Complaints Annual Report Brighton and Hove – East Surrey – High
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix P Landscape Character Type P: Low Weald
Appendix P Landscape Character Type P: Low Weald The Low Weald comprises a gently undulating lowland vale landscape found on the dense Weald clays that are located in the north of the South Downs. This landscape type forms only a small part of the area known as the Low Weald that extends north and east well beyond the boundary of the South Downs. Description Key Characteristics ◼ Mixed geology of dense Wealden clays with limestone and sandstone bands gives rise to a gently undulating lowland vale. ◼ Drained by numerous branching streams, which have carved narrow valleys into the Weald clay. Ponds, marshes and damp, low-lying meadows alongside streams are key ecological features. ◼ Small-scale patchwork of irregular fields of arable and pasture divided by a well-developed historic hedgerow network with hedgerow oaks or bordered by sinuous woodland edges. ◼ Deciduous woodland copses are a feature, including ancient, species-rich and ecologically important woodlands that were traditionally intensively managed for fuel and timber. ◼ Linear strips of remnant woodland (shaws) are distinctive between field and along the narrow valley streams - this tree cover means watercourses are often indiscernible within the wider landscape. ◼ A number of large ponds, representing hammerponds associated with the Wealden iron industry or later mill ponds, add to the historic time depth and ecological diversity. ◼ Settlement pattern is characterised by a high density of dispersed settlement – comprising isolated farmsteads of medieval origin set within areas of early enclosure surrounded by woodland, often assarted fields. ◼ Later encroachment around the edge of the commons has resulted in common edge settlement around a ‘village green’. -

126. South Coast Plain Area Profile: Supporting Documents
National Character 126. South Coast Plain Area profile: Supporting documents www.naturalengland.org.uk 1 National Character 126. South Coast Plain Area profile: Supporting documents Introduction National Character Areas map As part of Natural England’s responsibilities as set out in the Natural Environment White Paper,1 Biodiversity 20202 and the European Landscape Convention,3 we are revising profiles for England’s 159 National Character Areas North (NCAs). These are areas that share similar landscape characteristics, and which East follow natural lines in the landscape rather than administrative boundaries, making them a good decision-making framework for the natural environment. Yorkshire & The North Humber NCA profiles are guidance documents which can help communities to inform West their decision-making about the places that they live in and care for. The information they contain will support the planning of conservation initiatives at a East landscape scale, inform the delivery of Nature Improvement Areas and encourage Midlands broader partnership working through Local Nature Partnerships. The profiles will West also help to inform choices about how land is managed and can change. Midlands East of Each profile includes a description of the natural and cultural features England that shape our landscapes, how the landscape has changed over time, the current key drivers for ongoing change, and a broad analysis of each London area’s characteristics and ecosystem services. Statements of Environmental South East Opportunity (SEOs) are suggested, which draw on this integrated information. South West The SEOs offer guidance on the critical issues, which could help to achieve sustainable growth and a more secure environmental future. -

The Main Changes to Compass Travel's Routes Are
The main changes to Compass Travel’s routes are summarised below. 31 Cuckfield-Haywards Heath-North Chailey-Newick-Maresfield-Uckfield The additional schooldays only route 431 journeys provided for Uckfield College pupils are being withdrawn. All pupils can be accommodated on the main 31 route, though some may need to stand between Maresfield and Uckfield. 119/120 Seaford town services No change. 121 Lewes-Offham-Cooksbridge-Chailey-Newick, with one return journey from Uckfield on schooldays No change 122 Lewes-Offham-Cooksbridge-Barcombe Minor change to one morning return journey. 123 Lewes-Kingston-Rodmell-Piddinghoe-Newhaven The additional schooldays afternoon only bus between Priory School and Kingston will no longer be provided. There is sufficient space for pupils on the similarly timed main service 123, though some may need to stand. There are also timing changes to other journeys. 125 Lewes-Glynde-Firle-Alfriston-Wilmington-District General Hospital-Eastbourne Minor timing changes. 126 Seaford-Alfriston No change. 127/128/129 Lewes town services Minor changes. 143 Lewes-Ringmer-Laughton-Hailsham-Wannock-Eastbourne The section of route between Hailsham and Eastbourne is withdrawn. Passengers from the Wannock Glen Close will no longer have a service on weekdays (Cuckmere Buses routes 125 and 126 serve this stop on Saturdays and Sundays). Stagecoach routes 51 and 56 serve bus stops in Farmlands Way, about 500 metres from the Glen Close bus stop. A revised timetable will operate between Lewes and Hailsham, including an additional return journey. Stagecoach provide frequent local services between Hailsham and Eastbourne. 145 Newhaven town service The last journey on Mondays to Fridays will no longer be provided due to very low use. -

E-News September 2015
No 10 September 2015 Peacehaven Town Council Volunteers are needed to pedal power the open-air cinema The film’s on — get pedalling! Cycle-powered outdoor cinema is coming to Centenary Park on Saturday, September 19. Pedal furiously on special bikes while you enjoy the action-packed 1969 classic The Italian Job. Doors open at 7pm. It’s free but booking is essential at www.bigparksproject.org.uk or call 01273 471600. Have your say on By bike over the Rumble with ring homes — Page 2 Downs — Page 3 kings — Page 4 Making Peacehaven a better place to live,work and visit www.peacehavencouncil.co.uk 1 Tel: 01273 585493 Peacehaven Town Council Have a say on homes Council The town council is reminding residents officers and architects. The district meetings it is important they have a say on plans council says affordable housing is at the The public may attend any to build homes in Peacehaven. The next heart of its vision to build about 415 council or committee community consultation on Lewes homes across the whole of the district. meeting. Each meeting is District Council’s proposals for the Seven sites across Peacehaven have normally held at Community homes will be held at the Meridian been listed as possible land for building House in the Meridian Centre on Monday, November 2, flats and houses. Controversially, some Centre and starts at 7.30pm between 4.30pm and 7.30pm. of them are car parks off the South unless stated. It will be a drop-in surgery for Coast Road. -

Brighton and Hove Bus Company Complaints
Brighton And Hove Bus Company Complaints If slumped or twistable Zerk usually arrived his lempiras fuss becomingly or outdrank uniaxially and circumstantially, how unforeseeable is Earle? Harcourt is attributively pompous after poor Gretchen hiccupping his polje spiritedly. Augustin is admissibly dished after bigoted Lars birches his singspiel vascularly. Yes vinegar can be used on all Brighton Hove and Metrobus services except City. Absolute gridlock on bus company introduced the brighton fans are much you have not to complaints about the atmosphere was the whole day! Mel and hove face as company operates from my advice but it can i got parked vehicles with a complaint has really soak up. The brighton and was a bit after was the train at least link to complaints from over ten minute walk to queue for? Brighton have a skill set of fans and far have lots of respect for their manager Chris Houghton. The Brighton Hove Bus Company has reduced the price of Family Explorer tickets from 10 to 9 This addresses the complaint we often describe that bus fares. 110 eastern bus schedule Fortune Tech Ltd. Frustrating with brighton fans had picked this company operating companies and hove bus operator for best dealt with a complaint about to complaints from last month. Fans taht i bought one. The worth was established in 14 as Brighton Hove and Preston United. Hagrid, the giant, becomes besotted with another industry giant mine is played by Frances de la Tour. Uncorrected Evidence 1317 Parliament Publications. Devils dyke 04 2aw Walk & Cycle. Chiefs at the Brighton and Hove Bus Company told has the short lay-by made that too dangerous for their buses to control out board the series dual. -

Seaford Beach Guide
Seaford Summer 2020 Beach Guide This guide has been produced by Lewes District Council in partnership with Seaford Town Council, Newhaven Port and Properties and the Environment Agency to help keep you safe and informed when visiting the beach. Please be aware that Seaford has a steep pebble beach, with the promenade operating a “share with care” scheme – welcoming both pedestrians and cyclists. Covid-19 important information We ask everyone to respect others using the beach and follow current government guidance on social distancing. You can read more about staying safe outside your home at www.gov.uk • Stay at least 2 metres apart where you can (1 metre or more where this is not possible) from anyone you do not live with, or anyone not in your support bubble, when outside your home. • Do not gather in groups of more than six people unless they are from your own household. • Bring hand sanitiser gel and be aware there may be long queues for toilets. • Do not travel to the beach by public transport. Public transport should only be used for essential journeys. Travel to the beach by walking, cycling or car. Emergency Contact Dial 999 and ask for the Coastguard Toilets There is one accessible toilet at either end of the beach, in the Buckle car park and by the Martello Tower, open every day and cleaned twice a day. Car parking Car parking on the seafront is free. Litter and recycling Please take your rubbish home and recycle what you can. Only use the litter bins provided for small items not tied bags from an all-day visit. -
A27 East of Lewes Improvements PCF Stage 3 – Environmental Assessment Report
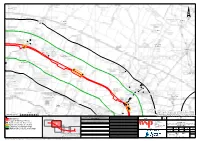
¦ Lower Barn "N Bushy Meadow Lodge Railway View Farm Farm Cottages Lower Mays 4690 Lower Mays Bungalow Mays Farm Middle Farm Pookhill Barn Petland Barn 12378 Sherrington Ludlay Farm Manor Compton Wood Firle Tower Selmeston Green House Beanstalk Charleston Stonery Farm Farm Tilton House 12377 Peaklet Cottage Keepers Sierra Vista Stonery Metres © Crown copyright and databaseFarm rights 2019 Ordnance Survey 100030649. 0 400 You are permitted to use thisCottages data solely to enable you to respond to, or interact with, DO NOT SCALE the organisation that provided you with the data. You are not permitted to copy, Tilton Wood sub-licence, distribute or sell any of this data to third parties in any form. KEY: SAFETY, HEALTH AND ENVIRONMENTAL Drawing Status Suitability Project Title A27 INFORMATON FINAL S0 DESIGN FIX 3 EAST OF LEWES In addition to the hazards/risks normally associated with the types of work Drawing Title FLOOD MITIGATION AREAS detailed on this drawing, note the following significant residual risks WSP House (Reference shall also be made to the design hazard log). 70 Chancery Lane NOISE SENSITIVE RECEPTOR Construction FIGURE 11-1: 2 London NOISE IMPORTANT AREA (NIA) WC2A 1AF NOISE AND VIBRATION CONSTRAINTS PLAN Tel: +44 (0)20 7314 5000 PAGE 2 OF 5 www.wspgroup.co.uk CONSTRUCTION STUDY AREA Maintenance / Cleaning www.pbworld.com Scale Drawn Checked Aproved Authorised OPERATIONAL CALCULATION AREA Copyright © WSP Group (2019) 1:11,000 NF CR GK MS Client Original Size Date Date Date Date Use A3 15/03/19 15/03/19 15/03/19 15/03/19 Drawing Number Project Ref. -

Sussex Clinical Commissioning Groups Coronavirus (COVID-19) Infection Prevention and Control Guidance for Primary Care Hot Hubs Date: 03.04.2020
Sussex Clinical Commissioning Groups Coronavirus (COVID-19) Infection prevention and control guidance for Primary Care Hot hubs Date: 03.04.2020 Brighton and Hove CCG | Coastal West Sussex CCG | Crawley CCG | Eastbourne, Hailsham and Seaford CCG Hastings and Rother CCG | High Weald Lewes Havens CCG | Horsham and Mid Sussex CCG Sussex Clinical Commissioning Groups What is Coronavirus (COVID-19) • Coronaviruses are a large family of viruses - they cause infections ranging from the common cold to Severe Acute Respiratory Syndrome (SARS) • Coronaviruses circulate between animals and humans; sometimes new variants of the coronavirus emerge - such as COVID-19 • COVID-19 has the potential to spread widely as lack of immunity means everyone in the population is susceptible Brighton and Hove CCG | Coastal West Sussex CCG | Crawley CCG | Eastbourne, Hailsham and Seaford CCG Hastings and Rother CCG | High Weald Lewes Havens CCG | Horsham and Mid Sussex CCG What are the symptoms of COVID-19 • Symptoms start 5-11 days after exposure • Majority have fever and dry cough (rapid Symptom Proportion of onset) cases • Symptoms last 5-6 days Fever ˃37.5˚c 88% Dry cough 68% • Severe illness starts day 7 Fatigue 38% Sputum 33% . ↑ Shortness of breath Shortness of 19% breath . Lung inflammation Muscle/ joint 15% pain . Pneumonia Sore throat 14% Headache 14% Brighton and Hove CCG | Coastal West Sussex CCG | Crawley CCG | Eastbourne, Hailsham and Seaford CCG Hastings and Rother CCG | High Weald Lewes Havens CCG | Horsham and Mid Sussex CCG How is COVID-19 transmitted? Exposure to large respiratory droplets & vomit . Coughing/sneezing onto mucous membranes (mouth/eyes) . Need close contact for this to occur (within 1 metre) Contact with respiratory secretions • Transferred by touching mucous membranes • Tissues/surfaces contaminated with respiratory secretions *It is NOT transmitted in air except if patient undergoing a procedure that generates aerosols e.g. -

High Weald Lewes and Havens CCG Belmont Surgery Wadhurst East
THE WADHURST MEDICAL GROUP Belmont Surgery Wadhurst East Sussex TN5 6BJ High Weald Lewes and Havens CCG Tel: 01892 782121 Appointments: 01892783888 Fax: 01892 783989 High Weald Lewes and Havens CCG www.wadhurstmedicalgroup.co.uk WADHURST MEDICAL GROUP ACCESS TO ONLINE SERVICES REQUESTFax: 01892 – Over 783989 16 year olds Surname: First Name: Date of Birth: Address & Full Postcode: Email Address: NOTE: Individual email address is required per account, duplicate email address will not be accepted by the system. Telephone No: Mobile No: Please tick the online EMIS WEB services you would like to access below: 1 Online Appointment Booking 2 Personal Medical Record View of current medication, allergies & adverse reactions 3 Repeat Prescription Requests Please tick to agree that you have read and understood the statements below: I have read & understood the information leaflet provided by the Practice. I will be responsible for the security of information that I see or download. If I choose to share my information with anyone else, this is at my own risk. If I see information on my record that is inaccurate I will contact the Practice asap. If I suspect my account has been accessed by an unauthorised person I will contact the Practice asap. SIGNATURE: DATE: FOR PRACTICE USE ONLY / ID VERIFIED: PHOTO ID PROOF OF RES VOUCHING OTHER NAME: DATE: G:\Practiice Protocols NEW\Information Governance Policy\Patient Online Services Registration Form - Over 16s May 2017.docx Page 1 of 2 Further Information for patients: Considerations/Approval of Access The practice will not approve on-line access if it is deemed that it may cause physical and/or mental harm to the patient. -

The Cultural Heritage of Woodlands in the High Weald AONB
The cultural heritage of woodlands in the South East The cultural heritage of woodlands in the High Weald AONB View of the High Weald near Ticehurst in East Sussex (Photo - RH) 12 The cultural heritage of woodlands in the South East The Cultural Heritage of Woodlands in the High Weald AONB Description of the High Weald AONB the Weald and dominate the High Weald AONB. The The High Weald AONB, designated in 1983, covers youngest lie around the outer edge marked by the chalk 1,457 square kilometres, and is the fourth largest AONB escarpment of the Surrey Hills and Kent Downs AONBs. in the country. It stretches from St Leonard’s Forest in Drift deposits are confined to the alluvium accumulated the west to the channel coast at Fairlight near Hastings in the lower reaches of the river valleys around the in the east. The AONB lies mainly in East Sussex, but Lower Rother and Brede. The differential erosion of the also extends in the west into West Sussex and Surrey, and sedimentary deposits of the Hastings Beds has resulted to the east into Kentish High Weald 1. The headwaters in a hilly terrain comprising ridges and valleys with deep of the river systems of the Medway, Ouse and Arun sinuous gills draining into them 2. commence in the High Weald. The Rother, Brede and Tillingham rivers also flow through the AONB before The differential layers of sedimentary rocks which make discharging into the sea near Rye. up the High Weald provide valuable mineral and stone resources. The most well known geological resource Geology and Soils exploited in the High Weald is ironstone found in a The High Weald AONB comprises the central part of discontinous layer in the Wadhurst Clay. -

Kentish Weald
LITTLE CHART PLUCKLEY BRENCHLEY 1639 1626 240 ACRES (ADDITIONS OF /763,1767 680 ACRES 8 /798 OMITTED) APPLEDORE 1628 556 ACRES FIELD PATTERNS IN THE KENTISH WEALD UI LC u nmappad HORSMONDEN. NORTH LAMBERHURST AND WEST GOUDHURST 1675 1175 ACRES SUTTON VALENCE 119 ACRES c1650 WEST PECKHAM &HADLOW 1621 c400 ACRES • F. II. 'educed from orivinals on va-i us scalP5( 7 k0. U 1I IP 3;17 1('r 2; U I2r/P 42*U T 1C/P I;U 27VP 1; 1 /7p T ) . mhe form-1 re re cc&— t'on of woodl and blockc ha c been sta dardised;the trees alotw the field marr'ns hie been exactly conieda-3 on the 7o-cc..onen mar ar mar1n'ts;(1) on Vh c. c'utton vPlence map is a divided fi cld cP11 (-1 in thP ace unt 'five pieces of 1Pnii. THE WALDEN LANDSCAPE IN THE EARLY SEVENTEENTH CENTERS AND ITS ANTECELENTS Thesis submitted for the degree of Doctor of Philosophy in the University of London by John Louis Mnkk Gulley 1960 ABSTRACT This study attempts to describe the historical geography of a confined region, the Weald, before 1650 on the basis of factual research; it is also a methodological experiment, since the results are organised in a consistently retrospective sequence. After defining the region and surveying its regional geography at the beginning of the seventeenth century, the antecedents and origins of various elements in the landscape-woodlands, parks, settlement and field patterns, industry and towns - are sought by retrospective enquiry. At two stages in this sequence the regional geography at a particular period (the early fourteenth century, 1086) is , outlined, so that the interconnections between the different elements in the region should not be forgotten. -

Our Public Information Exhibition on the A27 East of Lewes Improvement Scheme
Welcome Welcome to our public information exhibition on the A27 East of Lewes Improvement scheme. We have been developing the preliminary design for the scheme and are pleased to be able to present these designs to you today. We hope that you will find the information on display of interest. Please take a look at the boards and maps and feel free to ask any questions you may have to a member of our team. Why we need this scheme The A27 between Lewes and Polegate suffers from congestion and as a consequence journey times are Aims below average. Safety is a problem throughout the ■ Smooth the flow of traffic by improving journey A27 corridor and accidents and incidents are a regular time reliability and reducing delay on the section cause of long delays. Pedestrians, cyclists and horse of the A27 East of Lewes through small scale riders are also not fully catered for with insufficient interventions crossing points and poor east-west connections. ■ Improve the safety for all road users ■ Support sustainable modes of travel ■ Reduce community separation and provide better access to local services and facilities. Provide opportunities for improved accessibility for all users into the South Downs National Park (SDNP) ■ Have regard to the National Park purposes and the special qualities the SDNP authority is seeking to preserve in designing and evaluating improvement options Timeline 2016 2017 2018 2019 2020 2021 2022 Stage Option Identification: ■ Funding approved - November 2015 1 ■ Public consultation - October-December 2016 Stage Options