October, 2012 Consolidated Local Service Plan (CLSP) Template
Component: 020 LMHA: Texas Panhandle Centers
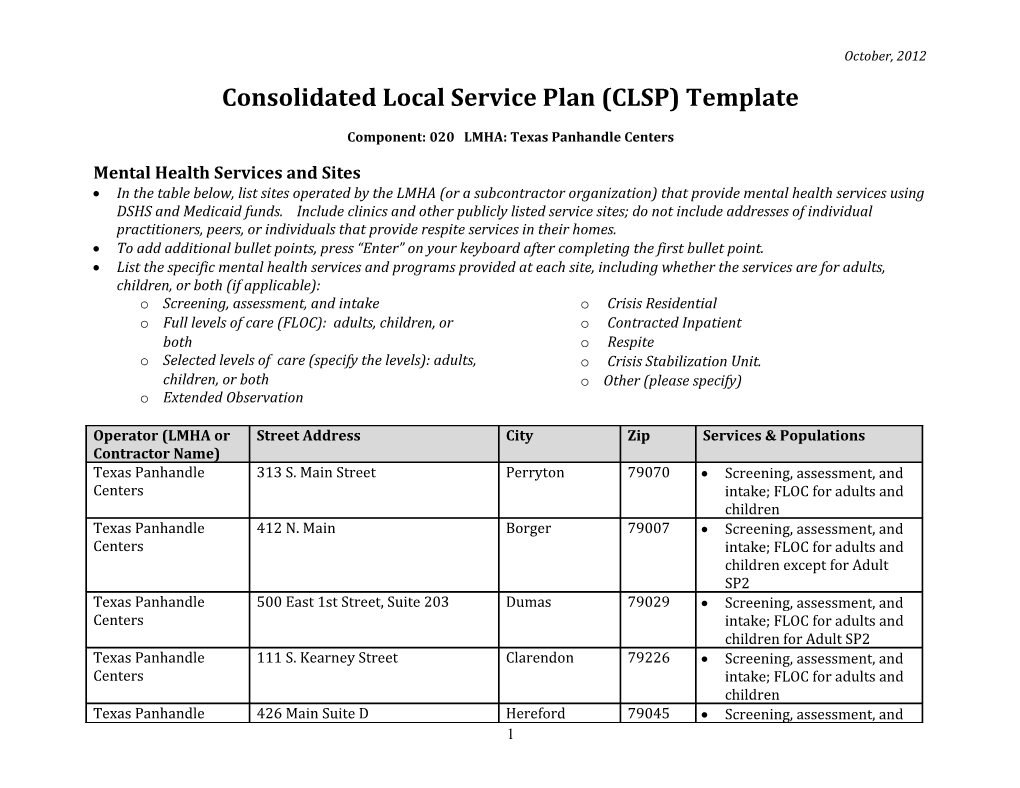
Mental Health Services and Sites In the table below, list sites operated by the LMHA (or a subcontractor organization) that provide mental health services using DSHS and Medicaid funds. Include clinics and other publicly listed service sites; do not include addresses of individual practitioners, peers, or individuals that provide respite services in their homes. To add additional bullet points, press “Enter” on your keyboard after completing the first bullet point. List the specific mental health services and programs provided at each site, including whether the services are for adults, children, or both (if applicable): o Screening, assessment, and intake o Crisis Residential o Full levels of care (FLOC): adults, children, or o Contracted Inpatient both o Respite o Selected levels of care (specify the levels): adults, o Crisis Stabilization Unit. children, or both o Other (please specify) o Extended Observation
Operator (LMHA or Street Address City Zip Services & Populations Contractor Name) Texas Panhandle 313 S. Main Street Perryton 79070 Screening, assessment, and Centers intake; FLOC for adults and children Texas Panhandle 412 N. Main Borger 79007 Screening, assessment, and Centers intake; FLOC for adults and children except for Adult SP2 Texas Panhandle 500 East 1st Street, Suite 203 Dumas 79029 Screening, assessment, and Centers intake; FLOC for adults and children for Adult SP2 Texas Panhandle 111 S. Kearney Street Clarendon 79226 Screening, assessment, and Centers intake; FLOC for adults and children Texas Panhandle 426 Main Suite D Hereford 79045 Screening, assessment, and 1 October, 2012
Operator (LMHA or Street Address City Zip Services & Populations Contractor Name) Centers intake; FLOC for adults and children Texas Panhandle 615 Buckler Ave Pampa 79065 Screening, assessment, and Centers intake; FLOC for adults and children Texas Panhandle 1501 S Polk Amarillo 79101 Screening, assessment, and Centers intake; FLOC for adults Texas Panhandle 1500 S Taylor Amarillo 79101 Screening, assessment, and Centers intake; FLOC for children Texas Panhandle 200 S Tyler Amarillo 79101 Screening, assessment, and Centers intake for the Homeless; FLOC for adults; referral services for children Texas Panhandle 1703 S Avondale Amarillo 79106 Mobile Crisis Outreach Centers Team-Crisis Services for Adults and Children, Screening, assessment, and intake Texas Panhandle 900 S Polk Suite 900 Amarillo 79101 Adult TCOOMMI Services, Centers Screening, assessment, and intake Texas Panhandle 9300 S Georgia Amarillo 79118 Juvenile TCOOMMI Services Centers For Randall County, Screening, assessment, and intake
2 October, 2012
Community Participation LMHAs have been engaged in multiple planning activities over the past year, including those relating to jail diversion efforts, plans to reduce utilization of state hospitals, and implementation of the Medicaid 1115 Transformation Waiver. The results of these planning efforts are summarized in this Local Service Plan.
Identify community stakeholders who participated in your local service planning activities over the past year.
Stakeholder Type Stakeholder Type
Consumers Family members Advocates (children and adult) Concerned citizens/others Local psychiatric hospital staff State hospital staff Mental health service providers Substance abuse treatment providers Prevention services providers Outreach, Screening, and Referral (OSAR) County officials City officials FQHCs/other primary care providers Local health departments Hospital emergency room personnel Emergency responders Faith-based organizations Community health & human service providers Probation department representatives Parole department representatives Court representatives from each county (judges, DAs, Law enforcement public defenders, etc.) Education representatives Employers/business leaders Planning and Network Advisory Committee Local consumer-led organizations
List the key issues and concerns identified by stakeholders. Only include items that were raised by multiple stakeholders and/or had broad support. When you finish listing one issue, press “Enter” on your keyboard to create a new bullet point. no local inpatient or intensive outpatient substance abuse treatment facilities no crisis respite facilities need for wraparound behavioral health services/systems of care for children gaps in jail and hospital diversion 3 October, 2012
need for more peer support services need for integrated primary and behavioral health care
System-Wide Priorities: Jail Diversion Strategies Indicate which of the following strategies you use to divert individuals from the criminal justice system.
Intercept Point Components 1: Law enforcement and emergency Co-mobilization with Crisis Intervention Team (CIT) or MH Deputies services Co-location with CIT or MH Deputies Training law enforcement staff Documenting police contacts with persons with mental illness Training law enforcement staff Police-friendly drop-off point Service linkage and follow-up for individuals who are not hospitalized Other: Mobile Crisis Outreach Team
2: Post-arrest: initial detention and Staff at court to review cases for post-booking diversion initial hearings Routine screening for mental illness and diversion eligibility Staff assigned to help defendants comply with conditions of diversion Staff at court who can authorize alternative services to incarceration Link to comprehensive services Other:
3. Post-initial hearing: jail, courts, Routine screening for mental illness and diversion eligibility forensic evaluations, and forensic Mental Health Court commitments Veterans’ Court Drug Court Community Court Re-entry Court Outpatient Competency Restoration Services for persons Not Guilty by Reason of Insanity Services for persons with other Forensic Outpatient Commitments Providing services in jail for persons Incompetent to Stand Trial 4 October, 2012
Intercept Point Components Compelled medication in jail for persons Incompetent to Stand Trial Providing services in jail (for persons without outpatient commitment) Staff assigned to serve as liaison between specialty courts and services providers Link to comprehensive services Other: Telepsychiatry services in area jails.
4: Re-entry from Jails, prisons, and Providing transitional services in jails forensic hospitalization Staff designated to assess needs, develop plan for services, and coordinate transition to ensure continuity of care at release Structured process to coordinate discharge/transition plans and procedures Specialized case management teams to coordinate post-release services Other:
5: Community corrections and Routine screening for mental illness and substance use disorders community support programs Training for probation or parole staff TCOOMMI program Forensic ACT Staff assigned to facilitate access to comprehensive services; specialized caseloads Staff assigned to serve as liaison with community corrections Working with community corrections to ensure a range of options to reinforce positive behavior and effectively address noncompliance Other:
System-Wide Priorities: Management of Hospital Utilization Complete the check boxes to indicate which strategies you use to minimize utilization of state and community hospitals, including emergency departments. A single strategy may be applicable to multiple populations. For each strategy that you use, identify the target population(s): Freq. State Hosp: Population with frequent state hospital admissions (ten or more psychiatric hospitalizations in the past five years with at least one admission in the past one year) LT State Hosp: Population with long-term state hospital stays (one year or longer)
5 October, 2012
Local Hosp/ER: Population with high utilization of community hospital and emergency services for psychiatric issues (as defined by LMHA/local stakeholders) Population on forensic commitments (Forensic)
Freq. LT Local State State Hosp/ Hosp. Hosp. ER Forensic Strategies Regular multi-agency review of data relating to admission and length of stay to identify clients with repeat admission and/or extended LOS Regular multi-agency reviews of cases with high utilization to identify contributing systemic issues and develop system improvements MCOT support for local emergency departments. Regular multi-agency review of cases with high utilization to identify and address individual client needs Multi-agency, multi-disciplinary discharge planning Outpatient case manager meetings with client during hospitalization and facilitating transition to community services Court liaisons to assist in identifying appropriate alternatives to long-term forensic commitment. Regular review of clients on forensic commitment to identify those who may be recommended for transfer to an alternative setting. Assigned liaison to facilitate discharge planning and transition to community services Identifying and transitioning clients to long term care facilities Frequent follow-up appointments during immediate post-discharge/crisis period Home visits during post-discharge/crisis period Regular telephone follow-up, especially during post discharge/crisis period Regular team staffings focused on clients with history of high utilization Regular multi-disciplinary treatment planning with community partners involved 6 October, 2012
Freq. LT Local State State Hosp/ Hosp. Hosp. ER Forensic Strategies in client’s treatment and support Evaluation and intervention related to identify and address substance use issues Specialized caseload (team or individual) for clients with history of high utilization Multi-agency action to develop and/or improve COPSD services (availability, access, level of coordination/integration, quality, etc.) Telephone or home visit (e.g., MCOT) follow-up for no-shows Home-based treatment services 24/7 access to support (warmline, on-line chat, peer sponsor, etc.) Peer specialist participation in team staffings and/or ACT team Peer support services Use of long-term injectable medication when appropriate Community Resource Coordination Groups Wellness Recovery Action Planning or other person-centered, strength-based and recovery-based approaches Housing assistance (Supported Housing, PATH outreach, housing vouchers, etc.) Transportation assistance to ensure access to services Use of token economies or other incentives Focused effort to develop and/or engage natural community supports “Hotspot” evaluation of catchment area zip codes and use of data to plan resource allocation, outreach to community partners, etc. Other: Participation in the Drug Court Team, TCOOMMI program for Adults and Youth
7 October, 2012
Other System-Wide Strategic Priorities List current activities in the following areas and any plans for the next two years. When you finish entering one bullet point, press “Enter” on your keyboard to create a new bullet and form field in the same cell. For those areas not required in the DSHS Performance Contract, enter NA if the LMHA has no current or planned activities. Space is provided to note activities related to other local priorities, if applicable.
Area of Focus Current Activities Plans Implementing and Meaningful fidelity is accomplished through Continue this practice, updating training, maintaining fidelity with consistent continuous training, supervision supervision, and oversight as evidence evidence-based practices and oversight to prevent migration away based practices evolve. from established principles and practices for the duration of the provision of services. Transition to a recovery- Currently part of Recovery-Oriented Continue planning and implementation oriented system of care, Systems of Care task force assessing and process and involvement with Via HOPE including development of addressing community needs. Participated NAD other evidence-based practices.. peer support services and in Via HOPE Recovery Institute, which other consumer promotes mental health system involvement in Center transformation by (1) helping activities and operations organizations develop culture and practices (e.g., planning, evaluation) that support and expect recovery, and (2) promoting consumer (aka peer, person in recovery), youth/ young adult, and family voice in the transformation process and the future, transformed mental health system. Incorporating trauma- One counselor and two counseling interns Countiue best practice research and informed principles into trained in CPT. incorporate as applicable care Addressing the needs of Planning stage of partnering with a Fully implement intensive outpatient consumers with co- intensive outpatient substance abuse substance abuse services occurring substance use provider and offering psychiatric support disorders during the course of the treatment. Integrating behavioral in intitial planning phase of integrated Plan to start project with local FQHC to 8 October, 2012
Area of Focus Current Activities Plans health and primary care health care being integrated health care as part of 1115 services and meeting Waiver. physical healthcare needs of Formal Agreement with primary care consumers. provider? Yes No Formal Agreement with primary care provider? Yes No Identifying and addressing Started Veteran's peer support program; Working with stakeholders to pursue needs of veterans currently employ veterans services Veteran's Court coordinator. Addressing diversity and working with area stakeholders on best assess needs in this area and incorporate cultural needs of consumers ways to reach and treat immigrant/non- into 1115 waiver projects. english speaking populations Local Priorities (Specify):
Local Priorities (Specify):
Local Unmet Needs In each of the following area, list unmet service needs. When you finish entering one bullet point, press “Enter” on your keyboard to create a new bullet in the same cell.
Service Unmet Service Needs Adult Services no local intensive outpatient substance abuse treatment facilities gaps in local diversion process lack of primary and behavioral healthcare integration
Child & Adolescent at risk of losing evidence-based best practice wraparound services in local school district. Services Crisis Services no local crisis respite facilities Other
9 October, 2012
Local Priorities and Plans Based on indicators of unmet needs, stakeholder inputs, and your internal assessment, identify your local priorities for the next two years. These might include changes in the array of services, allocation of resources, implementation of new strategies or initiatives, service enhancements, quality improvements, etc. Examples of possible priorities: Implementing WRAP Reducing state hospital admissions Integrating trauma-informed principles into services Expanding consumer/peer involvement in planning, service delivery, and evaluation Addressing primary healthcare needs or management of chronic physical disorders Improving access to services Jail diversion For each priority, identify at least one key objective and strategies/actions you will implement to achieve the objective(s). List at least one but no more than five priorities. These may relate to projects you are implementing under the Medicaid Texas Healthcare Transformation and Quality Improvement Program 1115 Waiver. When you finish entering one bullet point, press “Enter” on your keyboard to create a new bullet in the same cell.
Priority (Specify): Develop and implement crisis stabilization services to address the identified gaps in the current community crisis system. Objectives Strategies/Actions To develop a behavioral health crisis respite program Convene community stakeholders who can support the that will serve as an alternative to hospitalization and development of crisis stabilization services to conduct a incarceration, allowing local residents to remain in the gap analysis of the current community crisis system and community, improving their quality of life with the develop a specific action plan that identifies specific crisis side benefit of reducing state hospital and stabilization services to address identified gaps. incarceration costs. Analyze the current system of crisis stabilization services available in the community including capacity of each service, current utilization patterns, eligibility criteria and discharge criteria for each service. Assess the behavioral health needs of patients currently receiving crisis services in the jails, EDs, or psychiatric hospitals. Determine the types and volume of services needed to resolve crises in community‐based settings. Then conduct a gap analysis that will result in a data‐ driven plan to develop specific community‐based crisis 10 October, 2012
Priority (Specify): Develop and implement crisis stabilization services to address the identified gaps in the current community crisis system. Objectives Strategies/Actions stabilization alternatives that will meet the behavioral health needs of the patients (e.g. a minor emergency stabilization site for first responders to utilize as an alternative to costly and time consuming Emergency Department settings). Explore potential crisis alternative service models and determine acceptable and feasible models for implementation. Review the intervention(s) impact on access to and quality of behavioral health crisis stabilization services and identify “lessons learned,” opportunities to scale all or part of the intervention(s) to a broader patient population, and identify key challenges associated with expansion of the intervention(s), including special considerations for safety‐net populations
Priority (Specify): Design, implement, and evaluate research‐supported and evidence‐based interventions tailored towards individuals in the target population. Objectives Strategies/Actions Implement a Continuum of Care (CoC) Program Develop CHILD AND ADOLESCENT WRAPAROUND providing intensive wraparound services and supports SERVICES- an early service delivery model that provides for children and adults with behavioral health needs in individualized comprehensive services and supports to the top 21 counties of the Texas Panhandle. children and adolescents with serious emotional and/or behavioral disturbance across the local service area. This program, which will initially be delivered through a partnership between TPC and Amarillo Independent School District targeting children in grades pre-k through 12th grade, is aimed at maintaining children in less restrictive school and family settings and preventing hospitalization, and will work with community agencies, 11 October, 2012
Priority (Specify): Design, implement, and evaluate research‐supported and evidence‐based interventions tailored towards individuals in the target population. Objectives Strategies/Actions families, and youths for the purpose of improving access and expanding the array of coordinated community-based, culturally and linguistically competent service/supports for children and youth with a serious emotional disturbance and their families. Future focus will include expanding to surrounding school districts. Implement a 30 DAY INTENSIVE OUTPATIENT TREATMENT Program- Target adults who have a co- occurring diagnosis of substance abuse and mental illness who experience chronic or intermittent homelessness. Program will encourage services in the least restrictive setting that is clinically appropriate to meet the individual’s needs. Services will include partnering with the City of Amarillo Department of Public Health, and with shelters to provide a sober living environment for program participants, behavioral health services, substance abuse services, crisis services, psychiatric services, case management, skills training, employment services, peer support and other services that promote overall health and well being. CRIMINAL JUSTICE DIVERSION UNIT- created specifically to address current gaps in diversion services, this unit will target adults with behavioral health needs who have repeat contacts with the criminal justice system so they will not return, or not return as frequently. Three pronged approach will include: Crisis Transition that will focus on pre-booking and post-booking diversion while headquartered at the Randall County Jail, and on treating repeat offenders reentering the local community as part of the Randall County Prisoner Re-entry Program, a successful local diversion/reintegration program; Court/Jail Liaison that will advocate for clients with 12 October, 2012
Priority (Specify): Design, implement, and evaluate research‐supported and evidence‐based interventions tailored towards individuals in the target population. Objectives Strategies/Actions mental illness so that they can be treated in the least restrictive treatment environment that is feasible and will pursue incremental reductions in the number of law enforcement contacts, jail days, probation violations, or new charges for program participants; and Service Coordination that will provide increased engagement for clients who have been historically hard to engage and have ended up in a “revolving door” of encounters with law enforcement, mental health agencies, hospitals, etc.
Priority (Specify): Design, implement, and evaluate projects that provide integrated primary and behavioral health care services. Objectives Strategies/Actions Using primary health care staff, case managers, social TPC will identify sites for integrated care projects, which workers, and others to provide coordinated and would have the potential to benefit a significant number of integrated primary and behavioral health services for patients in the community. Ease of access, centralized the first time in the Amarillo, TX area through the co- locations, etc. will all be factors. location of primary care medical services and Develop provider agreements whereby co‐scheduling and community-based behavioral health services. information sharing between physical health and • Increase percentage of individuals receiving both behavioral health providers could be facilitated. Other physical and behavioral health care at the established successful integrated care sites will be used as models for locations. this. • Demonstrate improvement in quality of life, as Establish protocols and processes for communication, measured by an evidence-based and validated data‐sharing, and referral between behavioral and assessment tool, for the target population. physical health providers. Other successful integrated care sites, such as programs in Lubbock, TX and Austin, TX, will be used as models for this. Recruit a number of specialty providers to provide services in the specified locations. This will be done in 13 October, 2012
Priority (Specify): Design, implement, and evaluate projects that provide integrated primary and behavioral health care services. Objectives Strategies/Actions conjunction with partner agencies. Train physical and behavioral health providers in protocols, effective communication and team approach. Build a shared culture of treatment to include specific protocols and methods of information sharing that include: Regular consultative meetings between physical health and behavioral health practitioners; Case conferences on an individualized as‐needed basis to discuss individuals served by both types of practitioners; and/or Shared treatment plans co‐developed by both physical health and behavioral health practitioners. Other successful integrated care sites will be used as models for this. Acquire data reporting, communication and collection tools (equipment) to be used in the integrated setting. Other successful integrated care sites will be used as models for this. Explore the need for and develop any necessary legal agreements that may be needed in a collaborative practice. Arrange for utilities and building services for these settings. Research into this has already begun. Develop and implement data collection and reporting mechanisms and standards to track the utilization of integrated services as well as the health care outcomes of individual treated in these integrated service settings. Other successful integrated care sites will be used as models for this. Conduct quality improvement for project using methods such as rapid cycle improvement. This will be planned in conjunction with primary health care partners.
14 October, 2012
Priority (Specify): Design, implement, and evaluate projects that provide integrated primary and behavioral health care services. Objectives Strategies/Actions
Priority (Specify): Recruit, train and support consumers of mental health services to provide peer support services Objectives Strategies/Actions Design, implement, and evaluate whole health peer Train administrators and key clinical staff in the use of support for individuals with mental health and /or peer specialists as an essential component of a substance use disorders comprehensive health system. This will be done using materials received through collaboration with Via Hope. Conduct readiness assessments of organization that will integrate peer specialists into their network. Weaknesses will be identified through assessment informed by Via Hope collaboration. Some weaknesses have already been identified through Via Hope collaboration, such as not enough peer input into service delivery planning. Identify peer specialists interested in this type of work. The Center will work with the local NAMI chapter and the Amarillo Area Mental Health Consumers (a local independent peer support organization) to identify prospective peer specialists. Train identified peer specialists in whole health interventions, including conducting health risk assessments, setting SMART goals, providing educational and supportive services to targeted individuals with specific disorders (e.g. hypertension, diabetes, or health risks (e.g. obesity, tobacco use, physical inactivity. These program interventions will be used to enhance and support services provided in all projects we are proposing, including our integrated health care program, continuum of care program, and crisis respite program. Our Center is also going tobacco free; this project will 15 October, 2012
Priority (Specify): Recruit, train and support consumers of mental health services to provide peer support services Objectives Strategies/Actions provide needed support for clients. Implement health risk assessments to identify existing and potential health risks for behavioral health consumers. These assessments will be added to intake and update packets for behavioral health clients, and completed at the same time as intakes and updates. Identify patients with serious mental illness who have health risk factors that can be modified. These clients will be identified through the use of health assessments as described above. Implement whole health peer support. Will develop individual as well as group support, using peers as educators and encouragers. Connect patients to primary care and preventive services. Patients who have health needs identified through assessments and other means will be linked to a nurse case manager, who will refer to needed resources, including the Center’s integrated Health Program. Track patient outcomes. Review the intervention(s) impact on participants and identify “lessons learned,” opportunities to scale all or part of the intervention(s) to a broader patient population, and identify key challenges associated with expansion of the intervention(s), including special considerations for safety‐net populations. This will include a cross disciple evaluation of data by staff/stakeholders.
16 October, 2012
Priority (Specify): Objectives Strategies/Actions
Texas Healthcare Transformation and Quality Improvement Program 1115 Waiver List the titles of all projects you proposed for implementation under the Regional Health Partnership (RHP) plan. Identify the RHP Region(s) associated with each project. In each of the three status columns, check Yes or No. If approval status is unknown, leave blank.
1115 Waiver Projects RHP Project Title Accepted Approved Approved Region(s) in RHP by HHSC by CMS Plan 12 Development of behavioral health crisis stabilization Yes Yes Yes services as alternatives to hospitalization No No No 12 Provide an intervention for a targeted behavioral health Yes Yes Yes population to prevent unnecessary use of services in a No No No specified setting (i.e., the criminal justice system, ER, urgent care etc.) 12 Integrate Primary and Behavioral Health Care Services Yes Yes Yes No No No 12 Recruit, train, and support consumers of mental health Yes Yes Yes services to provide peer support services No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes
17 October, 2012
1115 Waiver Projects RHP Project Title Accepted Approved Approved Region(s) in RHP by HHSC by CMS Plan No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No
18 October, 2012
Mental Health Block Grant Inventory of Services The following table identifies the components of the “Good and Modern Addictions and Mental Health Service System” defined by SAMHSA. It reflects the full range of behavioral health services, including substance abuse services and excluding IDD services. These inventories are for information only and do not define DSHS requirements. SAMHSA has posted a description of the Good and Modern system on its website: http://www.samhsa.gov/healthreform/docs/good_and_modern_4_18_2011_508.pdf.
The survey is for behavioral health services available to individuals eligible for DSHS-funded services. For each service listed: Identify which age groups (if any) currently receive or have access to the service in your local service area, either through the LMHA (regardless of funding source) or elsewhere in the community. Identify the approximate percent of service area in which the service is available. It is acceptable to enter the percent of counties in which the service is available. Indicate whether the service is provided through the LMHA, through another community provider, and/or through collaboration between the LMHA and one or more community partners. Check as many columns as applicable.
Category Pop Service % of Source Area . t r l n A l e o o u H i h d t d t M A a A O L r / o d l b i a h l l C o C
Healthcare Generalized and specialized outpatient medical services 50 Home/ Physical Acute primary care 50 Health General health screens, tests, and immunization 50 Comprehensive case management 20 Care coordination and health promotion 30 Comprehensive transitional care 10 Individual and family support 10 Referral to community services 100 Prevention Screening, Brief Intervention, and Referral to Treatment (SBIRT) 100 (including Brief motivational interviews 10 Promotion) Screening, Brief Intervention, and Referral for Tobacco Cessation 19 October, 2012
Category Pop Service % of Source Area . t r l n A l e o o u H i h d t d t M A a A O L r / o d l b i a h l l C o C
Parent training 100 Facilitated referral 100 Relapse prevention/Wellness recovery support Warm line Engagement Assessment 100 Services Specialized evaluations (psychological, neurological) 100 Service planning (including crisis planning) 100 Consumer/family education 100 Outreach Outpatient Individual evidenced-based therapies 100 Group therapy 20 Family therapy 20 Multi-family therapy Consultation with staff/caregivers 100 Medication Medication management 100 Services Pharmacotherapy (including MAT) 100 Laboratory services 100 Community Parent/Family/Caregiver Support 30 Support Skill building (social, daily living, cognitive) 100 (Rehabilitative) Case management 100 Behavioral management 50 Supported employment Permanent supportive housing Recovery housing Therapeutic mentoring
20 October, 2012
Category Pop Service % of Source Area . t r l n A l e o o u H i h d t d t M A a A O L r / o d l b i a h l l C o C
Traditional healing services Other Supports Personal care (Habilitative) Homemaker Respite Supported education services Transportation Assisted living services Recreational services Interactive communication technology devices (Technological support services) Trained behavioral health interpreters Intensive Substance abuse intensive outpatient services Support Partial hospital Services Assertive community treatment 100 Intensive home based treatment 100 Multi-systemic therapy Intensive case management 100 Out-of-Home Crisis residential/stabilization Residential Clinically managed 24-hour care Services Clinically managed medium intensity care Adult mental health residential Children’s mental health residential Youth substance abuse residential Therapeutic foster care Acute Intensive Mobile crisis services 100
21 October, 2012
Category Pop Service % of Source Area . t r l n A l e o o u H i h d t d t M A a A O L r / o d l b i a h l l C o C
Services Medically monitored intensive inpatient 20 Peer-based crisis services Urgent care services 23-hour crisis stabilization service 24/7 crisis hotline services 100 Recovery Peer support 20 Supports Peer recovery support coaching 20 Peer-operated recovery community center 20 Supports for self-directed care Continuing care for substance abuse disorders Relapse Prevention/Wellness Recovery Support Behavioral health peer navigator
22