Development of Hyperprolactinemia Induced by the Addition of Bupropion to Venlafaxine XR Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WELLBUTRIN SR Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION psychosis, hallucinations, paranoia, delusions, homicidal ideation, These highlights do not include all the information needed to use aggression, hostility, agitation, anxiety, and panic, as well as suicidal WELLBUTRIN SR safely and effectively. See full prescribing ideation, suicide attempt, and completed suicide. Observe patients information for WELLBUTRIN SR. attempting to quit smoking with bupropion for the occurrence of such symptoms and instruct them to discontinue bupropion and contact a WELLBUTRIN SR (bupropion hydrochloride) sustained-release tablets, healthcare provider if they experience such adverse events. (5.2) for oral use • Initial U.S. Approval: 1985 Seizure risk: The risk is dose-related. Can minimize risk by gradually increasing the dose and limiting daily dose to 400 mg. Discontinue if WARNING: SUICIDAL THOUGHTS AND BEHAVIORS seizure occurs. (4, 5.3, 7.3) See full prescribing information for complete boxed warning. • Hypertension: WELLBUTRIN SR can increase blood pressure. Monitor blood pressure before initiating treatment and periodically during • Increased risk of suicidal thinking and behavior in children, treatment. (5.4) adolescents and young adults taking antidepressants. (5.1) • Activation of mania/hypomania: Screen patients for bipolar disorder and • Monitor for worsening and emergence of suicidal thoughts and monitor for these symptoms. (5.5) behaviors. (5.1) • Psychosis and other neuropsychiatric reactions: Instruct patients to contact a healthcare professional if such reactions occur. (5.6) --------------------------- INDICATIONS AND USAGE ---------------------------- • Angle-closure glaucoma: Angle-closure glaucoma has occurred in WELLBUTRIN SR is an aminoketone antidepressant, indicated for the patients with untreated anatomically narrow angles treated with treatment of major depressive disorder (MDD). (1) antidepressants. -

Concomitant Drugs Associated with Increased Mortality for MDMA Users Reported in a Drug Safety Surveillance Database Isaac V
www.nature.com/scientificreports OPEN Concomitant drugs associated with increased mortality for MDMA users reported in a drug safety surveillance database Isaac V. Cohen1, Tigran Makunts2,3, Ruben Abagyan2* & Kelan Thomas4 3,4-Methylenedioxymethamphetamine (MDMA) is currently being evaluated by the Food and Drug Administration (FDA) for the treatment of post-traumatic stress disorder (PTSD). If MDMA is FDA-approved it will be important to understand what medications may pose a risk of drug– drug interactions. The goal of this study was to evaluate the risks due to MDMA ingestion alone or in combination with other common medications and drugs of abuse using the FDA drug safety surveillance data. To date, nearly one thousand reports of MDMA use have been reported to the FDA. The majority of these reports include covariates such as co-ingested substances and demographic parameters. Univariate and multivariate logistic regression was employed to uncover the contributing factors to the reported risk of death among MDMA users. Several drug classes (MDMA metabolites or analogs, anesthetics, muscle relaxants, amphetamines and stimulants, benzodiazepines, ethanol, opioids), four antidepressants (bupropion, sertraline, venlafaxine and citalopram) and olanzapine demonstrated increased odds ratios for the reported risk of death. Future drug–drug interaction clinical trials should evaluate if any of the other drug–drug interactions described in our results actually pose a risk of morbidity or mortality in controlled medical settings. 3,4-Methylenedioxymethamphetamine (MDMA) is currently being evaluated by the Food and Drug Adminis- tration (FDA) for the treatment of posttraumatic stress disorder (PTSD). During the past two decades, “ecstasy” was illegally distributed and is purported to contain MDMA, but because the market is unregulated this “ecstasy” may actually contain adulterants or no MDMA at all1. -

Canadian Stroke Best Practice Recommendations
CANADIAN STROKE BEST PRACTICE RECOMMENDATIONS MOOD, COGNITION AND FATIGUE FOLLOWING STROKE Table 1C: Summary Table for Selected Pharmacotherapy for Post-Stroke Depression Update 2019 Lanctôt KL, Swartz RH (Writing Group Chairs) on Behalf of the Canadian Stroke Best Practice Recommendations Mood, Cognition and Fatigue following Stroke Writing Group and the Canadian Stroke Best Practice and Quality Advisory Committee, in collaboration with the Canadian Stroke Consortium © 2019 Heart & Stroke Heart and Stroke Foundation Mood, Cognition and Fatigue following Stroke Canadian Stroke Best Practice Recommendations Table 1C Table 1C: Summary Table for Selected Pharmacotherapy for Post-Stroke Depression This table provides a summary of the pharmacotherapeutic properties, side effects, drug interactions and other important information on selected classes of medications available for use in Canada and more commonly recommended for post-stroke depression. This table should be used as a reference guide by health care professionals when selecting an appropriate agent for individual patients. Patient compliance, patient preference and/or past experience, side effects, and drug interactions should all be taken into consideration during decision-making, in addition to other information provided in this table and available elsewhere regarding these medications. Selective Serotonin Reuptake Inhibitors (SSRI) Serotonin–norepinephrine reuptake Other inhibitors (SNRI) Medication *citalopram – Celexa *duloxetine – Cymbalta methylphenidate – Ritalin (amphetamine) -

Methylphenidate Hydrochloride
Application for Inclusion to the 22nd Expert Committee on the Selection and Use of Essential Medicines: METHYLPHENIDATE HYDROCHLORIDE December 7, 2018 Submitted by: Patricia Moscibrodzki, M.P.H., and Craig L. Katz, M.D. The Icahn School of Medicine at Mount Sinai Graduate Program in Public Health New York NY, United States Contact: [email protected] TABLE OF CONTENTS Page 3 Summary Statement Page 4 Focal Point Person in WHO Page 5 Name of Organizations Consulted Page 6 International Nonproprietary Name Page 7 Formulations Proposed for Inclusion Page 8 International Availability Page 10 Listing Requested Page 11 Public Health Relevance Page 13 Treatment Details Page 19 Comparative Effectiveness Page 29 Comparative Safety Page 41 Comparative Cost and Cost-Effectiveness Page 45 Regulatory Status Page 48 Pharmacoepial Standards Page 49 Text for the WHO Model Formulary Page 52 References Page 61 Appendix – Letters of Support 2 1. Summary Statement of the Proposal for Inclusion of Methylphenidate Methylphenidate (MPH), a central nervous system (CNS) stimulant, of the phenethylamine class, is proposed for inclusion in the WHO Model List of Essential Medications (EML) & the Model List of Essential Medications for Children (EMLc) for treatment of Attention-Deficit/Hyperactivity Disorder (ADHD) under ICD-11, 6C9Z mental, behavioral or neurodevelopmental disorder, disruptive behavior or dissocial disorders. To date, the list of essential medications does not include stimulants, which play a critical role in the treatment of psychotic disorders. Methylphenidate is proposed for inclusion on the complimentary list for both children and adults. This application provides a systematic review of the use, efficacy, safety, availability, and cost-effectiveness of methylphenidate compared with other stimulant (first-line) and non-stimulant (second-line) medications. -

Preferred Drug List Illinois Medicaid 10/1/2019: Revised 11/06/2019 for Drugs Not Found on This List, Go to the Drug Search Engine At
Preferred Drug List Illinois Medicaid 10/1/2019: Revised 11/06/2019 For drugs not found on this list, go to the drug search engine at: www.ilpriorauth.com *Exceptions as noted above* ▪ADHD Agents: Prior authorization required for participants under 6 years of age and participants 19 years of age and older ▪Spiriva AER 1.25mcg: Prior authorization NOT required for participants ages 6-17 years ▪Budesonide: Prior authorization NOT required for participants age 7 years and under ▪Anticonvulsants: Prior authorization NOT required for non-preferred epilepsy agents for those participants with a diagnosis of epilepsy or seizure disorder in Department records ▪Antipsychotics: Prior authorization required for participants under 8 years of age and long- term care residents 1 of 27 Preferred Drug List Illinois Medicaid 10/1/2019: Revised 11/06/2019 For drugs not found on this list, go to the drug search engine at: www.ilpriorauth.com Category Preferred Preferred, Requires PA Non-Preferred ADHD Agent - Amphetamine Mixtures* AMPHETAMINE/DEXTROAMPHETAMINE ADDERALL ADDERALL XR MYDAYIS ADHD Agent - Amphetamines* VYVANSE ADZENYS ER ADZENYS XR-ODT AMPHETAMINE SULFATE DESOXYN DEXEDRINE DEXTROAMPHETAMINE SULFATE DEXTROAMPHETAMINE SULFATE ER DYANAVEL XR EVEKEO EVEKEO ODT METHAMPHETAMINE HCL PROCENTRA ZENZEDI ADHD Agent - Selective Alpha Adrenergic Agonists CLONIDINE HCL ER INTUNIV CLONIDINE HYDROCHLORIDE ER GUANFACINE ER ADHD Agent - Selective Norepinephrine Reuptake Inhibitor* ATOMOXETINE ATOMOXETINE HYDROCHLORIDE STRATTERA 2 of 27 Preferred Drug List Illinois -

Levomilnacipran (Fetzima®) Indication
Levomilnacipran (Fetzima®) Indication: Indicated for the treatment of major depressive disorder (MDD), FDA approved July 2013. Mechanism of action Levomilnacipran, the more active enantiomer of racemic milnacipran, is a selective SNRI with greater potency for inhibition of norepinephrine relative to serotonin reuptake Compared with duloxetine or venlafaxine, levomilnacipran has over 10-fold higher selectivity for norepinephrine relative to serotonin reuptake inhibition The exact mechanism of the antidepressant action of levomilnacipran is unknown Dosage and administration Initial: 20 mg once daily for 2 days and then increased to 40 mg once daily. The dosage can be increased by increments of 40 mg at intervals of two or more days Maintenance: 40-120 mg once daily with or without food. Fetzima should be swallowed whole (capsule should not be opened or crushed) Levomilnacipran and its metabolites are eliminated primarily by renal excretion o Renal impairment Dosing: Clcr 30-59 mL/minute: 80 mg once daily Clcr 15-29 mL/minute: 40 mg once daily End-stage renal disease (ESRD): Not recommended Discontinuing treatment: Gradually taper dose, if intolerable withdrawal symptoms occur, consider resuming the previous dose and/or decrease dose at a more gradual rate How supplied: Capsule ER 24 Hour Fetzima Titration: 20 & 40 mg (28 ea) Fetzima: 20 mg, 40 mg, 80 mg, 120 mg Warnings and Precautions Elevated Blood Pressure and Heart Rate: measure heart rate and blood pressure prior to initiating treatment and periodically throughout treatment Narrow-angle glaucoma: may cause mydriasis. Use caution in patients with controlled narrow- angle glaucoma Urinary hesitancy or retention: advise patient to report symptoms of urinary difficulty Discontinuation Syndrome Seizure disorders: Use caution with a previous seizure disorder (not systematically evaluated) Risk of Serotonin syndrome when taken alone or co-administered with other serotonergic agents (including triptans, tricyclics, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. -

Levomilnacipran for the Treatment of Major Depressive Disorder
Out of the Pipeline Levomilnacipran for the treatment of major depressive disorder Matthew Macaluso, DO, Hala Kazanchi, MD, and Vikram Malhotra, MD An SNRI with n July 2013, the FDA approved levomil- Table 1 once-daily dosing, nacipran for the treatment of major de- Levomilnacipran: Fast facts levomilnacipran pressive disorder (MDD) in adults.1 It is I Brand name: Fetzima decreased core available in a once-daily, extended-release formulation (Table 1).1 The drug is the fifth Class: Serotonin-norepinephrine reuptake symptoms of inhibitor serotonin-norepinephrine reuptake inhibi- MDD and was well Indication: Treatment of major depressive tor (SNRI) to be sold in the United States disorder in adults tolerated in clinical and the fourth to receive FDA approval for FDA approval date: July 26, 2013 trials treating MDD. Availability date: Fourth quarter of 2013 Levomilnacipran is believed to be the Manufacturer: Forest Pharmaceuticals more active enantiomer of milnacipran, Dosage forms: Extended–release capsules in which has been available in Europe for 20 mg, 40 mg, 80 mg, and 120 mg strengths years and was approved by the FDA in Recommended dosage: 40 mg to 120 mg 2009 for treating fibromyalgia. Efficacy of capsule once daily with or without food levomilnacipran for treating patients with Source: Reference 1 MDD was established in three 8-week ran- domized controlled trials (RCTs).1 cial and occupational functioning in addi- Clinical implications tion to improvement in the core symptoms Levomilnacipran is indicated for treating of depression.5 -

Sibutramine Hydrochloride Monohydrate) Capsule CS-IV
MERIDIA - sibutramine hydrochloride capsule ---------- MERIDIA® (sibutramine hydrochloride monohydrate) Capsule CS-IV DESCRIPTION MERIDIA® (sibutramine hydrochloride monohydrate) is an orally administered agent for the treatment of obesity. Chemically, the active ingredient is a racemic mixture of the (+) and (-) enantiomers of cyclobutanemethanamine, 1-(4-chlorophenyl)-N,N-dimethyl-α-(2-methylpropyl)-, hydrochloride, monohydrate, and has an empirical formula of C17H29Cl2NO. Its molecular weight is 334.33. The structural formula is shown below: Sibutramine hydrochloride monohydrate is a white to cream crystalline powder with a solubility of 2.9 mg/mL in pH 5.2 water. Its octanol: water partition coefficient is 30.9 at pH 5.0. Each MERIDIA capsule contains 5 mg, 10 mg, and 15 mg of sibutramine hydrochloride monohydrate. It also contains as inactive ingredients: lactose monohydrate, NF; microcrystalline cellulose, NF; colloidal silicon dioxide, NF; and magnesium stearate, NF in a hard-gelatin capsule [which contains titanium dioxide, USP; gelatin; FD&C Blue No. 2 (5- and 10-mg capsules only); D&C Yellow No. 10 (5- and 15-mg capsules only), and other inactive ingredients]. CLINICAL PHARMACOLOGY Mode of Action Sibutramine produces its therapeutic effects by norepinephrine, serotonin and dopamine reuptake inhibition. Sibutramine and its major pharmacologically active metabolites (M1 and M2) do not act via release of monoamines. Pharmacodynamics Sibutramine exerts its pharmacological actions predominantly via its secondary (M1) and primary (M2) amine metabolites. The parent compound, sibutramine, is a potent inhibitor of serotonin (5- hydroxytryptamine, 5-HT) and norepinephrine reuptake in vivo, but not in vitro. However, metabolites M1 and M2 inhibit the reuptake of these neurotransmitters both in vitro and in vivo. -

MEDICATION GUIDE WELLBUTRIN® (WELL Byu-Trin) (Bupropion Hydrochloride) Tablets
NDA 018644/S-041 NDA 020358/S-048 Page 6 MEDICATION GUIDE WELLBUTRIN® (WELL byu-trin) (bupropion hydrochloride) Tablets Read this Medication Guide carefully before you start using WELLBUTRIN and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment. If you have any questions about WELLBUTRIN, ask your doctor or pharmacist. IMPORTANT: Be sure to read the three sections of this Medication Guide. The first section is about the risk of suicidal thoughts and actions with antidepressant medicines; the second section is about the risk of changes in thinking and behavior, depression and suicidal thoughts or actions with medicines used to quit smoking; and the third section is entitled “What Other Important Information Should I Know About WELLBUTRIN?” Antidepressant Medicines, Depression and Other Serious Mental Illnesses, and Suicidal Thoughts or Actions This section of the Medication Guide is only about the risk of suicidal thoughts and actions with antidepressant medicines. Talk to your, or your family member’s, healthcare provider about: • all risks and benefits of treatment with antidepressant medicines • all treatment choices for depression or other serious mental illness What is the most important information I should know about antidepressant medicines, depression and other serious mental illnesses, and suicidal thoughts or actions? 1. Antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults within the first few months of treatment. 2. Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. -
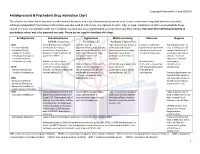
Antidepressant & Psychedelic Drug Interaction Chart
Copyright Psychedelic School 8/2020 Antidepressant & Psychedelic Drug Interaction Chart This chart is not intended to be used to make medical decisions and is for informational purposes only. It was constructed using data whenever possible, although extrapolation from known information was also used to inform risk. Any decision to start, stop, or taper medication and/or use psychedelic drugs should be made in conjunction with your healthcare provider(s). It is recommended to not perform any illicit activity. This chart the intellectual property of psychedelic school and is for personal use only. Please do not copy or distribute this chart. Antidepressant Phenethylamines Tryptamines MAOI-containing Ketamine Ibogaine -MDMA, mescaline -Psilocybin, LSD -Ayahuasca, Syrian Rue SSRIs Taper & discontinue at least 2 Consider taper & Taper & discontinue at least 2 Has been studied and Taper & discontinue at · Paroxetine (Paxil) weeks prior (all except discontinuation at least 2 weeks weeks prior (all except found effective both with least 2 weeks prior (all · Sertraline (Zoloft) fluoxetine) or 6 weeks prior prior (all except fluoxetine) or 6 fluoxetine) or 6 weeks prior and without concurrent except fluoxetine) or 6 · Citalopram (Celexa) (fluoxetine only) due to loss of weeks prior (fluoxetine only) (fluoxetine only) due to use of antidepressants weeks prior (fluoxetine · Escitalopram (Lexapro) psychedelic effect due to potential loss of potential risk of serotonin only) due to risk of · Fluxoetine (Prozac) psychedelic effect syndrome additive QTc interval · Fluvoxamine (Luvox) MDMA is unable to cause Recommended prolongation, release of serotonin when the Chronic antidepressant use may Life threatening toxicities can to be used in conjunction arrhythmias, or SPARI serotonin reuptake pump is result in down-regulation of occur with these with oral antidepressants cardiotoxicity · Vibryyd (Vilazodone) blocked. -

Adverse Effects of First-Line Pharmacologic Treatments of Major Depression in Older Adults
Draft Comparative Effectiveness Review Number xx Adverse Effects of First-line Pharmacologic Treatments of Major Depression in Older Adults Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov This information is distributed solely for the purposes of predissemination peer review. It has not been formally disseminated by the Agency for Healthcare Research and Quality. The findings are subject to change based on the literature identified in the interim and peer-review/public comments and should not be referenced as definitive. It does not represent and should not be construed to represent an Agency for Healthcare Research and Quality or Department of Health and Human Services (AHRQ) determination or policy. Contract No. 290-2015-00012I Prepared by: Will be included in the final report Investigators: Will be included in the final report AHRQ Publication No. xx-EHCxxx <Month, Year> ii Purpose of the Review To assess adverse events of first-line antidepressants in the treatment of major depressive disorder in adults 65 years or older. Key Messages • Acute treatment (<12 weeks) with o Serotonin norepinephrine reuptake inhibitors (SNRIs) (duloxetine, venlafaxine), but not selective serotonin reuptake inhibitors (SSRIs) (escitalopram, fluoxetine) led to a greater number of adverse events compared with placebo. o SSRIs (citalopram, escitalopram and fluoxetine) and SNRIs (duloxetine and venlafaxine) led to a greater number of patients withdrawing from studies due to adverse events compared with placebo o Details of the contributing adverse events in RCTs were rarely reported to more clearly characterize what adverse events to expect. -

Phd Thesis Project: Pharmacological and Toxicological Investigations of New Psychoactive Substances, Supervised by Prof
PHARMACOLOGICAL AND TOXICOLOGICAL INVESTIGATIONS OF NEW PSYCHOACTIVE SUBSTANCES Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Dino Lüthi aus Rüderswil, Bern Basel, 2018 Originaldokument gespeichert auf dem Dokumentenserver der Universität Basel edoc.unibas.ch Dieses Werk ist lizenziert unter einer Creative Commons Namensnennung-Nicht kommerziell 4.0 International Lizenz (https://creativecommons.org/licenses/by-nc-sa/4.0/deed.de). Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Stephan Krähenbühl, Prof. Matthias E. Liechti und Prof. Anne Eckert. Basel, den 26.06.2018 Prof. Martin Spiess Dekan der Philosophisch- Naturwissenschaftlichen Fakultät PHARMACOLOGICAL AND TOXICOLOGICAL INVESTIGATIONS OF NEW PSYCHOACTIVE SUBSTANCES “An adult must make his own decision as to whether or not he should expose himself to a specific drug, be it available by prescription or proscribed by law, by measuring the potential good and bad with his own personal yardstick.” ― Alexander Shulgin, Pihkal: A Chemical Love Story. PREFACE This thesis is split into a pharmacology part and a toxicology part. The pharmacology part consists of investigations on the monoamine transporter and receptor interactions of traditional and newly emerged drugs, mainly stimulants and psychedelics; the toxicology part consists of investigations on mechanisms of hepatocellular toxicity of synthetic cathinones. All research described in this thesis has been published in peer-reviewed journals, and was performed between October 2014 and June 2018 in the Division of Clinical Pharmacology and Toxicology at the Department of Biomedicine of the University Hospital Basel and University of Basel, and partly at the pRED Roche Innovation Center Basel at F.