Eliminating Needless NPO in the ED
Identify Stakeholders Standard Rollout Process
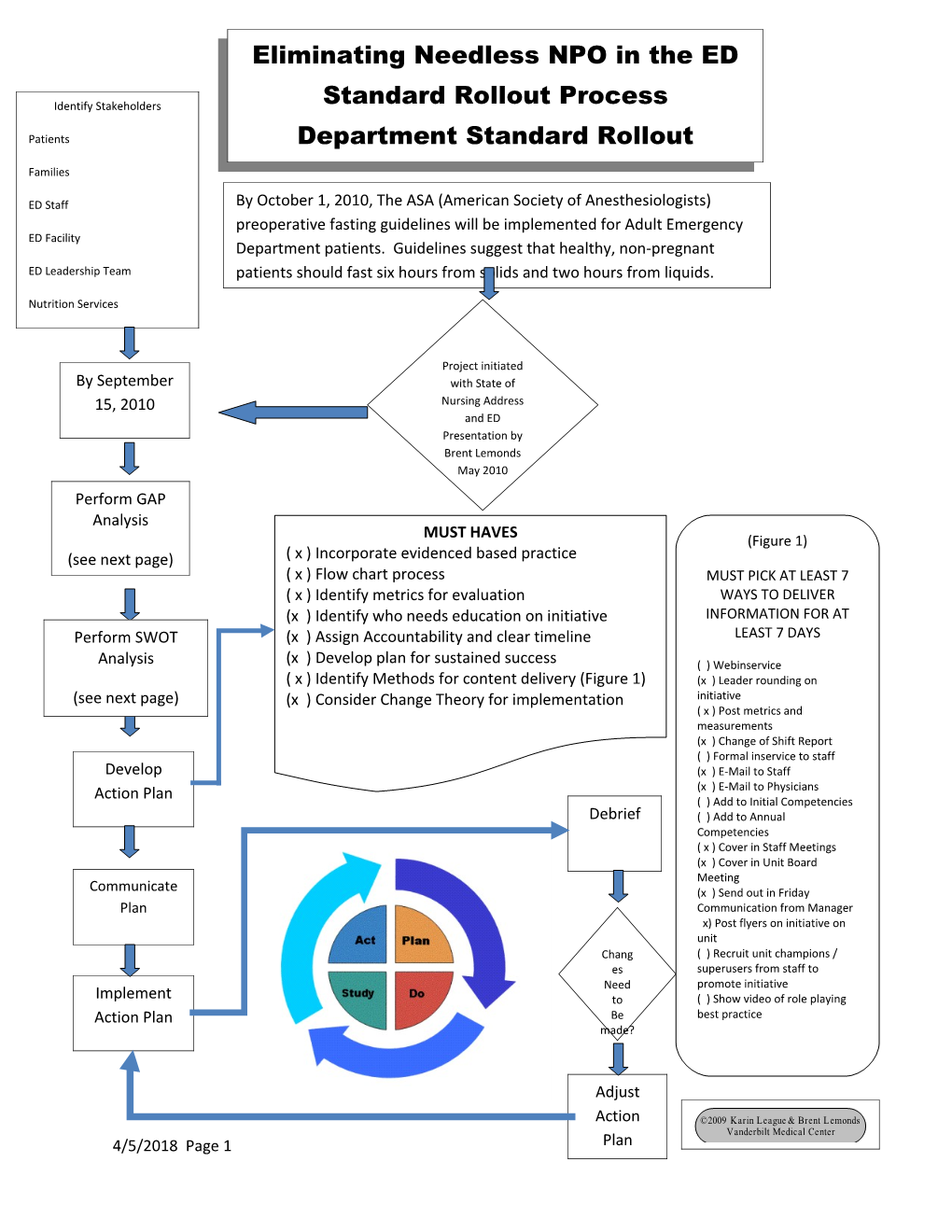
Patients Department Standard Rollout Families Process ED Staff By October 1, 2010, The ASA (American Society of Anesthesiologists) preoperative fasting guidelines will be implemented for Adult Emergency ED Facility Department patients. Guidelines suggest that healthy, non-pregnant ED Leadership Team patients should fast six hours from solids and two hours from liquids.
Nutrition Services
Project initiated By September with State of 15, 2010 Nursing Address and ED Presentation by Brent Lemonds May 2010 Perform GAP Analysis MUST HAVES (Figure 1) (see next page) ( x ) Incorporate evidenced based practice ( x ) Flow chart process MUST PICK AT LEAST 7 ( x ) Identify metrics for evaluation WAYS TO DELIVER (x ) Identify who needs education on initiative INFORMATION FOR AT Perform SWOT (x ) Assign Accountability and clear timeline LEAST 7 DAYS
Analysis (x ) Develop plan for sustained success ( ) Webinservice ( x ) Identify Methods for content delivery (Figure 1) (x ) Leader rounding on (see next page) (x ) Consider Change Theory for implementation initiative ( x ) Post metrics and measurements (x ) Change of Shift Report ( ) Formal inservice to staff Develop (x ) E-Mail to Staff (x ) E-Mail to Physicians Action Plan ( ) Add to Initial Competencies Debrief ( ) Add to Annual Competencies ( x ) Cover in Staff Meetings (x ) Cover in Unit Board Meeting Communicate (x ) Send out in Friday Plan Communication from Manager x) Post flyers on initiative on unit Chang ( ) Recruit unit champions / es superusers from staff to Need promote initiative Implement to ( ) Show video of role playing Action Plan Be best practice made?
Adjust
Action ©2009 Karin League & Brent Lemonds Vanderbilt Medical Center 4/5/2018 Page 1 Plan GAP ANALYSIS Directions: Consider organizations mission, vision, strategy, and objectives.
CURRENT STATE GAP FUTURE STATE Pt is placed on Lack of education Procedure times NPO status upon regarding ASA are identified and admission to ED Guidelines patients given and held without solids up to six fluids or solids hours prior to until after procedure and procedures and clear liquids up results. until two hours prior to procedure. Patients placed on Lack of education Patients have extended NPO regarding ASA increased comfort status are Guidelines levels, are uncomfortable, hydrated prior to thirsty, hungry, procedures, able to dehydrated, have receive routine compromised medications and acid/base balance, have better interrupted routine glucose control. medication schedule and poor glucose control.
4/5/2018 Page 2 4/5/2018 Page 3 Must Haves STRENGTHS WEAKNESSES Increases patient satisfaction Long held perception that Increases family satisfaction keeping patients NPO Increases staff satisfaction preoperatively for extended Evidence Based Practice periods is essential to prevent aspiration. There is no evidence to support this theory. OPPORTUNITIES THREATS This project addresses the Physicians not willing to Innovation Pillar change Applies evidence based Nursing staff not willing to practice in the clinical setting change Educates staff regarding ASA Increased nutrition cost to guidelines department Keeps patients homeostatic and better prepared for procedures Multi-disciplinary
Incorporate evidence based practice
Anderson, M, Comrie R. (2009, July). Adopting preoperative fasting guidelines. AORN, 90(1): 73-80
Brady M., Kinn S., Stuart P, (2004, April). Preoperative fasting for adults to prevent perioperative complications. Evidence Based Nursing, 7(2) :44.
4/5/2018 Page 4 Brewer JP, Bosse G, Seifert S, Prochnow L, Martin J, Schleppers A., Geldner G, Soreide E, Spies C. (2009, September). Pre-operative fasting: a nationwide survey of German anaesthesia departments. Acta Anaesthesiol Scand. Epub ahead of print.
Cote, Charles J. M.D., (1990, April). NPO after Midnight for Children-A Reappraisal. The Journal of Anesthesiology. 72 (4) 589-592.
Crenshaw, Jeannette T., Winslow, Elizabeth H., (2002, May). Preoperative Fasting: Old Habits Die Hard: Research and published guidelines no longer support the routine use of ‘NPO after midnight’, but the practice persists. American Journal of Nursing. 102(5) 36-44.
Jarvela K, Maaranen P, Sisto T., (2008, July). Pre-operative oral carbohydrate treatment before coronary bypass surgery . Acta Anaesthesiol Scand. Epub 2008 May 12.
Ljungqvist O, Soreide E., (1990, April). Preoperative fasting. British Journal of Surgery Society Ltd., 90(4):400-6.
Meisner M., Ernhofer U., Schmidt J., (2008, September). [Liberalisation of preoperative fasting guidelines: effects on patient comfort and clinical practicability during elective laparoscopic surgery of the lower abdomen]. Zentralbl Chir. 133(5):479-85. Epub 2008 Oct. 15.
Murphy, Glenn S, Auit, Michael L., Wong, Hak Yui, Szokoi, Joseph W., (2000, February). The effect of a new NPO policy on operating room utilization. Journal of Clinical Anesthesia. 12(1):48-51.
Maltby, J. Roger, (2006, September). Fasting from midnight – the history behind the dogma. Best Practice & Research Clinical Anaestesiology. 20(3):363-378.
Scarlett M, Crawford-Sykes A, Nelson M., (2002, December). Preoperative starvation and pulmonary aspiration. New perspectives and guidelines. West Indian Medical Journal . 51(4):241-5.
Soreide E, Ljungqvist O., (2006, September) Modern preoperative fasting guidelines: a summary of the present recommendations and remaining questions. Best Pract Res Clin Anaesthesiol. 20(3):483-91.
Spies CD, Breuer JP, Gust R, Wichmann M, Senkal M, Kampa U, Weissauer W. Schleppers A. Soreide E, Martin E, Kaisers U, Falke KJ, Haas N, Kox WJ, . (2003, November). [Preoperative fasting. An update], Anaesthesist. 52(11):1039-45.
Stuart PC, (2006, September). The evidence base behind modern fasting guidelines. Best Pract Res Clin Anaesthesiol. 20 (3):457-69.
Yuill KA, Richardson RA, Davidson HI, Garden OJ, Parks RW. (2005, February). The administration of an oral carbohydrate-containing fluid prior to a major elective upper-gastrointestinal surgery preserves skeletal muscle mass postoperatively—a randomized clinical trial. Clinical Nutrition. 24(1):32-7.
4/5/2018 Page 5 Flowchart the Process
4/5/2018 Page 6 ED Prolonged NPO Improvement Project Monday, June 14, 2010
Procedure is scheduled
Yes No Is Time slot Give solids until 6 Available hours prior to NPO as ordered procedure
Give clear liquids until 2 hours prior to procedure
Patient able to take meds approved before procedure with a sip of water.
Better glucose control, Better hydration. Better comfort and satisfaction
4/5/2018 Page 7 Identify metrics for evaluation: PRC data, NPO staff survey (Before and after implementation), nurse driven patient outcomes, patient satisfaction, nurse retention rates. Identify who needs education on initiative:
Patients
Families staff leadership team
Nurse champions
Faculty
Residents
Assign accountability and clear timeline:
Action Person Assigned Timeline Status
PRC question formulated Traci Denton RN with help June 2010 complete and submitted from Brent
Survey Monkey NPO survey Traci Denton RN July 2010 In progress distributed to ED nursing staff
Evaluate NPO Survey Traci Denton RN August 1, 2010 results
Set up meeting with Ian Traci Denton RN July 27,2010 Jones MD to present plan
Set up meeting with Dr. Traci Denton RN August 10, 2010 Moran and Dr. Jones to present plan
Present plan in September Traci Denton RN September 13, 15 staff meetings and 17 Member of management
4/5/2018 Page 8 Action Person Assigned Timeline Status
team conducting meetings
Present plan in September Traci Denton RN September 28, Unit Board meeting 2010
Evaluate response to PRC Traci Denton with help October 1, 2010 question from Gary
Place plan in spindle report Traci Denton RN September 27- x 7 days October 3, 2010
Send out in Friday Janice Sisco RN as September 24, Communication submitted by Traci Denton 2010 and October RN 1. 2010
Communicate to Physicians Traci Denton RN with September 27, via email assistance in distribution 2010
Post flyers on unit Traci Denton RN September 27, 2010
Evaluate response to PRC Traci Denton with help November 1, 2010 question post from Gary (and monthly x 6 implementation months)
Repeat NPO survey to Traci Denton RN November 1, 2010- nursing staff and evaluate December 1, 2010 post implementation results
Develop plan for sustained success: sustained success will be achieved through ongoing leader rounding for outcomes, incorporation of education into orientation pathway, at least yearly education to staff, sharing of outcomes data with staff linking them to the initiative.
4/5/2018 Page 9 Identify Methods of Content Delivery: See figure 1 for summary.
Change Theory:
Stetler Model Theory-
This theory integrates EBP with research.
There are five phases: 1) Preparation
2) Validation
3) Comparative evaluation and decision making
4) Translation and Application
5) Evaluation
http://74.6.239.67/search/cache?ei=UTF-8&p=Stetler+Model+Theory&fr=yfp-t- 152&u=courseweb.edteched.uottawa.ca/nsg6133/Course_Modules/Module_PDFs/Stetler- Marram.pdf&w=stetler+model+theory+theories&d=DwzyEd29TeE2&icp=1&.intl=us&sig=gA rTsgbpYybXu1qZMKbNfw--
Knowledge Translation
-provides a framework that may be helpful in considering the challenges that clinicians are likely to face when attempting to implement evidence based practice.
- exchange, synthesis, and ethically sound application of knowledge within a complex system of interactions among researchers and users to accelerate capture of the benefits of research.
Rogers Diffusion of Innovations-
-Behavioral theory that describes the process the user goes through in the adaptation/rejection of new ideas, practices, and technology.
4/5/2018 Page 10
4/5/2018 Page 11