department of Genetics, Osmania University, Hyderabad, India 2- Center for Cellular and Molecular Biology, Habsiguda, Hyderabad, India 3- Institute of Genetics and Hospital for Genetic Diseases, Begumpet, Hyderabad, India 4- Infertility Institute and research Center, Secunderabad, India Abstract Uterine leiomyomas/fibroids are the most common pelvic tumors of the female genital tract. The initiators remaining unknown, estrogens and progesterone are considered as promoters of fibroid growth. Fibroids are monoclonal tumors showing 40-50% karyo- typically detectable chromosomal abnormalities. Cytogenetic aberrations involving chromosomes 6, 7, 12 and 14 constitute the major chromosome abnormalities seen in leiomyomata. This has led to the discovery that disruptions or dysregulations of HMGIC and HMGIY genes contribute to the development of these tumors. Genes such as RAD51L1 act as translocation partners to HMGIC and lead to disruption of gene structure leading to the pathogenesis of uterine fibroids. The mechanism underlying * Corresponding Author: this disease is yet to be identified. The occurrence of PCOLCE amid a cluster of at Downloaded from http://www.jri.ir Pratibha Nallari, Department of Genetics, least eight Alu sequences is potentially relevant to the possible involvement of Osmania University, PCOLCE in the 7q22 rearrangements that occur in many leiomyomata. PCOLCE is Hyderabad, 500 007, implicated in cell growth processes. Involvement of Alu sequences in rearrangements India can lead to the disruption of this gene and, hence, loss of control for gene expression E-mail: leading to uncontrolled cell growth. -

Insights Into Regulation of Human RAD51 Nucleoprotein Filament Activity During
Insights into Regulation of Human RAD51 Nucleoprotein Filament Activity During Homologous Recombination Dissertation Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Ravindra Bandara Amunugama, B.S. Biophysics Graduate Program The Ohio State University 2011 Dissertation Committee: Richard Fishel PhD, Advisor Jeffrey Parvin MD PhD Charles Bell PhD Michael Poirier PhD Copyright by Ravindra Bandara Amunugama 2011 ABSTRACT Homologous recombination (HR) is a mechanistically conserved pathway that occurs during meiosis and following the formation of DNA double strand breaks (DSBs) induced by exogenous stresses such as ionization radiation. HR is also involved in restoring replication when replication forks have stalled or collapsed. Defective recombination machinery leads to chromosomal instability and predisposition to tumorigenesis. However, unregulated HR repair system also leads to similar outcomes. Fortunately, eukaryotes have evolved elegant HR repair machinery with multiple mediators and regulatory inputs that largely ensures an appropriate outcome. A fundamental step in HR is the homology search and strand exchange catalyzed by the RAD51 recombinase. This process requires the formation of a nucleoprotein filament (NPF) on single-strand DNA (ssDNA). In Chapter 2 of this dissertation I describe work on identification of two residues of human RAD51 (HsRAD51) subunit interface, F129 in the Walker A box and H294 of the L2 ssDNA binding region that are essential residues for salt-induced recombinase activity. Mutation of F129 or H294 leads to loss or reduced DNA induced ATPase activity and formation of a non-functional NPF that eliminates recombinase activity. DNA binding studies indicate that these residues may be essential for sensing the ATP nucleotide for a functional NPF formation. -

Homologous Recombination As a Potential Target for Ca€Eine
Oncogene (2000) 19, 5788 ± 5800 ã 2000 Macmillan Publishers Ltd All rights reserved 0950 ± 9232/00 $15.00 www.nature.com/onc Homologous recombination as a potential target for caeine radiosensitization in mammalian cells: reduced caeine radiosensitization in XRCC2 and XRCC3 mutants Nesrin A Asaad1, Zhao-Chong Zeng1, Jun Guan1, John Thacker2 and George Iliakis*,1 1Department of Radiation Oncology of Kimmel Cancer Center, Jeerson Medical College, Philadelphia, Pennsylvania, PA 19107, USA; 2Medical Research Council, Radiation and Genome Stability Unit, Harwell, Oxfordshire, OX11 ORD, UK The radiosensitizing eect of caeine has been associated Introduction with the disruption of multiple DNA damage-responsive cell cycle checkpoints, but several lines of evidence also Caeine (1,3,7-trimethylxanthine) at submillimolar implicate inhibition of DNA repair. The role of DNA concentrations exerts a wide variety of physiological repair inhibition in caeine radiosensitization remains eects on dierent organisms from bacteria to man uncharacterized, and it is unknown which repair process, (Garattini, 1993; Timson, 1977). At higher concentra- or lesion, is aected. We show that a radiosensitive cell tions (0.5 ± 10 mM), it strongly enhances the cytotoxic line, mutant for the RAD51 homolog XRCC2 and eect of ionizing radiation and other physical or defective in homologous recombination repair (HRR), chemical agents that act by inducing damage in DNA displays signi®cantly diminished caeine radiosensitiza- (Kihlman, 1977; Murnane, 1995; Timson, 1977; tion that can be restored by expression of XRCC2. Waldren and Rasko, 1978). Radiosensitization is Despite the reduced radiosensitization, caeine eec- manifest at non-cytotoxic concentrations and therefore tively abrogates checkpoints in S and G2 phases in caeine is considered a model radiosensitizer. -

Rad51c Deficiency Destabilizes XRCC3, Impairs Recombination and Radiosensitizes S/G2-Phase Cells
Lawrence Berkeley National Laboratory Lawrence Berkeley National Laboratory Title Rad51C deficiency destabilizes XRCC3, impairs recombination and radiosensitizes S/G2- phase cells Permalink https://escholarship.org/uc/item/2fp0538b Authors Lio, Yi-Ching Schild, David Brenneman, Mark A. et al. Publication Date 2004-05-01 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Rad51C deficiency destabilizes XRCC3, impairs recombination and radiosensitizes S/G2-phase cells Yi-Ching Lio1, 2,*, David Schild1, Mark A. Brenneman3, J. Leslie Redpath2 and David J. Chen1 1Life Sciences Division, Lawrence Berkeley National Laboratory, Berkeley, CA 94720, USA; 2Department of Radiation Oncology, University of California, Irvine, Irvine, CA 92697, USA; 3Department of Genetics, Rutgers University, Piscataway, NJ 08854, USA. * To whom correspondence should be addressed: Yi-Ching Lio MS74-157, Life Sciences Division Lawrence Berkeley National Laboratory One Cyclotron Road Berkeley, CA 94720 Phone: (510) 486-5861 Fax: (510) 486-6816 e-mail: [email protected] Running title: Human Rad51C functions in homologous recombination Total character count: 52621 1 ABSTRACT The highly conserved Rad51 protein plays an essential role in repairing DNA damage through homologous recombination. In vertebrates, five Rad51 paralogs (Rad51B, Rad51C, Rad51D, XRCC2, XRCC3) are expressed in mitotically growing cells, and are thought to play mediating roles in homologous recombination, though their precise functions remain unclear. Here we report the use of RNA interference to deplete expression of Rad51C protein in human HT1080 and HeLa cells. In HT1080 cells, depletion of Rad51C by small interfering RNA caused a significant reduction of frequency in homologous recombination. The level of XRCC3 protein was also sharply reduced in Rad51C-depleted HeLa cells, suggesting that XRCC3 is dependent for its stability upon heterodimerization with Rad51C. -

RAD51L3 (1-216, His-Tag) Human Protein – AR51328PU-S | Origene
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for AR51328PU-S RAD51L3 (1-216, His-tag) Human Protein Product data: Product Type: Recombinant Proteins Description: RAD51L3 (1-216, His-tag) human recombinant protein, 0.1 mg Species: Human Expression Host: E. coli Tag: His-tag Predicted MW: 23.9 kDa Concentration: lot specific Purity: >95% by SDS - PAGE Buffer: Presentation State: Purified State: Liquid purified protein Buffer System: 20 mM Tris-HCl buffer (pH 8.0) containing 0.4M Urea, 10% glycerol Preparation: Liquid purified protein Protein Description: Recombinant human RDA51D protein, fused to His-tag at N-terminus, was expressed in E.coli. Storage: Store undiluted at 2-8°C for one week or (in aliquots) at -20°C to -80°C for longer. Avoid repeated freezing and thawing. Stability: Shelf life: one year from despatch. RefSeq: NP_001136043 Locus ID: 5892 UniProt ID: O75771 Cytogenetics: 17q12 Synonyms: BROVCA4; R51H3; RAD51L3; TRAD This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 RAD51L3 (1-216, His-tag) Human Protein – AR51328PU-S Summary: The protein encoded by this gene is a member of the RAD51 protein family. RAD51 family members are highly similar to bacterial RecA and Saccharomyces cerevisiae Rad51, which are known to be involved in the homologous recombination and repair of DNA. -

Whole-Exome Sequencing of Metastatic Cancer and Biomarkers of Treatment Response
Supplementary Online Content Beltran H, Eng K, Mosquera JM, et al. Whole-exome sequencing of metastatic cancer and biomarkers of treatment response. JAMA Oncol. Published online May 28, 2015. doi:10.1001/jamaoncol.2015.1313 eMethods eFigure 1. A schematic of the IPM Computational Pipeline eFigure 2. Tumor purity analysis eFigure 3. Tumor purity estimates from Pathology team versus computationally (CLONET) estimated tumor purities values for frozen tumor specimens (Spearman correlation 0.2765327, p- value = 0.03561) eFigure 4. Sequencing metrics Fresh/frozen vs. FFPE tissue eFigure 5. Somatic copy number alteration profiles by tumor type at cytogenetic map location resolution; for each cytogenetic map location the mean genes aberration frequency is reported eFigure 6. The 20 most frequently aberrant genes with respect to copy number gains/losses detected per tumor type eFigure 7. Top 50 genes with focal and large scale copy number gains (A) and losses (B) across the cohort eFigure 8. Summary of total number of copy number alterations across PM tumors eFigure 9. An example of tumor evolution looking at serial biopsies from PM222, a patient with metastatic bladder carcinoma eFigure 10. PM12 somatic mutations by coverage and allele frequency (A) and (B) mutation correlation between primary (y- axis) and brain metastasis (x-axis) eFigure 11. Point mutations across 5 metastatic sites of a 55 year old patient with metastatic prostate cancer at time of rapid autopsy eFigure 12. CT scans from patient PM137, a patient with recurrent platinum refractory metastatic urothelial carcinoma eFigure 13. Tracking tumor genomics between primary and metastatic samples from patient PM12 eFigure 14. -
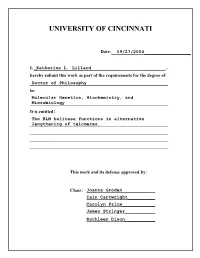
University of Cincinnati
UNIVERSITY OF CINCINNATI Date:__09/27/2004_________________ I, _Katherine L. Lillard___________________________, hereby submit this work as part of the requirements for the degree of: Doctor of Philosophy in: Molecular Genetics, Biochemistry, and Microbiology It is entitled: The BLM helicase functions in alternative lengthening of telomeres. This work and its defense approved by: Chair: Joanna Groden____________ Iain Cartwright__________ Carolyn Price____________ James Stringer___________ Kathleen Dixon___________ THE BLM HELICASE FUNCTIONS IN ALTERNATIVE LENGTHENING OF TELOMERES A dissertation submitted to the Division of Research and Advanced Studies Of the University of Cincinnati in partial fulfillment of the requirements for the degree of DOCTORATE OF PHILOSOPHY (Ph.D.) In the Department of Molecular Genetics, Biochemistry & Microbiology Of the College of Medicine 2004 by Kate Lillard-Wetherell B.S., University of Texas at Austin, 1998 Committee Chair: Joanna Groden, Ph.D. ABSTRACT Somatic cells from persons with the inherited chromosome breakage syndrome Bloom syndrome (BS) feature excessive chromosome breakage, intra-and inter- chromosomal homologous exchanges and telomeric associations. The gene mutated in BS, BLM, encodes a RecQ-like ATP-dependent 3’-to-5’ helicase that presumably functions in some types of DNA transactions. As the absence of BLM is associated with excessive recombination, in vitro experiments have tested the ability of BLM to suppress recombination and/or resolve recombination intermediates. In vitro, BLM promotes branch migration of Holliday junctions, resolves D-loops and unwinds G-quadruplex DNA. A function for BLM in maintaining telomeres is suggested by the latter, since D- loops and perhaps G-quadruplex structures are thought to be present at telomeres. In the present study, the association of BLM with telomeres was investigated. -

Contribution of DNA Double-Strand Break Repair Gene XRCC3 Genotypes to Oral Cancer Susceptibility in Taiwan
ANTICANCER RESEARCH 34: 2951-2956 (2014) Contribution of DNA Double-strand Break Repair Gene XRCC3 Genotypes to Oral Cancer Susceptibility in Taiwan CHIA-WEN TSAI1,3, WEN-SHIN CHANG2,3, JUHN-CHERNG LIU2,3, MING-HSUI TSAI3, CHENG-CHIEH LIN3,4 and DA-TIAN BAU1,2,3 Graduate Institutes of 1Basic Medical Science and 2Clinic Medical Science, China Medical University, Taichung, Taiwan, R.O.C.; 3Terry Fox Cancer Research Laboratory, Department of Medical Research, in China Medical University Hospital, Taichung, Taiwan, R.O.C.; 4Asia University, Taichung, Taiwan, R.O.C. Abstract. The DNA repair gene X-ray repair cross and neck cancers in Taiwan (2). Three major lifestyle factors, complementing protein 3 (XRCC3) is thought to play a major namely the use of tobacco, alcohol and betel nuts, are main role in double-strand break repair and in maintaining causes of oral cancer in Taiwan, while the genomic etiology genomic stability. Very possibly, defective double-strand of oral cancer is of great interest but largely unknown. break repair of cells can lead to carcinogenesis. Therefore, a Human DNA repair mechanisms protect the genome from case–control study was performed to reveal the contribution various insults caused by endogenous and exogenous DNA- of XRCC3 genotypes to individual oral cancer susceptibility. damaging agents (3) and defects in the DNA repair system In this hospital-based research, the association of XRCC3 are thought to be essential in tumorigenesis (4, 5). Therefore, rs1799794, rs45603942, rs861530, rs3212057, rs1799796, it is logical to suspect that some genetic variants of DNA rs861539, rs28903081 genotypes with oral cancer risk in a repair genes might contribute to oral cancer pathogenesis. -

Differential Expression of Thymic DNA Repair Genes in Low-Dose-Rate Irradiated AKR/J Mice
pISSN 1229-845X, eISSN 1976-555X JOURNAL OF J. Vet. Sci. (2013), 14(3), 271-279 http://dx.doi.org/10.4142/jvs.2013.14.3.271 Veterinary Received: 9 Mar. 2012, Revised: 19 Sep. 2012, Accepted: 23 Oct. 2012 Science Original Article Differential expression of thymic DNA repair genes in low-dose-rate irradiated AKR/J mice Jin Jong Bong1, Yu Mi Kang1, Suk Chul Shin1, Seung Jin Choi1, Kyung Mi Lee2,*, Hee Sun Kim1,* 1Radiation Health Research Institute, Korea Hydro and Nuclear Power, Seoul 132-703, Korea 2Global Research Lab, BAERI Institute, Department of Biochemistry and Molecular Biology, Korea University College of Medicine, Seoul 136-705, Korea We previously determined that AKR/J mice housed in a harmful to human life. For example, LDR irradiation low-dose-rate (LDR) (137Cs, 0.7 mGy/h, 2.1 Gy) γ-irradiation therapy for cancer is known to stimulate antioxidant facility developed less spontaneous thymic lymphoma and capacity, repair of DNA damage, apoptosis, and induction survived longer than those receiving sham or high-dose-rate of immune responses [4], and LDR irradiation has been (HDR) (137Cs, 0.8 Gy/min, 4.5 Gy) radiation. Interestingly, shown to mitigate lymphomagenesis and prolong the life histopathological analysis showed a mild lymphomagenesis in span of AKR/J mice [17,18]. Conversely, low-dose (LD) the thymus of LDR-irradiated mice. Therefore, in this study, we irradiation is reportedly involved in carcinogenesis, and LD investigated whether LDR irradiation could trigger the irradiation (lower than 2.0 Gy) has been shown to promote expression of thymic genes involved in the DNA repair process tumor growth and metastasis by enhancing angiogenesis of AKR/J mice. -

(EZH2) Genotypes with Bladder Cancer Risk in Taiwan
ANTICANCER RESEARCH 36 : 4509-4514 (2016) doi:10.21873/anticanres.10997 Association of Enhancer of Zeste 2 ( EZH2 ) Genotypes with Bladder Cancer Risk in Taiwan WEN-SHIN CHANG 1,2* , CHENG-HSI LIAO 1,2,3,8* , CHIA-WEN TSAI 2* , PEI-SHIN HU 2,4 , HSI-CHIN WU 2, SHIH-WEI HSU 1,2,3,8 , CHIEH-LUN HSIAO 1,2 , CHANG-HSIEN HSU 5, YI-WEN HUNG 6 and DA-TIAN BAU 1,2,7 1Graduate Institute of Clinical Medical Science, China Medical University, Taichung, Taiwan, R.O.C.; 2Terry Fox Cancer Research Laboratory, China Medical University Hospital, Taichung, Taiwan, R.O.C.; 3Taichung Armed Forces General Hospital, Taichung, Taiwan, R.O.C.; 4Department of Ophthalmology, Changhua Christian Hospital, Changhua, Taiwan, R.O.C.; Departments of 5Business Administration, and 7Bioinformatics and Medical Engineering, Asia University, Taichung, Taiwan, R.O.C.; 6Department of Medicine Research, Taichung Veterans General Hospital, Taichung, Taiwan, R.O.C.; 8National Defence Medical Center, Taipei, Taiwan, R.O.C. Abstract. Aim: Bladder cancer is the sixth most common associated with the lower risk of bladder cancer development, cancer worldwide and its incidence is particularly high in especially among non-smokers. many developed regions including southwestern Taiwan. However, the genetic contribution to the etiology of bladder Bladder cancer is the most serious urinary neoplasm cancer is not well-understood. The aim of this study was to worldwide, with high incidence rates of approximately evaluate the association of the enhancer of zeste homolog 2 10/100,000 and 3/100,000 in more and less developed (EZH2) genotypes with Taiwan bladder cancer risk.