Doncaster & Bassetlaw Area Prescribing Committee October 2016 V7.0
Shared Care Protocol for the Management of Dementia
1.0 INTRODUCTION
This protocol sets out guidelines for assessment and treatment of dementia and responsibilities when care is to be shared between Primary Care and Rotherham Doncaster and South Humber Mental Health NHS Foundation Trust. This protocol applies to any patient with a neurodegenerative dementing process that could respond favourably to cognitive enhancers. In practice this means patients with Alzheimer’s disease, but also could include similar presentations (such as Pick’s Disease and Lewy Body Dementia (LBD)). Mixed vascular and Alzheimer’s dementia can respond to medication, patients with pure vascular dementia are excluded from this protocol.
This document only covers the pharmacological management of dementia. For guidance on BPSD please refer to: BPSD Guidance-February 2015 N.B. Risperidone is the only antipsychotic licensed for BPSD
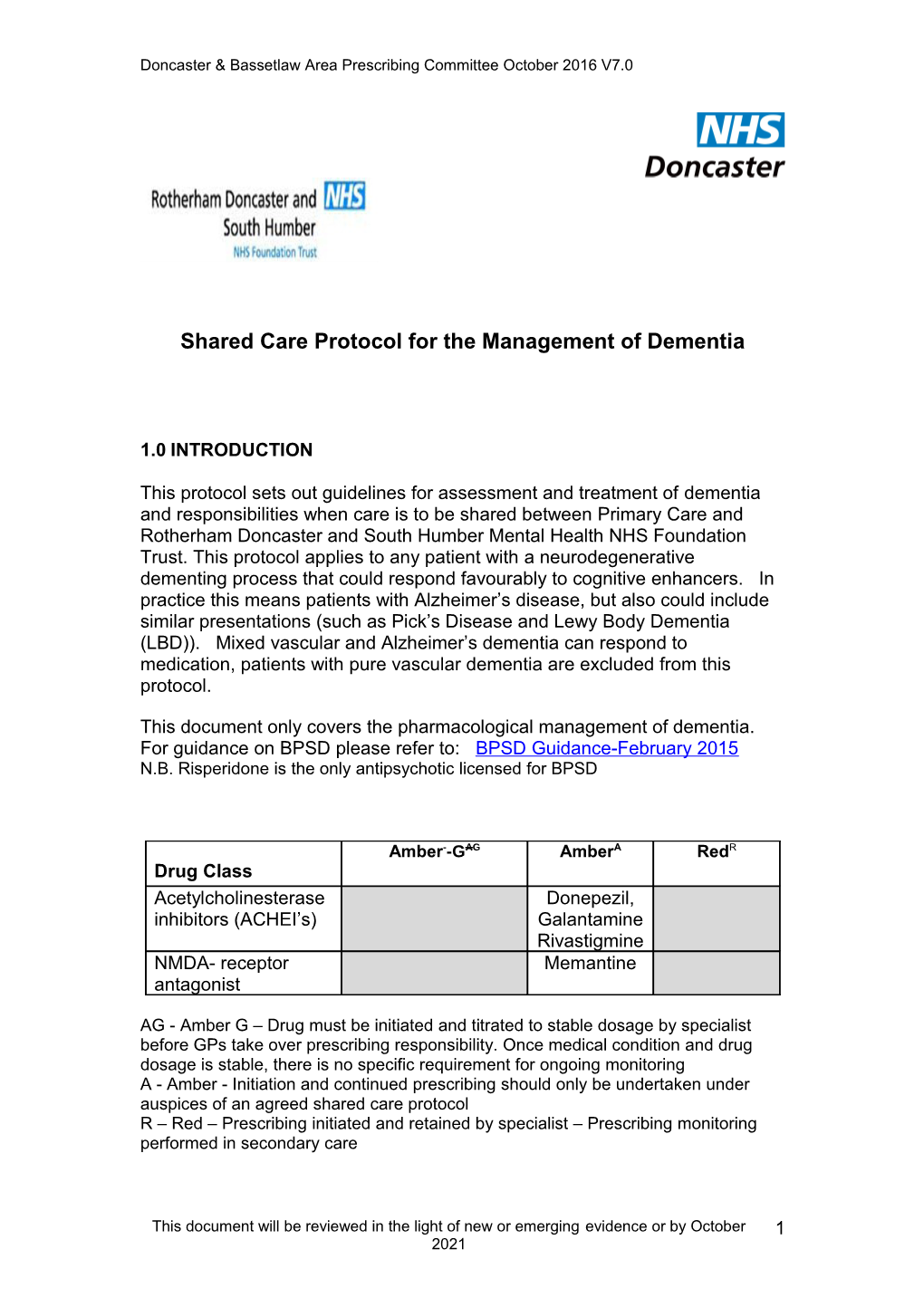
Amber--GAG AmberA RedR Drug Class Acetylcholinesterase Donepezil, inhibitors (ACHEI’s) Galantamine Rivastigmine NMDA- receptor Memantine antagonist
AG - Amber G – Drug must be initiated and titrated to stable dosage by specialist before GPs take over prescribing responsibility. Once medical condition and drug dosage is stable, there is no specific requirement for ongoing monitoring A - Amber - Initiation and continued prescribing should only be undertaken under auspices of an agreed shared care protocol R – Red – Prescribing initiated and retained by specialist – Prescribing monitoring performed in secondary care
This document will be reviewed in the light of new or emerging evidence or by October 1 2021 Doncaster & Bassetlaw Area Prescribing Committee October 2016 V7.0
2. National Institute for Clinical Excellence (NICE) Indications
Donepezil, galantamine and rivastigmine are recommended as options for the treatment of mild to moderate Alzheimer's disease.
When the decision has been made to prescribe an acetylcholinesterase inhibitor, it is recommended that therapy should be initiated with a drug with the lowest acquisition cost (taking into account required daily dose and the price per dose once shared care has started). However, an alternative acetylcholinesterase inhibitor could be prescribed where it is considered appropriate having regard to adverse event profile, expectations around concordance, medical co-morbidity, possibility of drug interactions, and dosing profiles.
Memantine is recommended for patients with:
Proven intolerance to efficacy of acetyl-cholinesterase-inhibitor
Behaviour that challenges and other non-pharmacological / pharmacological therapies are inappropriate, ineffective or contra–indicated in moderate to severe disease
Evidence of psychosis and other non-pharmacological / pharmacological therapies are inappropriate, ineffective or contra–indicated in moderate to severe disease
Moderate to severe Alzheimer’s disease (MOCA <20/30 or equivalent assessment of severity)
2.1 Symptoms for which an Antidementia drug may be used in the context of Alzheimers
Although many people with dementia retain positive personality traits and personal attributes, as their condition progresses they can experience some or all of the following: Memory loss (for example forgetting the way home or unable to remember names and places) Language impairment – a decline in the ability to talk Communication problems – a decline in the ability to read and write Disorientation Changes in personality and changes in mood Difficulties with activities of daily living
This document will be reviewed in the light of new or emerging evidence or by October 2 2021 Doncaster & Bassetlaw Area Prescribing Committee October 2016 V7.0
Self-neglect Psychiatric symptoms (e.g. apathy, depression or psychosis) and out-of-character behaviour (e.g., aggression, sleep disturbance or disinhibited sexual behaviour, although the latter is not typically the presenting feature of dementia)
Secondary prevention of dementia, vascular and other modifiable risk factors (for example, smoking, excessive alcohol consumption, obesity, diabetes, hypertension and raised cholesterol) should be reviewed in people with dementia, and if appropriate, treated.
3. Drug treatment
For prescribing information please see current BNF: http://www.bnf.org.uk/bnf/bnf/current/index.htm
Or for more detailed prescribing information the summary of product characteristics for the individual drug: http://www.medicines.org.uk/
4.0 SHARED CARE ARRANGEMENTS
Once a stable medication regimen has been established (usually 3 months), physical monitoring and prescribing of amber category drugs can be transferred to primary care with agreement.
GP Responsibilities Secondary Care Responsibilities Identifying patients that are Diagnosis of mild to severe suspected to be suffering from mild Alzheimer’s disease. to severe Alzheimer’s disease. Assessment of mental state. Referral to specialist mental health services for diagnosis Provide appropriate patient/carer and assessment. information and education.
Prescribing of the antidementia Initiation of treatment with drug following initiation and antidementia drug. Dose stabilisation by secondary care adjustment to maintenance with documented evidence of dose. clinical effectiveness. Assessment of effectiveness of treatment at minimum of one To check for interactions with any month after reaching newly prescribed medication. maintenance dose.
Refer back to secondary care with Reassessment on a regular basis any concerns. to ensure continuing benefit,
This document will be reviewed in the light of new or emerging evidence or by October 3 2021 Doncaster & Bassetlaw Area Prescribing Committee October 2016 V7.0
minimum annually. Consider discontinuation, in line with guidance below. Discontinuation of treatment if ineffective or no longer indicated.
Inform primary care of assessments and clinic visits
*Appropriate scales such as the Montreal Cognitive Assessment (MOCA), Severe Impairment Battery (SIB), The Neuropsychiatric Inventory (NPI), and The Bristol Activities of Daily Living (BADL) Scale should be used to help judge effectiveness. Continuation Criteria The patient meets the criteria in the initiation and monitoring in mild to severe Alzheimer’s disease by response in at least one domain which is clinically relevant. Improvement / stabilisation of cognitive function better than expected natural decline e.g. less than expected decline in MOCA score of >5 points in 12 months in moderate disease or 5 points on the SIB over 6 months in severe disease. Meaningful improvement/ stabilisation of functional ability as evidenced by improvement, stabilisation or reduction in expected decline (<10/60 in 12 months) on clinically relevant items or total score on the BADL in moderate disease or improvement or stabilisation in severe disease.
Reduction in aggressive behaviour that challenges and/or psychosis as evidenced by NPI improved scores of 2 or more in the relevant subscale over 6 months. An overall clinical global impression of stabilisation or improvement must be stated Discontinuation Criteria Discontinuation must be discussed first with the Consultant, carers, family, and with the patient wherever possible.
1) Adverse reaction to the medication 2) Lack of compliance with the medication lack of evidence of efficacy i.e. the patient does not fulfil the criteria for continuation stated above 3) Patient is on an end of life care pathway. 4) If the treatment is for cognitive problems predominantly a MOCA of <5/30 or SIB score of <30/100. GPs may wish to use any recognised cognitive tests (eg 6 item CIT) to determine cognitive decline and likely continued benefit of antidementia drug. 5) An irreversible deterioration in the patients global clinical presentation since the last review e.g., a CVA
An overall clinical global impression must state the treatment is no longer effective
This document will be reviewed in the light of new or emerging evidence or by October 4 2021 Doncaster & Bassetlaw Area Prescribing Committee October 2016 V7.0
6.0 PROCEDURE FOR ADOPTING SHARED CARE
Shared care [Amber] classification The specialist will send to the GP a diagnostic assessment report, a copy of the shared care protocol and a shared care referral specifying who is responsible for monitoring. Both the specialist and GP should sign the proforma with a record kept in the GP and Specialist records. Full details will be given of the prescribing regime (form, strength and dose of medication) and follow-up plan. The patient will be asked to make arrangements with their GP for continued supply.
7.0 REFERENCES
Personal Social Services Research Unit, London School of Economics and the Institute of Psychiatry. Dementia UK: a report into the prevalence and cost of Dementia. Alzheimer’s Society 2007 NICE Clinical Guidance 42: Dementia Supporting people with dementia and their carers in health and social care November 2006 updated 2016 Donepezil, galantamine, rivastigmine and memantine for the treatment of Alzheimer's disease (TA217) RDASH shared care agreement for Memantine 2014 Aricept (Donepezil) Summary of Product Characteristics Reminyl (Galantamine) Summary of Product Characteristics Exelon (Rivastigmine) Summary of Product Characteristics Ebixa (Memantine) Summary of Product Characteristics
8.0 SHARED CARE DEVELOPMENT
Written by: Rotherham Doncaster and South Humber Mental Health NHS Foundation Trust Doncaster Area Prescribing Committee September 2008
Reviewed by: Rotherham Doncaster and South Humber Mental Health NHS Foundation Trust Doncaster & Bassetlaw Area Prescribing Committee October 2016
This document will be reviewed in the light of new or emerging evidence or by October 5 2021