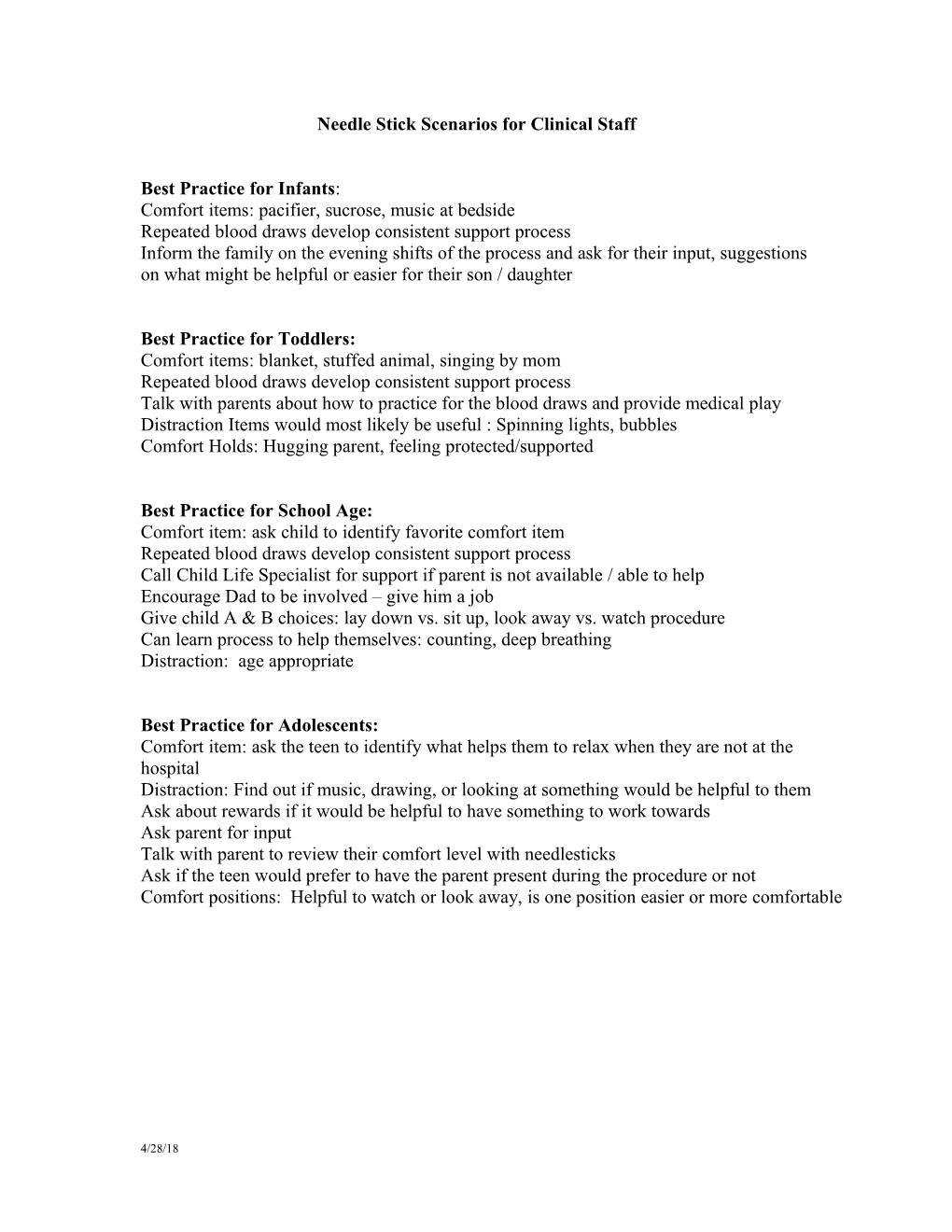
Needle Stick Scenarios for Clinical Staff
Best Practice for Infants: Comfort items: pacifier, sucrose, music at bedside Repeated blood draws develop consistent support process Inform the family on the evening shifts of the process and ask for their input, suggestions on what might be helpful or easier for their son / daughter
Best Practice for Toddlers: Comfort items: blanket, stuffed animal, singing by mom Repeated blood draws develop consistent support process Talk with parents about how to practice for the blood draws and provide medical play Distraction Items would most likely be useful : Spinning lights, bubbles Comfort Holds: Hugging parent, feeling protected/supported
Best Practice for School Age: Comfort item: ask child to identify favorite comfort item Repeated blood draws develop consistent support process Call Child Life Specialist for support if parent is not available / able to help Encourage Dad to be involved – give him a job Give child A & B choices: lay down vs. sit up, look away vs. watch procedure Can learn process to help themselves: counting, deep breathing Distraction: age appropriate
Best Practice for Adolescents: Comfort item: ask the teen to identify what helps them to relax when they are not at the hospital Distraction: Find out if music, drawing, or looking at something would be helpful to them Ask about rewards if it would be helpful to have something to work towards Ask parent for input Talk with parent to review their comfort level with needlesticks Ask if the teen would prefer to have the parent present during the procedure or not Comfort positions: Helpful to watch or look away, is one position easier or more comfortable
4/28/18 Immunization Scenarios:
A. Infant: 2 month old girl/boy in for three injectable and one oral immunizations
This first-time mother is present and nervous about the pain her child will feel from the shots Your clinic practice is to give two injections at the same time using 2 clinical staff members
1. What things would be important for you to consider prior to giving these immunizations? 2. What are some things you might do to help reduce pain and anxiety for this child? 3. What comfort positions would you discuss with this mother? 4. How would you involve the family? 5. After the poke, how do you communicate to the parent or the team about things that worked?
B. Toddler: 12 month old boy presenting for 3 injectable immunizations
Parent (mother only) exhausted Active child, runs when he sees the white coats
1. What things would be important for you to consider prior to giving these immunizations? 2. What are some things you might do to help reduce pain and anxiety for this child? 3. What comfort positions would you discuss with this mother? 4. How would you involve the family? 5. After the poke, how do you communicate to the parent or the team about things that worked?
C. Pre-Kindergarten Visit: 4 year old girl in for pre-kindergarten shots
This patient will be receiving four injections at this visit The child is scared The mom is negotiating with child saying “if you sit still, we will stop at McDonalds on our way home” The child is becoming more anxious
1. What things would be important for you to consider prior to giving these immunizations? 2. What are some things you might do to help reduce pain and anxiety for this child? 3. What comfort positions would you discuss with this mother? 4. How would you involve the family? 5. After the poke, how do you communicate to the parent or the team about things that worked?
4/28/18 D. School Ager: Annual flu immunization and lab work
Child is scared Parent (father only) reports that his daughter is very fearful and has asthma episodes with stressful situations Recently hospitalized Girl is crying quietly and you can tell she is very afraid
1. What things would be important for you to consider prior to giving these immunizations? 2. What are some things you might do to help reduce pain and anxiety for this child? 3. What comfort positions would you discuss with this father? 4. How would you involve the family? 5. After the poke, how do you communicate to the parent or the team about things that worked?
E. Teenager: 14 year old boy here for tetanus immunization
Highly anxious Requests to have the tetanus immunization in his leg. (You know you can’t honor that choice!) Loves video games and has a DSI with him at the appointment
1. What things would be important for you to consider prior to giving these immunizations? 2. What are some things you might do to help reduce pain and anxiety for this child? 3. What comfort positions would you discuss? 4. How would you know if you should involve the family? 5. After the poke, how do you communicate to the parent or the team about things that worked?
F. Developmentally Delayed: 12 year old girl in the office for immunization
Non-verbal Unable to communicate her needs Limited mobility Parent present and actively involved in her daughter’s care
1. What things would be important for you to consider prior to giving these immunizations? 2. What are some things you might do to help reduce pain and anxiety for this child? 3. What comfort positions would you discuss with this parent? 4. How would you involve the family? 5. After the poke, how do you communicate to the parent or the team about things that worked?
4/28/18