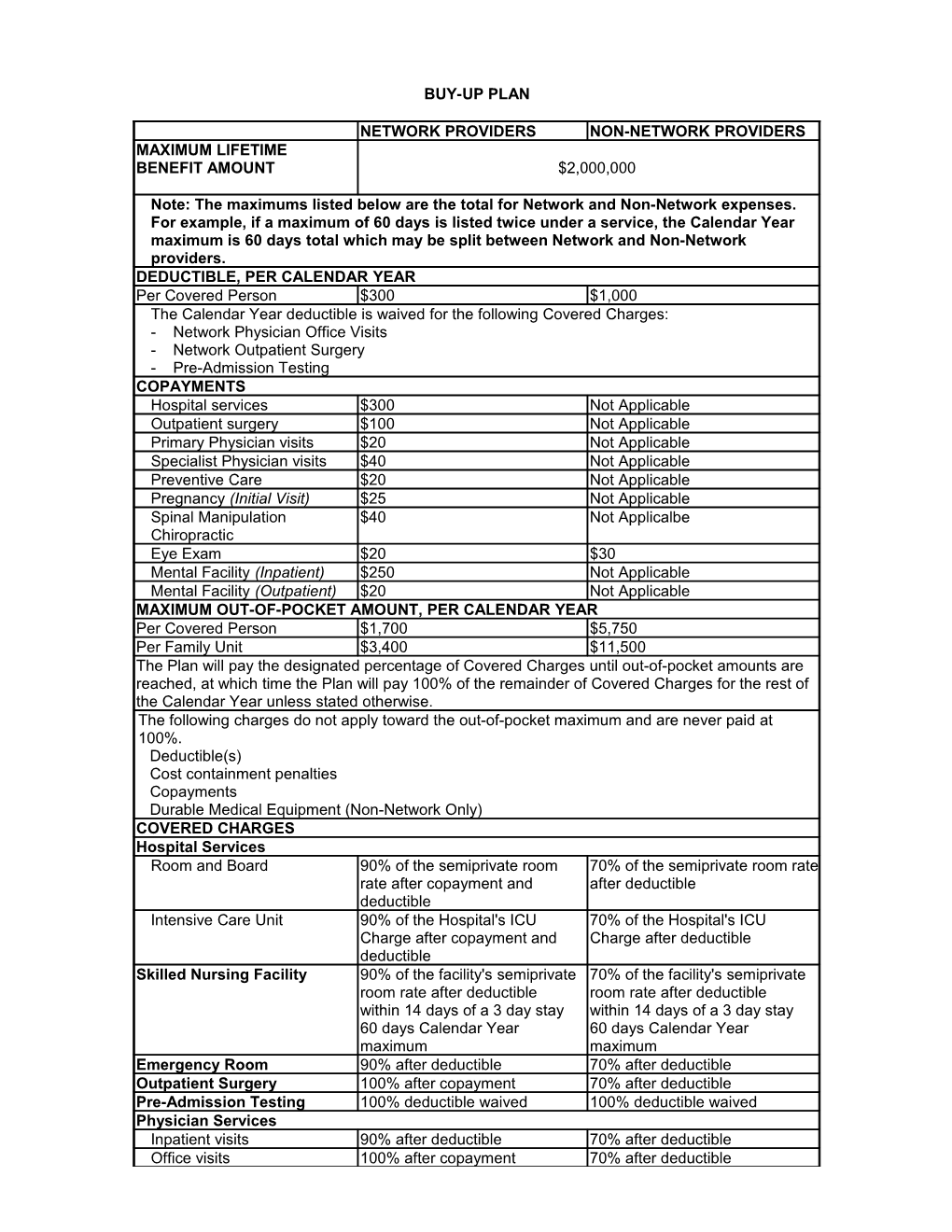
BUY-UP PLAN
NETWORK PROVIDERS NON-NETWORK PROVIDERS MAXIMUM LIFETIME BENEFIT AMOUNT $2,000,000
Note: The maximums listed below are the total for Network and Non-Network expenses. For example, if a maximum of 60 days is listed twice under a service, the Calendar Year maximum is 60 days total which may be split between Network and Non-Network providers. DEDUCTIBLE, PER CALENDAR YEAR Per Covered Person $300 $1,000 The Calendar Year deductible is waived for the following Covered Charges: - Network Physician Office Visits - Network Outpatient Surgery - Pre-Admission Testing COPAYMENTS Hospital services $300 Not Applicable Outpatient surgery $100 Not Applicable Primary Physician visits $20 Not Applicable Specialist Physician visits $40 Not Applicable Preventive Care $20 Not Applicable Pregnancy (Initial Visit) $25 Not Applicable Spinal Manipulation $40 Not Applicalbe Chiropractic Eye Exam $20 $30 Mental Facility (Inpatient) $250 Not Applicable Mental Facility (Outpatient) $20 Not Applicable MAXIMUM OUT-OF-POCKET AMOUNT, PER CALENDAR YEAR Per Covered Person $1,700 $5,750 Per Family Unit $3,400 $11,500 The Plan will pay the designated percentage of Covered Charges until out-of-pocket amounts are reached, at which time the Plan will pay 100% of the remainder of Covered Charges for the rest of the Calendar Year unless stated otherwise. The following charges do not apply toward the out-of-pocket maximum and are never paid at 100%. Deductible(s) Cost containment penalties Copayments Durable Medical Equipment (Non-Network Only) COVERED CHARGES Hospital Services Room and Board 90% of the semiprivate room 70% of the semiprivate room rate rate after copayment and after deductible deductible Intensive Care Unit 90% of the Hospital's ICU 70% of the Hospital's ICU Charge after copayment and Charge after deductible deductible Skilled Nursing Facility 90% of the facility's semiprivate 70% of the facility's semiprivate room rate after deductible room rate after deductible within 14 days of a 3 day stay within 14 days of a 3 day stay 60 days Calendar Year 60 days Calendar Year maximum maximum Emergency Room 90% after deductible 70% after deductible Outpatient Surgery 100% after copayment 70% after deductible Pre-Admission Testing 100% deductible waived 100% deductible waived Physician Services Inpatient visits 90% after deductible 70% after deductible Office visits 100% after copayment 70% after deductible NETWORK PROVIDERS NON-NETWORK PROVIDERS Surgery 90% after deductible 70% after deductible Allergy testing 90% after deductible 70% after deductible Allergy serum and injections 90% after deductible 70% after deductible Home Health Care 90% after deductible 70% after deductible 75 Calendar Year maximum 75 Calendar Year maximum Outpatient Private Duty 90% after deductible 70% after deductible Nursing 90 eight hour shifts Calendar 90 eight hour shifts Calendar Year maximum Year maximum Hospice Care 90% after deductible 70% after deductible 180 days inpatient and 180 days inpatient and outpatient outpatient Lifetime maximum Lifetime maximum Ambulance Service 90% after deductible 70% after deductible Occupational, Speech and 90% after deductible 70% after deductible Physical Therapy Durable Medical Equipment 80% after deductible 70% after deductible Prosthetics 80% after deductible 70% after deductible Orthotics 80% after deductible 70% after deductible Spinal Manipulation 100% after copayment 70% after deductible Chiropractic 20 visits limited to $30 per visit Calendar Year maximum Nutritional Education/ 90% after deductible 70% after deductible Therapy for Diabetes Other Eligible Expenses 90% after deductible 70% after deductible Mental Disorders & Substance Abuse (Combined) Inpatient 90% after copayment and 70% after deductible deductible 45 days Calendar Year 45 days Calendar Year maximum maximum Outpatient 100% after copayment 50% after deductible 52 visits Calendar Year 52 visits Calendar Year maximum maximum Preventive Care Routine Well Adult Care 100% after copayment 70% after deductible Includes: office visits, pap smear, mammogram, prostate screening, gynecological exam, routine physical examination, x-rays, laboratory blood tests, immunizations/flu shots (excluding foreign travel immunizations), routine eye examination and colonoscopy. Inpatient Routine Well 90% after deductible 70% after deductible Newborn Care Routine Well Child Care 100% after copayment 70% after deductible Includes: office visits, routine physical examination (including sports exam), pap smear, gynecological exam, laboratory blood tests, x-rays and immunizations/Flu shots. Organ Transplants Inpatient 90% after copayment and 70% after deductible deductible Outpatient 90% after deductible 70% after deductible Pregnancy Initial Visit 100% after copayment 70% after deductible Delivery Charge 90% after deductible 70% after deductible Facility Charge 90% after copayment and 70% after deductible deductible Dependent daughters’ pregnancy not covered. CORE PLAN
NETWORK PROVIDERS NON-NETWORK PROVIDERS MAXIMUM LIFETIME BENEFIT AMOUNT $2,000,000
Note: The maximums listed below are the total for Network and Non-Network expenses. For example, if a maximum of 60 days is listed twice under a service, the Calendar Year maximum is 60 days total which may be split between Network and Non-Network providers. DEDUCTIBLE, PER CALENDAR YEAR Per Covered Person $500 $1,500 The Calendar Year deductible is waived for the following Covered Charges: - Network Physician Office Visits - Network Outpatient Surgery - Pre-Admission Testing COPAYMENTS Hospital services $200 Not Applicable Primary Physician visits $25 Not Applicable Specialist Physician visits $50 Not Applicable Preventive Care $25 Not Applicable Pregnancy (Initial Visit) $25 Not Applicable Spinal Manipulation $50 Not Applicalbe Chiropractic Eye Exam $25 $30 Mental Facility (Inpatient) $250 Not Applicable Mental Facility (Outpatient) $25 Not Applicable MAXIMUM OUT-OF-POCKET AMOUNT, PER CALENDAR YEAR Per Covered Person $2,500 $5,750 Per Family Unit $5,000 $11,500 The Plan will pay the designated percentage of Covered Charges until out-of-pocket amounts are reached, at which time the Plan will pay 100% of the remainder of Covered Charges for the rest of the Calendar Year unless stated otherwise. The following charges do not apply toward the out-of-pocket maximum and are never paid at 100%. Deductible(s) Cost containment penalties Copayments Durable Medical Equipment (Non-Network Only) COVERED CHARGES Hospital Services Room and Board 80% of the semiprivate room 60% of the semiprivate room rate rate after copayment and after deductible deductible Intensive Care Unit 80% of the Hospital's ICU 60% of the Hospital's ICU Charge after copayment and Charge after deductible deductible Skilled Nursing Facility 80% of the facility's semiprivate 60% of the facility's semiprivate room rate after deductible room rate after deductible within 14 days of a 3 day stay within 14 days of a 3 day stay 60 days Calendar Year 60 days Calendar Year maximum maximum Emergency Room 80% after deductible 60% after deductible Outpatient Surgery 80% after deductible 60% after deductible Pre-Admission Testing 100% deductible waived 100% deductible waived Physician Services Inpatient visits 80% after deductible 60% after deductible Office visits 100% after copayment 60% after deductible Surgery 80% after deductible 60% after deductible NETWORK PROVIDERS NON-NETWORK PROVIDERS Allergy testing 80% after deductible 60% after deductible Allergy serum and injections 80% after deductible 60% after deductible Home Health Care 80% after deductible 60% after deductible 75 Calendar Year maximum 75 Calendar Year maximum Outpatient Private Duty 80% after deductible 60% after deductible Nursing 90 eight hour shifts Calendar 90 eight hour shifts Calendar Year maximum Year maximum Hospice Care 80% after deductible 60% after deductible 180 days inpatient and 180 days inpatient and outpatient outpatient Lifetime maximum Lifetime maximum Ambulance Service 80% after deductible 60% after deductible Occupational, Speech and 80% after deductible 60% after deductible Physical Therapy Durable Medical Equipment 80% after deductible 60% after deductible Prosthetics 80% after deductible 60% after deductible Orthotics 80% after deductible 60% after deductible Spinal Manipulation 100% after copayment 60% after deductible Chiropractic 20 visits limited to $30 per visit Calendar Year maximum Nutritional Education/ 80% after deductible 60% after deductible Therapy for Diabetes Other Eligible Expenses 80% after deductible 60% after deductible Mental Disorders & Substance Abuse (Combined) Inpatient 80% after copayment and 60% after deductible deductible 45 days Calendar Year 45 days Calendar Year maximum maximum Outpatient 100% after copayment 50% after deductible 52 visits Calendar Year 52 visits Calendar Year maximum maximum Preventive Care Routine Well Adult Care 100% after copayment 60% after deductible Includes: office visits, pap smear, mammogram, prostate screening, gynecological exam, routine physical examination, x-rays, laboratory blood tests, immunizations/flu shots (excluding foreign travel immunizations), routine eye examination and colonoscopy. Inpatient Routine Well 80% after deductible 60% after deductible Newborn Care Routine Well Child Care 100% after copayment 60% after deductible Includes: office visits, routine physical examination (including sports exam), pap smear, gynecological exam, laboratory blood tests, x-rays and immunizations/flu shots. Organ Transplants Inpatient 80% after copayment and 60% after deductible deductible Outpatient 80% after deductible 60% after deductible Pregnancy Initial Visit 100% after copayment 60% after deductible Delivery Charge 80% after deductible 60% after deductible Facility Charge 80% after copayment and 60% after deductible deductible Dependent daughters’ pregnancy not covered. OUT-OF-AREA PLAN
NETWORK PROVIDERS NON-NETWORK PROVIDERS MAXIMUM LIFETIME BENEFIT AMOUNT $2,000,000
DEDUCTIBLE, PER CALENDAR YEAR Per Covered Person $250 Per Family 3 Participants The Calendar Year deductible is waived for the following Covered Charges: - Pre-Admission Testing - Routine Well Adult Care MAXIMUM OUT-OF-POCKET AMOUNT, PER CALENDAR YEAR Per Covered Person $3,000 Per Family Unit $5,000 The Plan will pay the designated percentage of Covered Charges until out-of-pocket amounts are reached, at which time the Plan will pay 100% of the remainder of Covered Charges for the rest of the Calendar Year unless stated otherwise. The following charges do not apply toward the out-of-pocket maximum and are never paid at 100%. Deductible(s) Cost containment penalties Outpatient Substance Abuse COVERED CHARGES Hospital Services Room and Board 80% of the semiprivate room rate after deductible Intensive Care Unit 80% of the Hospital's ICU Charge after deductible Skilled Nursing Facility 80% of the facility's semiprivate room rate after deductible within 14 days of a 3 day stay 60 days Calendar Year maximum Emergency Room 80% after deductible Outpatient Surgery 80% after deductible Pre-Admission Testing 100% deductible waived Physician Services Inpatient visits 80% after deductible Office visits 80% after deductible Surgery 80% after deductible Allergy testing 80% after deductible Allergy serum and injections 80% after deductible Home Health Care 80% after deductible 75 Calendar Year maximum Outpatient Private Duty 80% after deductible Nursing 90 eight hour shifts Calendar Year maximum Hospice Care 80% after deductible 180 days inpatient and outpatient Lifetime maximum Ambulance Service 80% after deductible Occupational, Speech and 80% after deductible Physical Therapy Durable Medical Equipment 80% after deductible Prosthetics 80% after deductible Orthotics 80% after deductible Spinal Manipulation 80% after deductible Chiropractic Nutritional 80% after deductible Education/Therapy for Diabetes Other Eligible Expenses 80% after deductible NETWORK PROVIDERS NON-NETWORK PROVIDERS Mental Disorders & Substance Abuse (Combined) Inpatient 80% after deductible 45 days Calendar Year maximum Outpatient 50% after deductible 52 visits Calendar Year maximum Preventive Care Routine Well Adult Care 80% deductible waived Includes: office visits, pap smear, mammogram, prostate screening, gynecological exam, routine physical examination, x-rays, laboratory blood tests, immunizations/flu shots (excluding foreign travel immunizations), routine eye examination and colonoscopy. Inpatient Routine Well 80% after deductible Newborn Care Routine Well Child Care 80% after deductible Includes: office visits, routine physical examination (including sports exam), pap smear, gynecological exam, laboratory blood tests, x-rays and immunizations/flu shots. Organ Transplants Inpatient 80% after deductible Outpatient 80% after deductible Pregnancy Initial Visit 80% after deductible Delivery Charge 80% after deductible Facility Charge 80% after deductible Dependent daughters’ pregnancy not covered. PRESCRIPTION DRUG BENEFIT
Calendar Year Deductible
Per Individual...... $50 Per Family...... $100
Retail Network Pharmacy (30 Day Supply)*mail-order rates will apply after fourth fill (original plus three refills) Generic Copayment...... $10 Preferred Brand Copayment...... $25 Non-Preferred Copayment...... $40
Retail Non-Network Pharmacy (30 Day Supply)
Generic 70% after deductible
Preferred Brand 70% after deductible
Non-Preferred 70% after deductible
Mail Order Prescription Drug (90 Day Supply) Generic Copayment...... $25 Preferred Brand Copayment...... $65 Non-Preferred Brand Copayment...... $100
*Penalty Maintenance – after the fourth fill at retail pharmacy, mail-order rates will apply for a 30-day supply.