SEPT2 Is a New Fusion Partner of MLL in Acute Myeloid Leukemia with T (2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![FK506-Binding Protein 12.6/1B, a Negative Regulator of [Ca2+], Rescues Memory and Restores Genomic Regulation in the Hippocampus of Aging Rats](https://docslib.b-cdn.net/cover/6136/fk506-binding-protein-12-6-1b-a-negative-regulator-of-ca2-rescues-memory-and-restores-genomic-regulation-in-the-hippocampus-of-aging-rats-16136.webp)
FK506-Binding Protein 12.6/1B, a Negative Regulator of [Ca2+], Rescues Memory and Restores Genomic Regulation in the Hippocampus of Aging Rats
This Accepted Manuscript has not been copyedited and formatted. The final version may differ from this version. A link to any extended data will be provided when the final version is posted online. Research Articles: Neurobiology of Disease FK506-Binding Protein 12.6/1b, a negative regulator of [Ca2+], rescues memory and restores genomic regulation in the hippocampus of aging rats John C. Gant1, Eric M. Blalock1, Kuey-Chu Chen1, Inga Kadish2, Olivier Thibault1, Nada M. Porter1 and Philip W. Landfield1 1Department of Pharmacology & Nutritional Sciences, University of Kentucky, Lexington, KY 40536 2Department of Cell, Developmental and Integrative Biology, University of Alabama at Birmingham, Birmingham, AL 35294 DOI: 10.1523/JNEUROSCI.2234-17.2017 Received: 7 August 2017 Revised: 10 October 2017 Accepted: 24 November 2017 Published: 18 December 2017 Author contributions: J.C.G. and P.W.L. designed research; J.C.G., E.M.B., K.-c.C., and I.K. performed research; J.C.G., E.M.B., K.-c.C., I.K., and P.W.L. analyzed data; J.C.G., E.M.B., O.T., N.M.P., and P.W.L. wrote the paper. Conflict of Interest: The authors declare no competing financial interests. NIH grants AG004542, AG033649, AG052050, AG037868 and McAlpine Foundation for Neuroscience Research Corresponding author: Philip W. Landfield, [email protected], Department of Pharmacology & Nutritional Sciences, University of Kentucky, 800 Rose Street, UKMC MS 307, Lexington, KY 40536 Cite as: J. Neurosci ; 10.1523/JNEUROSCI.2234-17.2017 Alerts: Sign up at www.jneurosci.org/cgi/alerts to receive customized email alerts when the fully formatted version of this article is published. -

Bayesian Hierarchical Modeling of High-Throughput Genomic Data with Applications to Cancer Bioinformatics and Stem Cell Differentiation
BAYESIAN HIERARCHICAL MODELING OF HIGH-THROUGHPUT GENOMIC DATA WITH APPLICATIONS TO CANCER BIOINFORMATICS AND STEM CELL DIFFERENTIATION by Keegan D. Korthauer A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Statistics) at the UNIVERSITY OF WISCONSIN–MADISON 2015 Date of final oral examination: 05/04/15 The dissertation is approved by the following members of the Final Oral Committee: Christina Kendziorski, Professor, Biostatistics and Medical Informatics Michael A. Newton, Professor, Statistics Sunduz Kele¸s,Professor, Biostatistics and Medical Informatics Sijian Wang, Associate Professor, Biostatistics and Medical Informatics Michael N. Gould, Professor, Oncology © Copyright by Keegan D. Korthauer 2015 All Rights Reserved i in memory of my grandparents Ma and Pa FL Grandma and John ii ACKNOWLEDGMENTS First and foremost, I am deeply grateful to my thesis advisor Christina Kendziorski for her invaluable advice, enthusiastic support, and unending patience throughout my time at UW-Madison. She has provided sound wisdom on everything from methodological principles to the intricacies of academic research. I especially appreciate that she has always encouraged me to eke out my own path and I attribute a great deal of credit to her for the successes I have achieved thus far. I also owe special thanks to my committee member Professor Michael Newton, who guided me through one of my first collaborative research experiences and has continued to provide key advice on my thesis research. I am also indebted to the other members of my thesis committee, Professor Sunduz Kele¸s,Professor Sijian Wang, and Professor Michael Gould, whose valuable comments, questions, and suggestions have greatly improved this dissertation. -

Supplementary Information Integrative Analyses of Splicing in the Aging Brain: Role in Susceptibility to Alzheimer’S Disease
Supplementary Information Integrative analyses of splicing in the aging brain: role in susceptibility to Alzheimer’s Disease Contents 1. Supplementary Notes 1.1. Religious Orders Study and Memory and Aging Project 1.2. Mount Sinai Brain Bank Alzheimer’s Disease 1.3. CommonMind Consortium 1.4. Data Availability 2. Supplementary Tables 3. Supplementary Figures Note: Supplementary Tables are provided as separate Excel files. 1. Supplementary Notes 1.1. Religious Orders Study and Memory and Aging Project Gene expression data1. Gene expression data were generated using RNA- sequencing from Dorsolateral Prefrontal Cortex (DLPFC) of 540 individuals, at an average sequence depth of 90M reads. Detailed description of data generation and processing was previously described2 (Mostafavi, Gaiteri et al., under review). Samples were submitted to the Broad Institute’s Genomics Platform for transcriptome analysis following the dUTP protocol with Poly(A) selection developed by Levin and colleagues3. All samples were chosen to pass two initial quality filters: RNA integrity (RIN) score >5 and quantity threshold of 5 ug (and were selected from a larger set of 724 samples). Sequencing was performed on the Illumina HiSeq with 101bp paired-end reads and achieved coverage of 150M reads of the first 12 samples. These 12 samples will serve as a deep coverage reference and included 2 males and 2 females of nonimpaired, mild cognitive impaired, and Alzheimer's cases. The remaining samples were sequenced with target coverage of 50M reads; the mean coverage for the samples passing QC is 95 million reads (median 90 million reads). The libraries were constructed and pooled according to the RIN scores such that similar RIN scores would be pooled together. -
Cell Type-Specific Gene Expression Patterns Associated with Posttraumatic Stress Disorder in World Trade Center Responders
Kuan et al. Translational Psychiatry (2019) 9:1 https://doi.org/10.1038/s41398-018-0355-8 Translational Psychiatry ARTICLE Open Access Cell type-specific gene expression patterns associated with posttraumatic stress disorder in World Trade Center responders Pei-Fen Kuan1, Xiaohua Yang2,SeanClouston 3,XuRen1,RomanKotov4, Monika Waszczuk4,PrashantK.Singh5, Sean T. Glenn5, Eduardo Cortes Gomez 6, Jianmin Wang6,EvelynBromet4 and Benjamin J. Luft2 Abstract Posttraumatic stress disorder (PTSD), a chronic disorder resulting from severe trauma, has been linked to immunologic dysregulation. Gene expression profiling has emerged as a promising tool for understanding the pathophysiology of PTSD. However, to date, all but one gene expression study was based on whole blood or unsorted peripheral blood mononuclear cell (PBMC), a complex tissue consisting of several populations of cells. The objective of this study was to utilize RNA sequencing to simultaneously profile the gene expression of four immune cell subpopulations (CD4T, CD8T, B cells, and monocytes) in 39 World Trade Center responders (20 with and 19 without PTSD) to determine which immune subsets play a role in the transcriptomic changes found in whole blood. Transcriptome-wide analyses identified cell-specific and shared differentially expressed genes across the four cell types. FKBP5 and PI4KAP1 genes were consistently upregulated across all cell types. Notably, REST and SEPT4, genes linked to neurodegeneration, were among the top differentially expressed genes in monocytes. Pathway analyses identified differentially expressed gene sets involved in mast cell activation and regulation in CD4T, interferon-beta production in CD8T, and neutrophil- fi 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; related gene sets in monocytes. -

Chromatin Dysregulation and DNA Methylation at Transcription Start Sites Associated with Transcriptional Repression in Cancers
Corrected: Publisher correction ARTICLE https://doi.org/10.1038/s41467-019-09937-w OPEN Chromatin dysregulation and DNA methylation at transcription start sites associated with transcriptional repression in cancers Mizuo Ando 1,2, Yuki Saito1,2, Guorong Xu3, Nam Q. Bui 4,5, Kate Medetgul-Ernar1, Minya Pu1, Kathleen Fisch 3, Shuling Ren1, Akihiro Sakai1, Takahito Fukusumi1, Chao Liu1, Sunny Haft1, John Pang1, Adam Mark3, Daria A. Gaykalova6, Theresa Guo6, Alexander V. Favorov 7,8, Srinivasan Yegnasubramanian7, Elana J. Fertig7, Patrick Ha 9, Pablo Tamayo 1, Tatsuya Yamasoba 2, Trey Ideker4, Karen Messer1 & Joseph A. Califano1,10 1234567890():,; Although promoter-associated CpG islands have been established as targets of DNA methylation changes in cancer, previous studies suggest that epigenetic dysregulation out- side the promoter region may be more closely associated with transcriptional changes. Here we examine DNA methylation, chromatin marks, and transcriptional alterations to define the relationship between transcriptional modulation and spatial changes in chromatin structure. Using human papillomavirus-related oropharyngeal carcinoma as a model, we show aberrant enrichment of repressive H3K9me3 at the transcriptional start site (TSS) with methylation- associated, tumor-specific gene silencing. Further analysis identifies a hypermethylated subtype which shows a functional convergence on MYC targets and association with CREBBP/EP300 mutation. The tumor-specific shift to transcriptional repression associated with DNA methylation at TSSs was confirmed in multiple tumor types. Our data may show a common underlying epigenetic dysregulation in cancer associated with broad enrichment of repressive chromatin marks and aberrant DNA hypermethylation at TSSs in combination with MYC network activation. 1 Moores Cancer Center, University of California San Diego, 3855 Health Sciences Dr, La Jolla, CA 92093, USA. -

Atherosclerosis-Susceptible and Atherosclerosis-Resistant Pigeon Aortic Cells Express Different Genes in Vivo
University of New Hampshire University of New Hampshire Scholars' Repository New Hampshire Agricultural Experiment Station Publications New Hampshire Agricultural Experiment Station 7-1-2013 Atherosclerosis-susceptible and atherosclerosis-resistant pigeon aortic cells express different genes in vivo Janet L. Anderson University of New Hampshire, [email protected] C. M. Ashwell University of New Hampshire - Main Campus S. C. Smith University of New Hampshire - Main Campus R. Shine University of New Hampshire - Main Campus E. C. Smith University of New Hampshire - Main Campus See next page for additional authors Follow this and additional works at: https://scholars.unh.edu/nhaes Part of the Poultry or Avian Science Commons Recommended Citation J. L. Anderson, C. M. Ashwell, S. C. Smith, R. Shine, E. C. Smith and R. L. Taylor, Jr. Atherosclerosis- susceptible and atherosclerosis-resistant pigeon aortic cells express different genes in vivo Poultry Science (2013) 92 (10): 2668-2680 doi:10.3382/ps.2013-03306 This Article is brought to you for free and open access by the New Hampshire Agricultural Experiment Station at University of New Hampshire Scholars' Repository. It has been accepted for inclusion in New Hampshire Agricultural Experiment Station Publications by an authorized administrator of University of New Hampshire Scholars' Repository. For more information, please contact [email protected]. Authors Janet L. Anderson, C. M. Ashwell, S. C. Smith, R. Shine, E. C. Smith, and Robert L. Taylor Jr. This article is available at University of New Hampshire Scholars' Repository: https://scholars.unh.edu/nhaes/207 Atherosclerosis-susceptible and atherosclerosis-resistant pigeon aortic cells express different genes in vivo J. -

Protein Kinase A-Mediated Septin7 Phosphorylation Disrupts Septin Filaments and Ciliogenesis
cells Article Protein Kinase A-Mediated Septin7 Phosphorylation Disrupts Septin Filaments and Ciliogenesis Han-Yu Wang 1,2, Chun-Hsiang Lin 1, Yi-Ru Shen 1, Ting-Yu Chen 2,3, Chia-Yih Wang 2,3,* and Pao-Lin Kuo 1,2,4,* 1 Department of Obstetrics and Gynecology, College of Medicine, National Cheng Kung University, Tainan 701, Taiwan; [email protected] (H.-Y.W.); [email protected] (C.-H.L.); [email protected] (Y.-R.S.) 2 Institute of Basic Medical Sciences, College of Medicine, National Cheng Kung University, Tainan 701, Taiwan; [email protected] 3 Department of Cell Biology and Anatomy, College of Medicine, National Cheng Kung University, Tainan 701, Taiwan 4 Department of Obstetrics and Gynecology, National Cheng-Kung University Hospital, Tainan 704, Taiwan * Correspondence: [email protected] (C.-Y.W.); [email protected] (P.-L.K.); Tel.: +886-6-2353535 (ext. 5338); (C.-Y.W.)+886-6-2353535 (ext. 5262) (P.-L.K.) Abstract: Septins are GTP-binding proteins that form heteromeric filaments for proper cell growth and migration. Among the septins, septin7 (SEPT7) is an important component of all septin filaments. Here we show that protein kinase A (PKA) phosphorylates SEPT7 at Thr197, thus disrupting septin filament dynamics and ciliogenesis. The Thr197 residue of SEPT7, a PKA phosphorylating site, was conserved among different species. Treatment with cAMP or overexpression of PKA catalytic subunit (PKACA2) induced SEPT7 phosphorylation, followed by disruption of septin filament formation. Constitutive phosphorylation of SEPT7 at Thr197 reduced SEPT7-SEPT7 interaction, but did not affect SEPT7-SEPT6-SEPT2 or SEPT4 interaction. -

1 Supporting Information for a Microrna Network Regulates
Supporting Information for A microRNA Network Regulates Expression and Biosynthesis of CFTR and CFTR-ΔF508 Shyam Ramachandrana,b, Philip H. Karpc, Peng Jiangc, Lynda S. Ostedgaardc, Amy E. Walza, John T. Fishere, Shaf Keshavjeeh, Kim A. Lennoxi, Ashley M. Jacobii, Scott D. Rosei, Mark A. Behlkei, Michael J. Welshb,c,d,g, Yi Xingb,c,f, Paul B. McCray Jr.a,b,c Author Affiliations: Department of Pediatricsa, Interdisciplinary Program in Geneticsb, Departments of Internal Medicinec, Molecular Physiology and Biophysicsd, Anatomy and Cell Biologye, Biomedical Engineeringf, Howard Hughes Medical Instituteg, Carver College of Medicine, University of Iowa, Iowa City, IA-52242 Division of Thoracic Surgeryh, Toronto General Hospital, University Health Network, University of Toronto, Toronto, Canada-M5G 2C4 Integrated DNA Technologiesi, Coralville, IA-52241 To whom correspondence should be addressed: Email: [email protected] (M.J.W.); yi- [email protected] (Y.X.); Email: [email protected] (P.B.M.) This PDF file includes: Materials and Methods References Fig. S1. miR-138 regulates SIN3A in a dose-dependent and site-specific manner. Fig. S2. miR-138 regulates endogenous SIN3A protein expression. Fig. S3. miR-138 regulates endogenous CFTR protein expression in Calu-3 cells. Fig. S4. miR-138 regulates endogenous CFTR protein expression in primary human airway epithelia. Fig. S5. miR-138 regulates CFTR expression in HeLa cells. Fig. S6. miR-138 regulates CFTR expression in HEK293T cells. Fig. S7. HeLa cells exhibit CFTR channel activity. Fig. S8. miR-138 improves CFTR processing. Fig. S9. miR-138 improves CFTR-ΔF508 processing. Fig. S10. SIN3A inhibition yields partial rescue of Cl- transport in CF epithelia. -

Phylogenetic and Evolutionary Analysis of the Septin Protein Family in Metazoan
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector FEBS Letters 581 (2007) 5526–5532 Phylogenetic and evolutionary analysis of the septin protein family in metazoan Lihuan Cao1, Xiangming Ding1, Wenbo Yu, Xianmei Yang, Suqin Shen, Long Yu* State Key Laboratory of Genetic Engineering, Institute of Genetics, School of Life Sciences, Fudan University, Shanghai 200433, PR China Received 9 August 2007; revised 11 October 2007; accepted 19 October 2007 Available online 29 October 2007 Edited by Takashi Gojobori have a P-loop [8,9] which is defined by the Walker A motif Abstract Septins, a conserved family of cytoskeletal GTP- binding proteins, were presented in diverse eukaryotes. Here, a (GxxGxGKST), Walker B motif (DxxG), and the GTP-speci- comprehensive phylogenetic and evolutionary analysis for septin ficity motif (xKxD). Septins differ from most other members of proteins in metazoan was carried out. First, we demonstrated this subclass in that they lack an asparagine at position 1 of the that all septin proteins in metazoan could be clustered into four GTP-specificity motif (i.e. not NKxD, but AKAD or GKAD) subgroups, and the representative homologue of every subgroup [7]. Recently, the crystal structures of the human SEPT2 G was presented in the non-vertebrate chordate Ciona intestinalis, domain and the heterotrimeric human SEPT2-SEPT6-SEPT7 indicating that the emergence of the four septin subgroups should complex had been determined. The septin complex structure have occurred prior to divergence of vertebrates and inverte- revealed a universal bipolar polymer building block, composed brates, and the expansion of the septin gene number in verte- of an extended G domain, which forms oligomers and fila- brates was mainly by the duplication of pre-existing genes ments by conserved interactions between adjacent nucleotide- rather than by the appearance of new septin subgroup. -
Background Methods Conclusions Results
Gene Expression Profiles of Pediatric Tuberculosis Patients and Exposed Controls from India Jeffrey A Tornheim,1 Mandar Paradkar,2 Anil Madugundu,4,5 Nikhil Gupte,2 Vandana Kulkarni,2 Sreelakshmi Sreenivasamurthy,4,5 Remya Raja,4 Neeta Pradhan,2 Shri Vijay Bala Yogendra Shivakumar,6 Chhaya Valvi,3 Rewa Kohli,2 Padmapriyadarsini Chandrasekaran,7 Vidya Mave,2 Akhilesh Pandey,4,5 and Amita Gupta1 1Center for Clinical Global Health Education, Division of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore, MD, USA, 2Byramjee Jeejeebhoy Government Medical College – Johns Hopkins University Clinical Research Site, Pune, Maharashtra, India, 3Byramjee Jeejeebhoy Government Medical College, Pune, Maharashtra, India, 4National Institute of Mental Health and Neurosciences - Institute of Bioinformatics Lab, Bangalore, India, 5Institute of Genetic Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, USA, 6Johns Hopkins University – India office (CCGHE), Pune, Maharashtra, India, 7National Institute for Research in Tuberculosis, Chennai, Tamil Nadu, India BACKGROUND RESULTS—Differential Gene Expression Tuberculosis (TB) is the #1 infectious disease killer worldwide, and 27% of cases are in India (WHO 2016). Aim 1: Differential gene expression between pediatric cases (N=16) and controls (N=32) at enrollment Children frequently have either paucibacillary disease, are too young to provide adequate sputum Gene Counts Fold Change Distribution samples, or develop extrapulmonary disease, forcing clinicians to rely on diagnostic tests with poor sensitivity and frequent presumptive treatment for TB in children (Perez-Velez NEJM 2012). Several studies have attempted to use biomarkers of host response to infection as an alternative means of Number of Differentially Expressed Genes between Cases and Controls, diagnosing TB, but these studies have not included many children, Indian patients, or microbiologically by False Discovery Rate (FDR) and Log2-Fold Change Any Log2 >0.5 Log2 >1.0 Log2 >1.5 Log2 >2.0 confirmed patients. -

The Requirement of SEPT2 and SEPT7 for Migration and Invasion in Human Breast Cancer Via MEK/ERK Activation
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 7, No. 38 Research Paper The requirement of SEPT2 and SEPT7 for migration and invasion in human breast cancer via MEK/ERK activation Nianzhu Zhang1,*, Lu Liu2,*, Ning Fan2, Qian Zhang1, Weijie Wang1, Mingnan Zheng3, Lingfei Ma4, Yan Li2, Lei Shi1,5 1Institute of Cancer Stem Cell, Cancer Center, Dalian Medical University, Dalian, 116044, Liaoning, P.R.China 2College of Basic Medical Sciences, Dalian Medical University, Dalian, 116044 Liaoning, P.R.China 3Department of Gynecology and Obstetrics, Dalian Municipal Central Hospital Affiliated to Dalian Medical University, Dalian, 116033, Liaoning, P.R.China 4The First Affiliated Hospital of Dalian Medical University, Dalian, 116011, Liaoning, P.R.China 5State Key Laboratory of Drug Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Shanghai, 201203, P.R.China *These authors contributed equally to this work Correspondence to: Lei Shi, email: [email protected] Yan Li, email: [email protected] Lingfei Ma, email: [email protected] Keywords: septin, forchlorfenuron, breast cancer, invasion, MAPK Received: April 24, 2016 Accepted: July 28, 2016 Published: August 19, 2016 ABSTRACT Septins are a novel class of GTP-binding cytoskeletal proteins evolutionarily conserved from yeast to mammals and have now been found to play a contributing role in a broad range of tumor types. However, their functional importance in breast cancer remains largely unclear. Here, we demonstrated that pharmaceutical inhibition of global septin dynamics would greatly suppress proliferation, migration and invasiveness in breast cancer cell lines. We then examined the expression and subcellular distribution of the selected septins SEPT2 and SEPT7 in breast cancer cells, revealing a rather variable localization of the two proteins with cell cycle progression. -
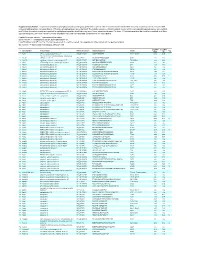
Supplementary Table 1
Supplementary Table 1. Large-scale quantitative phosphoproteomic profiling was performed on paired vehicle- and hormone-treated mTAL-enriched suspensions (n=3). A total of 654 unique phosphopeptides corresponding to 374 unique phosphoproteins were identified. The peptide sequence, phosphorylation site(s), and the corresponding protein name, gene symbol, and RefSeq Accession number are reported for each phosphopeptide identified in any one of three experimental pairs. For those 414 phosphopeptides that could be quantified in all three experimental pairs, the mean Hormone:Vehicle abundance ratio and corresponding standard error are also reported. Peptide Sequence column: * = phosphorylated residue Site(s) column: ^ = ambiguously assigned phosphorylation site Log2(H/V) Mean and SE columns: H = hormone-treated, V = vehicle-treated, n/a = peptide not observable in all 3 experimental pairs Sig. column: * = significantly changed Log 2(H/V), p<0.05 Log (H/V) Log (H/V) # Gene Symbol Protein Name Refseq Accession Peptide Sequence Site(s) 2 2 Sig. Mean SE 1 Aak1 AP2-associated protein kinase 1 NP_001166921 VGSLT*PPSS*PK T622^, S626^ 0.24 0.95 PREDICTED: ATP-binding cassette, sub-family A 2 Abca12 (ABC1), member 12 XP_237242 GLVQVLS*FFSQVQQQR S251^ 1.24 2.13 3 Abcc10 multidrug resistance-associated protein 7 NP_001101671 LMT*ELLS*GIRVLK T464, S468 -2.68 2.48 4 Abcf1 ATP-binding cassette sub-family F member 1 NP_001103353 QLSVPAS*DEEDEVPVPVPR S109 n/a n/a 5 Ablim1 actin-binding LIM protein 1 NP_001037859 PGSSIPGS*PGHTIYAK S51 -3.55 1.81 6 Ablim1 actin-binding