Communicable Disease Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Picture of the Month
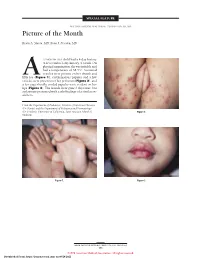
SPECIAL FEATURE SECTION EDITOR: WALTER W. TUNNESSEN, JR, MD Picture of the Month Kevin A. Slavin, MD; Ilona J. Frieden, MD 15-MONTH-OLD child had a 4-day history of fever and a 1-day history of a rash. On physical examination she was irritable and had a temperature of 38.3°C. Scattered vesicles were present on her thumb and Afifth toe (Figure 1), erythematous papules and a few vesicles were present over her perineum (Figure 2), and a few superficially eroded papules were evident on her lips (Figure 3). The lesions were gone 3 days later, but a playmate presented with early findings of a similar ex- anthem. From the Department of Pediatrics, Division of Infectious Diseases (Dr Slavin) and the Department of Pediatrics and Dermatology (Dr Frieden), University of California, San Francisco School of Figure 2. Medicine. Figure 1. Figure 3. ARCH PEDIATR ADOLESC MED/ VOL 152, MAY 1998 505 ©1998 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/28/2021 Denouement and Discussion Hand-Foot-and-Mouth Disease Figure 1. Vesicles are present on the thumb and fifth toe. foot-and-mouth disease).1,2,5-9 The lesions on the but- tocks are of the same size and typical of the early forms Figure 2. Multiple erythematous papules and a few scattered vesicles are of the exanthem, but they are not frequently vesicular present over the perineum. in nature. Lesions involving the perineum seem to be more Figure 3. Superficially eroded papules are present on the lips. common in children who wear diapers, suggesting that friction or minor trauma may play a role in the develop- ment of lesions. -

Expanding the Role of Dermatology at the World Health Organization and Beyond
EDITORIAL A Seat at the Big Table: Expanding the Role of Dermatology at the World Health Organization and Beyond y patient can’t breathe. From across Kaposi’s sarcoma, seborrheic dermatitis, her- the busy, open ward, you can see the pes zoster, scabies, papular pruritic eruption, Mplaques of Kaposi’s sarcoma riddling eosinophilic folliculitis, tinea, molluscum, drug her skin. The impressive woody edema has reactions, and oral candidiasis (World Health enlarged her legs to the size of small tree trunks. Organization, in press). These conditions have We don’t have access to confirmatory pulmo- a high prevalence in developing countries, but nary testing in Kenya, but she probably wouldn’t many lack internationally agreed-on standards survive a bronchoscopy anyway. of care. This deficit led to inconsistent and some- When she dies six hours later, we can be pret- times dangerous treatment approaches or lack of ty sure that it is her pulmonary Kaposi’s sarcoma, essential drugs. Critically, dermatologists were along with her underlying HIV, that killed her. involved at all levels of the guideline-develop- Her family tells us that she had dark spots on ment process, including Cochrane reviews of the her skin and swelling in her legs for more than literature, guideline development and review, a year before she presented to the hospital. Like and additional funding for the project from many of our patients in East Africa, she sought the International Foundation for Dermatology help from a traditional healer for many months (http://www.ifd.org). before turning to the biomedical health system, Although diseases such as Kaposi’s sarcoma only hours before her death. -

Communicable Disease Chart
COMMON INFECTIOUS ILLNESSES From birth to age 18 Disease, illness or organism Incubation period How is it spread? When is a child most contagious? When can a child return to the Report to county How to prevent spreading infection (management of conditions)*** (How long after childcare center or school? health department* contact does illness develop?) To prevent the spread of organisms associated with common infections, practice frequent hand hygiene, cover mouth and nose when coughing and sneezing, and stay up to date with immunizations. Bronchiolitis, bronchitis, Variable Contact with droplets from nose, eyes or Variable, often from the day before No restriction unless child has fever, NO common cold, croup, mouth of infected person; some viruses can symptoms begin to 5 days after onset or is too uncomfortable, fatigued ear infection, pneumonia, live on surfaces (toys, tissues, doorknobs) or ill to participate in activities sinus infection and most for several hours (center unable to accommodate sore throats (respiratory diseases child’s increased need for comfort caused by many different viruses and rest) and occasionally bacteria) Cold sore 2 days to 2 weeks Direct contact with infected lesions or oral While lesions are present When active lesions are no longer NO Avoid kissing and sharing drinks or utensils. (Herpes simplex virus) secretions (drooling, kissing, thumb sucking) present in children who do not have control of oral secretions (drooling); no exclusions for other children Conjunctivitis Variable, usually 24 to Highly contagious; -

Infectious Disease
INFECTIOUS DISEASE Infectious diseases are caused by germs that are transmitted directly from person to NOTE: person; animal to person (zoonotic The following symbols are used throughout this Community Health Assessment Report to serve only as a simple and quick diseases); from mother to unborn child; or reference for data comparisons and trends for the County. indirectly, such as when a person touches Further analysis may be required before drawing conclusions about the data. a surface that some germs can linger on. The NYSDOH recommends several The apple symbol represents areas in which Oneida County’s status or trend is FAVORABLE or COMPARABLE to its effective strategies for preventing comparison (i.e., NYS, US) or areas/issues identified as infectious diseases,, including: ensuring STRENGTHS. procedures and systems are in place in The magnifying glass symbols represent areas in which Oneida County’s status or trend is UNFAVORABLE to its communities for immunizations to be up to comparison (i.e., NYS, US) or areas/issues of CONCERN date; enabling sanitary practices by or NEED that may warrant further analysis. conveniently located sinks for washing DATA REFERENCES: hands; influencing community resources • All References to tables are in Attachment A – Oneida County Data Book. and cultures to facilitate abstinence and • See also Attachment B – Oneida County Chart Book for risk reduction practices for sexual behavior additional data. and injection drug use, and setting up support systems to ensure medicines are taken as prescribed.453 The reporting of suspect or confirmed communicable diseases is mandated under the New York State Sanitary Code (10NYCRR 2.10). -

Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet
Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet Hand, foot, and mouth disease is caused by one of several types of viruses Hand, foot, and mouth disease is usually characterized by tiny blisters on the inside of the mouth and the palms of the hands, fingers, soles of the feet. It is commonly caused by coxsackievirus A16 (an enterovirus), and less often by other types of viruses. Anyone can get hand, foot, and mouth disease Young children are primarily affected, but it may be seen in adults. Most cases occur in the summer and early fall. Outbreaks may occur among groups of children especially in child care centers or nursery schools. Symptoms usually appear 3 to 5 days after exposure. Hand, foot, and mouth disease is usually spread through person-to-person contact People can spread the disease when they are shedding the virus in their feces. It is also spread by the respiratory tract from mouth or respiratory secretions (such as from saliva on hands or toys). The virus has also been found in the fluid from the skin blisters. The infection is spread most easily during the acute phase/stage of illness when people are feeling ill, but the virus can be spread for several weeks after the onset of infection. The symptoms are much like a common cold with a rash The rash appears as blisters or ulcers in the mouth, on the inner cheeks, gums, sides of the tongue, and as bumps or blisters on the hands, feet, and sometimes other parts of the skin. The skin rash may last for 7 to 10 days. -

Chlamydia-English
URGENT and PRIVATE IMPORTANT INFORMATION ABOUT YOUR HEALTH DIRECTIONS FOR SEX PARTNERS OF PERSONS WITH CHLAMYDIA PLEASE READ THIS VERY CAREFULLY Your sex partner has recently been treated for chlamydia. Chlamydia is a sexually transmitted disease (STD) that you can get from having any kind of sex (oral, vaginal, or anal) with a person who already has it. You may have been exposed. The good news is that it’s easily treated. You are being given a medicine called azithromycin (sometimes known as “Zithromax”) to treat your chlamydia. Your partner may have given you the actual medicine, or a prescription that you can take to a pharmacy. These are instructions for how to take azithromycin. The best way to take care of this infection is to see your own doctor or clinic provider right away. If you can’t get to a doctor in the next several days, you should take the azithromycin. Even if you decide to take the medicine, it is very important to see a doctor as soon as you can, to get tested for other STDs. People can have more than one STD at the same time. Azithromycin will not cure other sexually transmitted infections. Having STDs can increase your risk of getting HIV, so make sure to also get an HIV test. SYMPTOMS Some people with chlamydia have symptoms, but most do not. Symptoms may include pain in your testicles, pelvis, or lower part of your belly. You may also have pain when you urinate or when having sex. Many people with chlamydia do not know they are infected because they feel fine. -

Cutaneous Manifestations of HIV Infection Carrie L
Chapter Title Cutaneous Manifestations of HIV Infection Carrie L. Kovarik, MD Addy Kekitiinwa, MB, ChB Heidi Schwarzwald, MD, MPH Objectives Table 1. Cutaneous manifestations of HIV 1. Review the most common cutaneous Cause Manifestations manifestations of human immunodeficiency Neoplasia Kaposi sarcoma virus (HIV) infection. Lymphoma 2. Describe the methods of diagnosis and treatment Squamous cell carcinoma for each cutaneous disease. Infectious Herpes zoster Herpes simplex virus infections Superficial fungal infections Key Points Angular cheilitis 1. Cutaneous lesions are often the first Chancroid manifestation of HIV noted by patients and Cryptococcus Histoplasmosis health professionals. Human papillomavirus (verruca vulgaris, 2. Cutaneous lesions occur frequently in both adults verruca plana, condyloma) and children infected with HIV. Impetigo 3. Diagnosis of several mucocutaneous diseases Lymphogranuloma venereum in the setting of HIV will allow appropriate Molluscum contagiosum treatment and prevention of complications. Syphilis Furunculosis 4. Prompt diagnosis and treatment of cutaneous Folliculitis manifestations can prevent complications and Pyomyositis improve quality of life for HIV-infected persons. Other Pruritic papular eruption Seborrheic dermatitis Overview Drug eruption Vasculitis Many people with human immunodeficiency virus Psoriasis (HIV) infection develop cutaneous lesions. The risk of Hyperpigmentation developing cutaneous manifestations increases with Photodermatitis disease progression. As immunosuppression increases, Atopic Dermatitis patients may develop multiple skin diseases at once, Hair changes atypical-appearing skin lesions, or diseases that are refractory to standard treatment. Skin conditions that have been associated with HIV infection are listed in Clinical staging is useful in the initial assessment of a Table 1. patient, at the time the patient enters into long-term HIV care, and for monitoring a patient’s disease progression. -

Pdf/Bookshelf NBK368467.Pdf
BMJ 2019;365:l4159 doi: 10.1136/bmj.l4159 (Published 28 June 2019) Page 1 of 11 Practice BMJ: first published as 10.1136/bmj.l4159 on 28 June 2019. Downloaded from PRACTICE CLINICAL UPDATES Syphilis OPEN ACCESS Patrick O'Byrne associate professor, nurse practitioner 1 2, Paul MacPherson infectious disease specialist 3 1School of Nursing, University of Ottawa, Ottawa, Ontario K1H 8M5, Canada; 2Sexual Health Clinic, Ottawa Public Health, Ottawa, Ontario K1N 5P9; 3Division of Infectious Diseases, Ottawa Hospital General Campus, Ottawa, Ontario What you need to know Box 1: Symptoms of syphilis by stage of infection (see fig 1) • Incidence rates of syphilis have increased substantially around the Primary world, mostly affecting men who have sex with men and people infected • Symptoms appear 10-90 days (mean 21 days) after exposure with HIV http://www.bmj.com/ • Main symptom is a <2 cm chancre: • Have a high index of suspicion for syphilis in any sexually active patient – Progresses from a macule to papule to ulcer over 7 days with genital lesions or rashes – Painless, solitary, indurated, clean base (98% specific, 31% sensitive) • Primary syphilis classically presents as a single, painless, indurated genital ulcer (chancre), but this presentation is only 31% sensitive; – On glans, corona, labia, fourchette, or perineum lesions can be painful, multiple, and extra-genital – A third are extragenital in men who have sex with men and in women • Diagnosis is usually based on serology, using a combination of treponemal and non-treponemal tests. Syphilis remains sensitive to • Localised painless adenopathy benzathine penicillin G Secondary on 24 September 2021 by guest. -

2020 European Guideline on the Management of Syphilis
DOI: 10.1111/jdv.16946 JEADV GUIDELINES 2020 European guideline on the management of syphilis M. Janier,1,* M. Unemo,2 N. Dupin,3 G.S. Tiplica,4 M. Potocnik, 5 R. Patel6 1STD Clinic, Hopital^ Saint-Louis AP-HP and Hopital^ Saint-Joseph, Paris, France 2WHO Collaborating Centre for Gonorrhoea and other Sexually Transmitted Infections, Department of Laboratory Medicine, Microbiology, Orebro€ University Hospital and Orebro€ University, Orebro,€ Sweden 3Syphilis National Reference Center, Hopital^ Tarnier-Cochin, AP-HP, Paris, France 42nd Dermatological Clinic, Carol Davila University, Colentina Clinical Hospital, Bucharest, Romania 5Department of Dermatovenereology, University Medical Centre Ljubljana, Ljubljana, Slovenia 6Department of Genitourinary Medicine, the Royal South Hants Hospital, Southampton, UK *Correspondence to: M. Janier. E-mail: [email protected] Abstract The 2020 edition of the European guideline on the management of syphilis is an update of the 2014 edition. Main modifications and updates include: - The ongoing epidemics of early syphilis in Europe, particularly in men who have sex with men (MSM) - The development of dual treponemal and non-treponemal point-of-care (POC) tests - The progress in non-treponemal test (NTT) automatization - The regular episodic shortage of benzathine penicillin G (BPG) in some European countries - The exclusion of azithromycin as an alternative treatment at any stage of syphilis - The pre-exposure or immediate post-exposure prophylaxis with doxycycline in populations at high risk of acquiring syphilis. Received: 12 June 2020; Accepted: 4 September 2020 Conflicts of interest The authors have no conflicts of interest related to this guideline. Funding sources None. Introduction EEA countries and particularly among men who have sex with Syphilis is a systemic human disease due to Treponema pallidum men (MSM).3 subsp. -

WHO GUIDELINES for the Treatment of Treponema Pallidum (Syphilis)
WHO GUIDELINES FOR THE Treatment of Treponema pallidum (syphilis) WHO GUIDELINES FOR THE Treatment of Treponema pallidum (syphilis) WHO Library Cataloguing-in-Publication Data WHO guidelines for the treatment of Treponema pallidum (syphilis). Contents: Web annex D: Evidence profiles and evidence-to-decision frameworks - Web annex E: Systematic reviews for syphilis guidelines - Web annex F: Summary of conflicts of interest 1.Syphilis – drug therapy. 2.Treponema pallidum. 3.Sexually Transmitted Diseases. 4.Guideline. I.World Health Organization. ISBN 978 92 4 154980 6 (NLM classification: WC 170) © World Health Organization 2016 All rights reserved. Publications of the World Health Organization are available on the WHO website (http://www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (http://www.who.int/about/licensing/ copyright_form/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Measles Diagnostic Tool
Measles Prodrome and Clinical evolution E Fever (mild to moderate) E Cough E Coryza E Conjunctivitis E Fever spikes as high as 105ºF Koplik’s spots Koplik’s Spots E E Viral enanthem of measles Rash E Erythematous, maculopapular rash which begins on typically starting 1-2 days before the face (often at hairline and behind ears) then spreads to neck/ the rash. Appearance is similar to “grains of salt on a wet background” upper trunk and then to lower trunk and extremities. Evolution and may become less visible as the of rash 1-3 days. Palms and soles rarely involved. maculopapular rash develops. Rash INCUBATION PERIOD Fever, STARTS on face (hairline & cough/coryza/conjunctivitis behind ears), spreads to trunk, Average 8-12 days from exposure to onset (sensitivity to light) and then to thighs/ feet of prodrome symptoms 0 (average interval between exposure to onset rash 14 day [range 7-21 days]) -4 -3 -2 -1 1234 NOT INFECTIOUS higher fever (103°-104°) during this period rash fades in same sequence it appears INFECTIOUS 4 days before rash and 4 days after rash Not Measles Rubella Varicella cervical lymphadenopathy. Highly variable but (Aka German Measles) (Aka Chickenpox) Rash E often maculopapular with Clinical manifestations E Clinical manifestations E Generally mild illness with low- Mild prodrome of fever and malaise multiforme-like lesions and grade fever, malaise, and lymph- may occur one to two days before may resemble scarlet fever. adenopathy (commonly post- rash. Possible low-grade fever. Rash often associated with painful edema hands and feet. auricular and sub-occipital). -

Virus Classification Tables V2.Vd.Xlsx
DNA Virus Classification Table DNA Virus Family Genera (Subfamily) Typical Species Genetic material Capsid Envelope Disease in Humans Diseases in other Species Adenoviridae Mastadenovirus Adenoviruses 1‐47 dsDNA Icosahedral Naked Respiratory illness; conjunctivitis, Canine hepatitis, respiratory illness in horses, gastroenteritis, tonsillitis, meningitis, cystitis cattle, pigs, sheep, goats, sea lions, birds dogs, squirrel enteritis Anelloviridae Torqueviruses Alpha‐Zeta Torqueviruses (‐)ssDNA Icosahedral Naked Hepatitis, lupus, pulmonary, myopathy, Chimpanzee, pig, cow, sheep, tree shrews, multiple sclerosis; 90% of humans infected pigs, cats, sea lions and chickens worldwide Asfarviridae Asfivirus African Swine fever virus dsDNA Icosahedral Enveloped African swine fever Arthropod (tick) transmission or ingestion; hemorrhagic fever in warthogs, pigs Baculoviridae Baculovirus Alpha‐Gamma Baculoviruses dsDNA Stick shaped Occluded or Enveloped none identified Arthropods, Lepidoptera, crustaceans Circoviridae Circovirus Porcine circovirus 1 ssDNA Icosahedral Naked none identified Birds, pigs, dogs; bats; rodents; causes post‐ weaning multisystem wasting syndrome, chicken anemia Circoviridae Cyclovirus Human cyclovirus 1 ssDNA Icosahedral Naked Cyclovirus Vietnam encephalitis Encephalitis; infects multiple species including birds, mammals, insects Hepadnaviridae Orthohepadnavirus Hepatitis B virus partially ssDNA Icosahedral Enveloped Hepatitis B virus; Cirrhosis, Hepatocellular Hepatitis in ducks, squirrels, primates, herons carcinoma Herpesviridae