1 the Honorable Mark Warner the Honorable Bill Cassidy United
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Term Potomac the FALL 2009
The FALL 2009 THE POTOMAC SCHOOL NONPROFIT ORG. Potomac 1301 Potomac School Road U.S. Postage McLean, VA 22101 PAID Rochester, NY www.potomacschool.org Term Permit No. 357 THE ALUMNI MAGAZINE OF THE POTOMAC SCHOOL THE CRAFT OF The Craft TEACHING of Teaching THE OF CRAFT • Annual Report TEACHING For more information, visit our Web site at www.potomacschool.org. ANNUAL REPORT 2008–2009 • OCTOBER 2 NOVEMBER 27 DECEMBER 5 Fall • • • LOWER SCHOOL ALUMNI SQUASH, REVELS 2009 DEDICATION 10:00 AM BASKETBALL, AND FOOTBALL GAMES 11:00 AM – 2:00 PM P65047_CVR.indd 1 8/26/09 3:40:41 PM THE ANNUAL HEAD OF SCHOOL The Potomac Term Geoff rey A. Jones 1301 Potomac School Road McLean VA 22101 FUND DIRECTOR OF COMMUNICATIONS Tel: 703-356-4100 Jill Lucas Fax: 703-749-6308 JULY 1, 2009 – www.potomacschool.org MANAGING EDITOR JUNE 30, 2010 THE POTOMAC TERM is published twice a year. Maria Cecil Send letters, comments and article submissions to the address above, or email to [email protected]. ART DIRECTION & DESIGN Catalone Design Co. LLC Alumni inquiries should be directed to The Potomac School Alumni Offi ce at [email protected]. CONTRIBUTING WRITERS Maria Cecil • Jill Lucas • Suzanne Marshall • Betty Miracle [Cover] Rising fi fth grader Tarik Lamech works with Middle School Cort Morgan • Charlotte Nelsen • Sheila O’Marah Science teacher Greg Mueller. CONTRIBUTING PHOTOGRAPHERS Deborah Kolt • Bern Hoff mann • Development staff • Art faculty This issue of The Potomac Term has been printed on Forest Stewardship Council (FSC) certifi ed paper, which sets the highest social and environmental standards in the paper market. -

Key Committees 2021
Key Committees 2021 Senate Committee on Appropriations Visit: appropriations.senate.gov Majority Members Minority Members Patrick J. Leahy, VT, Chairman Richard C. Shelby, AL, Ranking Member* Patty Murray, WA* Mitch McConnell, KY Dianne Feinstein, CA Susan M. Collins, ME Richard J. Durbin, IL* Lisa Murkowski, AK Jack Reed, RI* Lindsey Graham, SC* Jon Tester, MT Roy Blunt, MO* Jeanne Shaheen, NH* Jerry Moran, KS* Jeff Merkley, OR* John Hoeven, ND Christopher Coons, DE John Boozman, AR Brian Schatz, HI* Shelley Moore Capito, WV* Tammy Baldwin, WI* John Kennedy, LA* Christopher Murphy, CT* Cindy Hyde-Smith, MS* Joe Manchin, WV* Mike Braun, IN Chris Van Hollen, MD Bill Hagerty, TN Martin Heinrich, NM Marco Rubio, FL* * Indicates member of Labor, Health and Human Services, Education, and Related Agencies Subcommittee, which funds IMLS - Final committee membership rosters may still be being set “Key Committees 2021” - continued: Senate Committee on Health, Education, Labor, and Pensions Visit: help.senate.gov Majority Members Minority Members Patty Murray, WA, Chairman Richard Burr, NC, Ranking Member Bernie Sanders, VT Rand Paul, KY Robert P. Casey, Jr PA Susan Collins, ME Tammy Baldwin, WI Bill Cassidy, M.D. LA Christopher Murphy, CT Lisa Murkowski, AK Tim Kaine, VA Mike Braun, IN Margaret Wood Hassan, NH Roger Marshall, KS Tina Smith, MN Tim Scott, SC Jacky Rosen, NV Mitt Romney, UT Ben Ray Lujan, NM Tommy Tuberville, AL John Hickenlooper, CO Jerry Moran, KS “Key Committees 2021” - continued: Senate Committee on Finance Visit: finance.senate.gov Majority Members Minority Members Ron Wyden, OR, Chairman Mike Crapo, ID, Ranking Member Debbie Stabenow, MI Chuck Grassley, IA Maria Cantwell, WA John Cornyn, TX Robert Menendez, NJ John Thune, SD Thomas R. -

Nomination of Dr. Carla D. Hayden, to Be Librarian of Congress
S. HRG. 114–285 NOMINATION OF DR. CARLA D. HAYDEN, TO BE LIBRARIAN OF CONGRESS HEARING BEFORE THE COMMITTEE ON RULES AND ADMINISTRATION CONGRESS OF THE UNITED STATES ONE HUNDRED FOURTEENTH CONGRESS SECOND SESSION APRIL 20, 2016 Printed for the use of the Committee on Rules and Administration ( U.S. GOVERNMENT PUBLISHING OFFICE 20–359 WASHINGTON : 2016 For sale by the Superintendent of Documents, U.S. Government Publishing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 VerDate Sep 11 2014 15:14 Jun 23, 2016 Jkt 097434 PO 00000 Frm 00001 Fmt 5011 Sfmt 5011 C:\DOCS\20359.TXT SHAWN DeShaun on LAP51NQ082 with DISTILLER COMMITTEE ON RULES AND ADMINISTRATION SECOND SESSION ROY BLUNT, Missouri, Chairman LAMAR ALEXANDER, Tennessee CHARLES E. SCHUMER, New York MITCH MCCONNELL, Kentucky DIANNE FEINSTEIN, California THAD COCHRAN, Mississippi RICHARD J. DURBIN, Illinois PAT ROBERTS, Kansas TOM UDALL, New Mexico RICHARD SHELBY, Alabama MARK R. WARNER, Virginia TED CRUZ, Texas PATRICK J. LEAHY, Vermont SHELLEY MOORE CAPITO, West Virginia AMY KLOBUCHAR, Minnesota JOHN BOOZMAN, Arkansas ANGUS S. KING, JR., Maine ROGER WICKER, Mississippi STACY MCHATTON MCBRIDE, Staff Director KELLY L. FADO, Democratic Staff Director (II) VerDate Sep 11 2014 15:14 Jun 23, 2016 Jkt 097434 PO 00000 Frm 00002 Fmt 5904 Sfmt 5904 C:\DOCS\20359.TXT SHAWN DeShaun on LAP51NQ082 with DISTILLER C O N T E N T S OPENING STATEMENT OF: Hon. Roy Blunt, Chairman, a U.S. Senator from the State of Missouri ............ -

Mcconnell Announces Senate Republican Committee Assignments for the 117Th Congress
For Immediate Release, Wednesday, February 3, 2021 Contacts: David Popp, Doug Andres Robert Steurer, Stephanie Penn McConnell Announces Senate Republican Committee Assignments for the 117th Congress Praises Senators Crapo and Tim Scott for their work on the Committee on Committees WASHINGTON, D.C. – Following the 50-50 power-sharing agreement finalized earlier today, Senate Republican Leader Mitch McConnell (R-KY) announced the Senate Republican Conference Committee Assignments for the 117th Congress. Leader McConnell once again selected Senator Mike Crapo (R-ID) to chair the Senate Republicans’ Committee on Committees, the panel responsible for committee assignments for the 117th Congress. This is the ninth consecutive Congress in which Senate leadership has asked Crapo to lead this important task among Senate Republicans. Senator Tim Scott (R-SC) assisted in the committee selection process as he did in the previous three Congresses. “I want to thank Mike and Tim for their work. They have both earned the trust of our colleagues in the Republican Conference by effectively leading these important negotiations in years past and this year was no different. Their trust and experience was especially important as we enter a power-sharing agreement with Democrats and prepare for equal representation on committees,” McConnell said. “I am very grateful for their work.” “I appreciate Leader McConnell’s continued trust in having me lead the important work of the Committee on Committees,” said Senator Crapo. “Americans elected an evenly-split Senate, and working together to achieve policy solutions will be critical in continuing to advance meaningful legislation impacting all Americans. Before the COVID-19 pandemic hit our nation, our economy was the strongest it has ever been. -

November 1, 2019 the Honorable Mark Warner the Honorable Bill Cassidy, MD United States Senate United States Senate 703 Hart S
November 1, 2019 The Honorable Mark Warner The Honorable Bill Cassidy, MD United States Senate United States Senate 703 Hart Senate Office Building 520 Hart Senate Office Building Washington, DC 20510 Washington, DC 20510 The Honorable Chris Van Hollen The Honorable Shelley Moore Capito United States Senate United States Senate 110 Hart Senate Office Building 172 Russell Senate Office Building Washington, DC 20510 Washington, DC 20510 Dear Senators Warner, Cassidy, Van Hollen, and Capito, AcademyHealth, the professional society for health services research and health policy, is writing to thank you for your efforts to reauthorize the Patient-Centered Outcomes Research Institute (PCORI) and provide comment on the recently released discussion draft of the “Patient Centered Outcomes research Institute Reauthorization Act of 2019.” AcademyHealth’s 4,000 members produce and use health services research and are highly engaged with PCORI and its work. Our members informed the creation of PCORI, have served in its leadership, and have received funding support. Our members also have extensive experience in the federal health research ecosystem and value PCORI’s unique contributions to the evidence to improve patient outcomes. We therefore recognize how important it is for Congress to act now to reauthorize PCORI. It must have stable, predictable funding to ensure that the important patient-centered outcomes research and comparative effectiveness research it supports will continue without interruption. AcademyHealth strongly supports the discussion draft, including the modifications to PCORI’s authorizing statute that reflect many of our reauthorization principles, and offers the following comments: Support for a 10-Year Reauthorization of PCORI and Its Current Funding Mechanism PCORI and its Trust Fund were established to provide, stable, predictable funding for patient- centered outcomes research and comparative effectiveness research, as well as the dissemination of that research. -

Using Activists' Pairwise Comparisons to Measure Ideology
Is John McCain more conservative than Rand Paul? Using activists' pairwise comparisons to measure ideology ∗ Daniel J. Hopkins Associate Professor University of Pennsylvania [email protected] Hans Noely Associate Professor Georgetown University [email protected] April 3, 2017 Abstract Political scientists use sophisticated measures to extract the ideology of members of Congress, notably the widely used nominate scores. These measures have known limitations, including possibly obscuring ideological positions that are not captured by roll call votes on the limited agenda presented to legislators. Meanwhile scholars often treat the ideology that is measured by these scores as known or at least knowable by voters and other political actors. It is possible that (a) nominate fails to capture something important in ideological variation or (b) that even if it does measure ideology, sophisticated voters only observe something else. We bring an alternative source of data to this subject, asking samples of highly involved activists to compare pairs of senators to one another or to compare a senator to themselves. From these pairwise comparisons, we can aggregate to a measure of ideology that is comparable to nominate. We can also evaluate the apparent ideological knowledge of our respondents. We find significant differences between nominate scores and the perceived ideology of politically sophisticated activists. ∗DRAFT: PLEASE CONSULT THE AUTHORS BEFORE CITING. Prepared for presentation at the annual meeting of the Midwest Political Science Association in Chicago, April 6-9, 2017. We would like to thank Michele Swers, Jonathan Ladd, and seminar participants at Texas A&M University and Georgetown University for useful comments on earlier versions of this project. -

To: Senator Mark Warner, Senator Tim Kaine, Congressman Ben Cline, Congresswoman Jennifer Wexton CC
To: Senator Mark Warner, Senator Tim Kaine, Congressman Ben Cline, Congresswoman Jennifer Wexton CC: Governor Ralph Northam, Secretary of Transportation Shannon Valentine, Staunton District CTB Member Dixon Whitworth From: Kate Wofford, Executive Director, Alliance for the Shenandoah Valley Keven Walker, Chief Executive Office, Shenandoah Valley Battlefields Foundation 9386 South Congress Street, New Market VA 22844 Date: April 17, 2020 RE: Targeted Approach to Possible Interstate 81 Funds in Federal Infrastructure Package We understand that leaders in Congress and the Administration are in discussion about a possible infrastructure bill as part of the federal response to COVID 19 impacts, as well as possible reauthorization of the federal surface transportation law. We expect that you are receiving a number of requests from localities, constituents, interest groups, and others seeking infrastructure funds for priority projects. We are writing to urge a targeted and well-considered approach to any federal funding for transportation projects in Virginia’s Shenandoah Valley, particularly any funding for projects involving Interstate 81. The I-81 corridor in Virginia can certainly use improvements, and it has been a focus of concern for local and regional travelers for many years. In the past 15 years, there have been a wide range of proposals to address these concerns—some have been simply awful, while others have been fairly good. The awful ones call for extensive, excessive widening of I-81 regardless of the cost to taxpayers, transportation needs, or impacts on communities, health, and natural and historic resources. Among other things, overbuilding on I-81 would degrade the rural character of the corridor— damaging historic resources and streams and destroying productive farmland, homes and businesses. -

May 28,2019 the Honorable Chris Van Hollen United States Senate
May 28,2019 The Honorable Chris Van Hollen The Honorable Elijah Cummings United States Senate United States House of Representatives Washington, DC 20510 Washington, DC 20515 The Honorable Ben Cardin The Honorable John Sarbanes United States Senate United States House of Representatives Washington, DC 20510 Washington, DC 20515 The Honorable C.A. Dutch Ruppersberger United States House of Representatives Washington, DC 20515 Dear Senators Van Hollen and Cardin and Representatives Cummings, Sarbanes, and Ruppersberger: The undersigned organizations, representing patients, cancer care providers, and researchers, are writing to endorse the Henrietta Lacks Enhancing Cancer Research Act of 2019 (S. 946/HR 1966). Clinical trials are vitally important for advancing our knowledge of cancer and cancer treatments and providing patients with potentially life-saving treatment options. We commend your efforts – through a comprehensive review by the Government Accountability Office (GAO) – to understand the reasons for unequal access to cancer trials by racial and ethnic minorities and Americans who live in rural areas, are old and are poor. We are pleased that this legislation is named for Henrietta Lacks, as her name reflects the altruism of clinical trials enrollees, who typically dedicate considerable time and effort to clinical trials participation even as they receive access to investigational agents. The ability to enroll in a clinical trial should beoffered equally to minority patients, those in rural areas, and those who are old and poor. We look forward to the analysis and recommendations from GAO and the reforms that may follow the study recommendations. Our organizations have been engaged for some time in a wide range of efforts to improve the cancer clinical trial enterprise. -

Surname Notes Abbott Family Abbott, James Scotland and Virginia Abel
Surname Notes Abbott Family Abbott, James Scotland and Virginia Abel/Abel - Franklin Families Abshire Family Bedford, Franklin and Tazewell Counties Adams and Vaden Families Adams Family Massachusetts Adams Family Campbell County, Virginia Adams, Lela C. Biography Adams, Thomas Albert 1839-1888 Addison, Lucy Biography 1861-1937 Adkins Family Pittsylvania County, Virginia Adkins, John Ward Airheart/Airhart/Earhart Family Aker, James Biography 1871-1986 Akers Family Floyd County, Virginia Albert Family Alcorn-Lusk Family MSS C-2 Beverly R. Hoch Collection Alderman, Edwin Anderson Biography 1861-1931 Alderman, John Perry Biography - d. 1995 Alderson Family Alexander Family Alexander Family MSS C-2 Beverly R. Hoch Collection Alexander-Gooding Family MSS C-2 Beverly R. Hoch Collection Alford-Liggon Family MSS C-2 Beverly R. Hoch Collection Aliff/Ayliffe Family Allan Family Allen Family Little Creek, Pulaski County, Virginia Carroll County, Virginia - Court Allen Family Proceedings Allen Family MSS C-2 Beverly R. Hoch Collection Allen, Cary Biographty 1767-1795 Allen, George Allen, Robert N. Biography 1889-1831 Allen, Susan Biography Allen, William R. Fluvanna County, Virginia (Oversize File) Allerton Family Alley Family "Allees All Around" Allison Family MSS C-2 Beverly R. Hoch Collection Almond, James Lindsay, Jr. Almond, Russell E,. Biography - d.1905 Alphin Family Alt/Ault Family (Oversize File) Altig/Altick/Altice/Attic Altizer Family Ames Family Ammon Family Ammonet Family Anastasia - Manahan, Mrs. Anna Biography d. 1984 Surname Notes Anderson Family Craig County, Virginia Anderson Family George Smith Anderson (Oversize File) MSS C-2 Beverly R. Hoch Collection (3 Anderson Family folders) Anderson Famiy Prince George County, Virginia Anderson, Wax, Kemper Families Anderson, Cassandra M. -
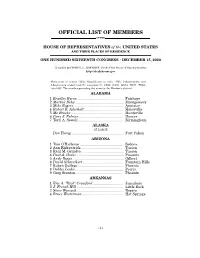
Official List of Members
OFFICIAL LIST OF MEMBERS OF THE HOUSE OF REPRESENTATIVES of the UNITED STATES AND THEIR PLACES OF RESIDENCE ONE HUNDRED SIXTEENTH CONGRESS • DECEMBER 15, 2020 Compiled by CHERYL L. JOHNSON, Clerk of the House of Representatives http://clerk.house.gov Democrats in roman (233); Republicans in italic (195); Independents and Libertarians underlined (2); vacancies (5) CA08, CA50, GA14, NC11, TX04; total 435. The number preceding the name is the Member's district. ALABAMA 1 Bradley Byrne .............................................. Fairhope 2 Martha Roby ................................................ Montgomery 3 Mike Rogers ................................................. Anniston 4 Robert B. Aderholt ....................................... Haleyville 5 Mo Brooks .................................................... Huntsville 6 Gary J. Palmer ............................................ Hoover 7 Terri A. Sewell ............................................. Birmingham ALASKA AT LARGE Don Young .................................................... Fort Yukon ARIZONA 1 Tom O'Halleran ........................................... Sedona 2 Ann Kirkpatrick .......................................... Tucson 3 Raúl M. Grijalva .......................................... Tucson 4 Paul A. Gosar ............................................... Prescott 5 Andy Biggs ................................................... Gilbert 6 David Schweikert ........................................ Fountain Hills 7 Ruben Gallego ............................................ -

9660 Hon. Chris Van Hollen Hon. Allyson Y. Schwartz
9660 EXTENSIONS OF REMARKS May 13, 2005 Social Security, but to push its social agen- Mr. Speaker, it is my hope that all Ameri- and Democrats, through many different admin- da, the so-called ‘‘ownership society.’’ cans will join me in congratulating the citizens istrations and many different times. I am proud Funny, median family income adjusted for inflation—the most important measure of of Israel and the entire Jewish community on that this support remains so strong today. how typical Americans are doing—has fallen the 57th anniversary of the birth of the State Mr. Speaker, it is truly an honor to stand by three straight years and is headed for a of Israel. Israel and I know my colleagues join me in ex- fourth as Bush showers tax breaks on compa- f pressing Mazel Tov for a remarkable 57 years. nies that aren’t hiring. Whose ownership so- f ciety is this? IN HONOR OF ISRAELI Democrats and their allies at AARP in the INDEPENDENCE DAY ISRAEL INDEPENDENCE DAY Social Security debate have offered little in the way of real solutions. John Rother, di- rector of policy and strategy for AARP—de- HON. ALLYSON Y. SCHWARTZ HON. ROBERT MENENDEZ fending his hilariously exaggerated, slam- OF PENNSYLVANIA OF NEW JERSEY dunk anti-personal account TV ad cam- IN THE HOUSE OF REPRESENTATIVES IN THE HOUSE OF REPRESENTATIVES paign—told me the idea of allowing the trust Thursday, May 12, 2005 Thursday, May 12, 2005 fund to invest more broadly makes sense. But he said the public isn’t ready for that Ms. -

VOTE! Ning in All Four Jurisdictions in the 8Th Congressional District and Run- Ning First in 133, Or 82 Percent, of the 163 Precincts
Vol. 39, No. 7 www.arlingtondemocrats.org July 2014 Beyer wins all four jurisdictions Don Beyer recorded an impressive primary victory June 10, win- VOTE! ning in all four jurisdictions in the 8th Congressional District and run- ning first in 133, or 82 percent, of the 163 precincts. Overall, Beyer got 46 percent of the vote in the district, not an absolute majority but a very impressive total given that there were SUNDAY seven candidates. Furthermore, he was 28 percentage points ahead of the Number Two candidate, Patrick Hope. (This is no joke) Beyer won in all four jurisdictions in the district, though by widely varying margins. Beyer’s margin was lowest in Arlington where he took 39 percent and was chased closely by Hope with 33 percent. Beyer did better in Alexandria with 44 percent, chased by Adam Ebbin The Republican with 21 percent. Beyer got an absolute majority of 52 percent in speaker of the Fairfax County and ran away with it in Falls Church where he got 72 percent. House of Delegates Hope came in second in both Fairfax and Falls Church, but a has fixed the elec- very distant second with 14 percent and 12 percent respectively. continued on page eight tion to replace Del. Bob Brink for Tues- day, August 19, re- Brink retires after 17 years quiring ACDC to Delegate Bob Brink announced last Friday that he was resigning from the House of Delegates effective Monday, June 30, after 17 years hold its caucus to in office. pick a nominee this Brink, 67, is the senior member among the four delegates repre- senting Arlington.