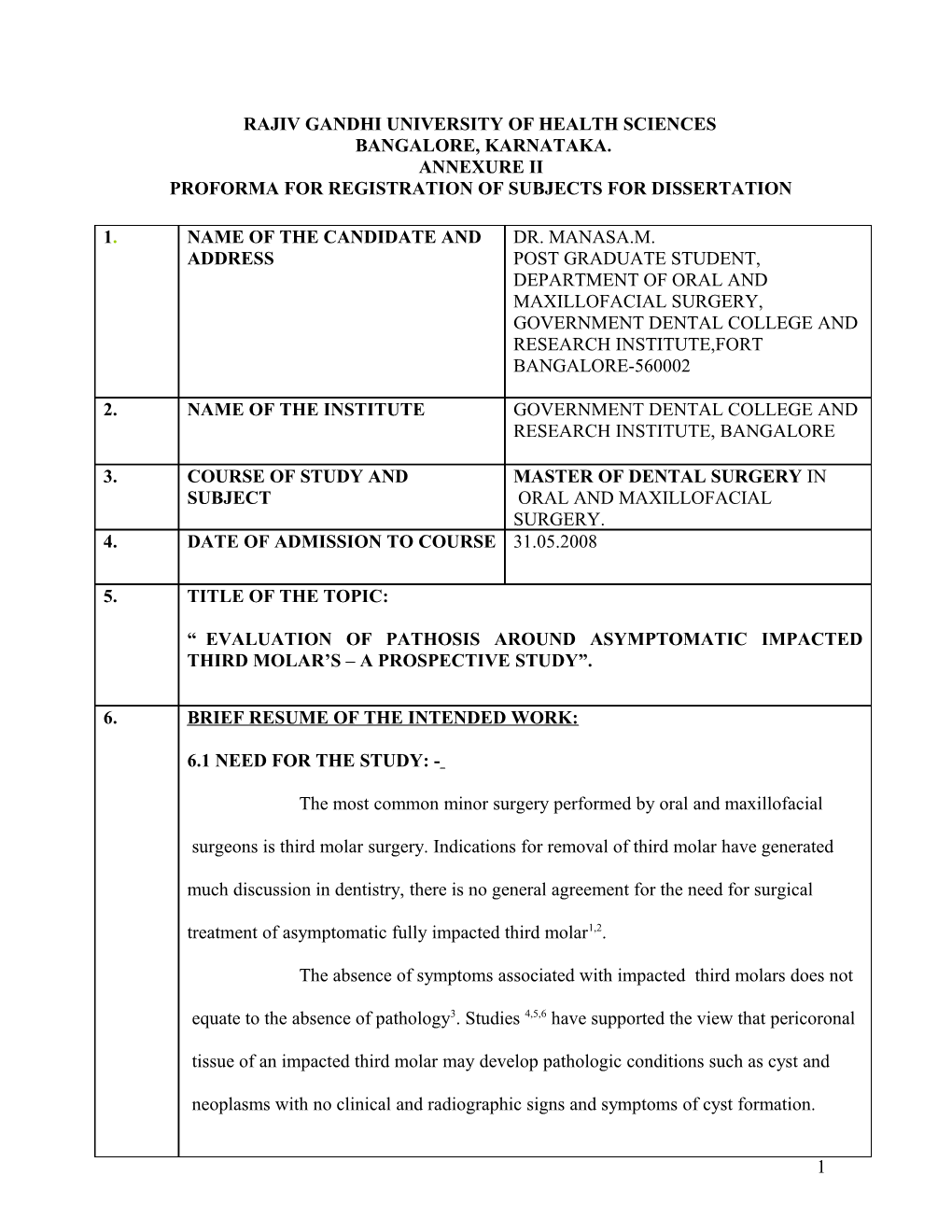
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES BANGALORE, KARNATAKA. ANNEXURE II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. NAME OF THE CANDIDATE AND DR. MANASA.M. ADDRESS POST GRADUATE STUDENT, DEPARTMENT OF ORAL AND MAXILLOFACIAL SURGERY, GOVERNMENT DENTAL COLLEGE AND RESEARCH INSTITUTE,FORT BANGALORE-560002
2. NAME OF THE INSTITUTE GOVERNMENT DENTAL COLLEGE AND RESEARCH INSTITUTE, BANGALORE
3. COURSE OF STUDY AND MASTER OF DENTAL SURGERY IN SUBJECT ORAL AND MAXILLOFACIAL SURGERY. 4. DATE OF ADMISSION TO COURSE 31.05.2008
5. TITLE OF THE TOPIC:
“ EVALUATION OF PATHOSIS AROUND ASYMPTOMATIC IMPACTED THIRD MOLAR’S – A PROSPECTIVE STUDY”.
6. BRIEF RESUME OF THE INTENDED WORK:
6.1 NEED FOR THE STUDY: -
The most common minor surgery performed by oral and maxillofacial
surgeons is third molar surgery. Indications for removal of third molar have generated
much discussion in dentistry, there is no general agreement for the need for surgical
treatment of asymptomatic fully impacted third molar1,2.
The absence of symptoms associated with impacted third molars does not
equate to the absence of pathology3. Studies 4,5,6 have supported the view that pericoronal
tissue of an impacted third molar may develop pathologic conditions such as cyst and
neoplasms with no clinical and radiographic signs and symptoms of cyst formation.
1 The aim of this prospective study is to evaluate the pathosis around asymptomatic impacted
third molar.
6.2 REVIEW OF LITERATURE:
1. Ninety-six dental follicle were collected from third molar teeth of 63 patients. No tooth had a follicular space greater than 2.4mm as measured on the panoramic radiograph. Specimens were examined histopathologically and diagnosis of dentigerous cysts was made in 31 cases,22 of 60 mandibular specimens(37%) and nine of 36 maxillary specimens(25%) were affected.
2. In a retrospective analysis of 9994 impacted third molars, removed in 7582 patients formed the basis of this study. The analysis revealed 231 cysts(2.31%) and 79 tumors(0.79%) including 7 benign tumors(0.77%) and 2 malignant tumors (0.02%) . Thus concluded the incidence of cysts and tumors around impacted third molars was 3.10%.
3. One hundred impacted third molars without evidence of abnormal pericoronal radiolucency( follicular space<2.0mm) were removed, pericoronal tissues were submitted to histopathologic examination. Of the specimens submitted,34% showed squamous metaplasia suggestive of cystic change equivalent to that found in dentigerous cysts and concluded that the incidence of soft tissue pathologic condition is higher than generally assumed from radiographic examination alone.
4. A clinical study on 94 patients, follicular spaces were measured from panoramic radiographs by each author independently, pericoronal tissues of radiographically normal impacted third molar’s were examined histopathologically. 47(50%) of them showed cystic changes. Ages of these patients ranged from 14 to 44 years (mean=22.19) but most of the cystic changes occurred in the 20-25 year age range. Results concluded that cystic changes may be encountered in the histopathological examination of asymptomatic third molar’s, especially in patients older than 20yrs. Vertically positioned impacted third molar may be suspected as higher possibility of cystic changes.
5. In a histopathological study of 120 impacted third molar dental follicles, results showed that pathological conditions were found in 23%, mostly in women who were more than 20yrs of age and concluded that asymptomatic impacted third molars should be removed before pathological changes can occur.
6. A study of 100 patients who had radiographically normal asymptomatic impacted lower third molar (<2.4mm radiolucency). The incidence of cystic changes in dental follicle was 46%. There was a high incidence in the right side and in men.
2 6.3 AIM AND OBJECTIVES OF THE STUDY: -
The aim of the study is to evaluate the pathosis around asymptomatic impacted third molar.
OBJECTIVES:-
1. To determine whether impacted third molars increase the incidence of pathological conditions.
2. The secondary purpose is to determine the frequency and type of cysts and tumors around impacted third molar.
3. To determine whether any particular type of impaction increases the occurrence of cysts and tumors.
4. To determine whether impacted third molar has any sex predilection for occurrence of cysts and tumors.
MATERIALS AND METHODS : -
7.1 SOURCES OF THE DATA.
Patients visiting the Department of Oral and Maxillofacial Surgery, Government Dental college and Research Institute , Bangalore.
7.2 METHODS OF COLLECTION OF DATA.
This is a prospective study, patients are selected randomly who are undergoing extraction of the impacted maxillary or mandibular third molar’s whose general and systemic conditions are evaluated to know their fitness for extraction(sample size-100).
INCLUSION CRITERIA: -
1. Patients with asymptomatic impacted third molar willing to undergo extraction.
2. Impacted third molar completely covered by soft tissue.
3 EXCLUSION CRITERIA: -
1. Medically compromised patients.
2. Patients with impacted third molar with established pathosis or symptomatic impacted third molar.
3. If the Impacted tooth lies in an area in which its removal may seriously jeopardize adjascent nerves, teeth or previously constructed prosthodontic bridges.
4. If Impacted tooth lies in an area of previously irradiated bone.
5. Partially or completely erupted impacted third molar.
PROCEDURE:
Impacted third molar (maxillary or mandibular) which are asymptomatic are considered for extraction.
Impacted teeth are classified according to WINTER;
1. Mesioangular. 2. Horizontal. 3. Vertical. 4. Distoangular.
Extraction is carried out by raising a mucoperiosteal flap and using a technique depending on the type of impaction.
After extracting the tooth, dental follicle and surrounding tissues is sent for histopathological examination
Data will be tabulated statistically by using chi-square test and student t test.
4 7.3 Does the study require any investigations or interventions to be conducted on patients or other humans or animals?
YES
7.4 Has ethical clearance been obtained from your institution in case of 7.3?
NOT REQUIRED
LIST OF REFERENCES:
8. 1. John Adelsperger,DDS,a John H. Campbell,DDS,MS,b David B. Coates,DDS,c Don-John Summerlin,DMD,MS,d and Charles E. Tomich,DDS,MSDe. Early soft tissue pathosis associated with impacted third molars without pericoronal radiolucency: Oral surgery, Oral medicine, Oral pathology, Oral radiology 2000 ;89:402-6.
2. O. Guven, A. Keskin, U.K.Akal; Incidence of cysts and tumors around impacted third molars. International journal of oral and maxillofacial surgery 2000;29:131-135.
3. Gulsun Yildirim,DDS,PhD,a Hanife Ataoglu,DDS,PhD,b Ahmet Mihmanli, DDS.PhD,c Dilek Kiziloglu,DDS,d and Mustafa Cihat Avunduk,DDS,MDe. Pathologic changes in soft tissue associated with asymptomatic impacted third molars: Oral surgery, Oral medicine, Oral pathology, Oral radiology 2008;106:14-8.
4. Timucin Baykul,DDS,PhD,a Ali A. Saglam,DDS.PhD,b Ulkem Aydin,DDS,PhD,c and Kayhan Basak,MDd. Incidence of cystic changes in radiographically normal impacted lower third molar follicles: Oral surgery, Oral medicine, Oral pathology, Oral radiology 2005;99:542-5.
5. J.W. Glosser, J.H. Campbell. Pathologic change in soft tissues associated with radiographically ‘normal’ third molar impactions: British journal of oral and maxillofacial surgery 1999;37:259-260.
6. G.H.L. Saravanaa, Krishnaraj Subhashrajb. Cystic changes in dental follicle associated with radiographically normal impacted mandibular third molar: British journal of oral and maxillofacial surgery 2008;46:552-553.
5 9. SIGNATURE OF THE CANDIDATE
10. REMARKS OF THE GUIDE
11 NAME AND DESIGNATION OF DR.GIRISH GIRADDI. PROFESSOR AND HEAD, 11.1 GUIDE DEPARTMENT OF ORAL AND MAXILLOFACIAL SURGERY, GOVT. DENTAL COLLEGE AND RESEARCH INSTITUTE, BANGALORE.
11.2 SIGNATURE
11.3 CO-GUIDE DR. S. HEMAVATHY. PROFESSOR AND HEAD, DEPARTMENT OF ORAL PATHOLOGY, GOVT. DENTAL COLLEGE AND RESEARCH INSTITUTE, BANGALORE.
11.4 SIGNATURE
6
11.5 HEAD OF THE DEPARTMENT DR. GIRISH GIRADDI. PROFESSOR AND HEAD, DEPARTMENT OF ORAL AND MAXILLOFACIAL SURGERY, GOVT. DENTAL COLLEGE AND RESEARCH INSTITUTE, BANGALORE.
11.6 SIGNATURE
12. 12.1 REMARK OF THE CHAIRMAN AND PRINCIPAL
12.2 SIGNATURE
7