Clinical Order Set Orthopaedic Hip Fracture Post-Op Orders Elder friendly – if patient 75 years or olderPage 1 of 7 Key: Req – Requisition MAR – Medication Administration Record K – Kardex Dis – Discontinued P – Drug ProfileKEY Demographics
Admit to Orthopaedics MRP is ______
Code Status: Full Code No-CPR see further written orders regarding CPR/DNR MRP to determine
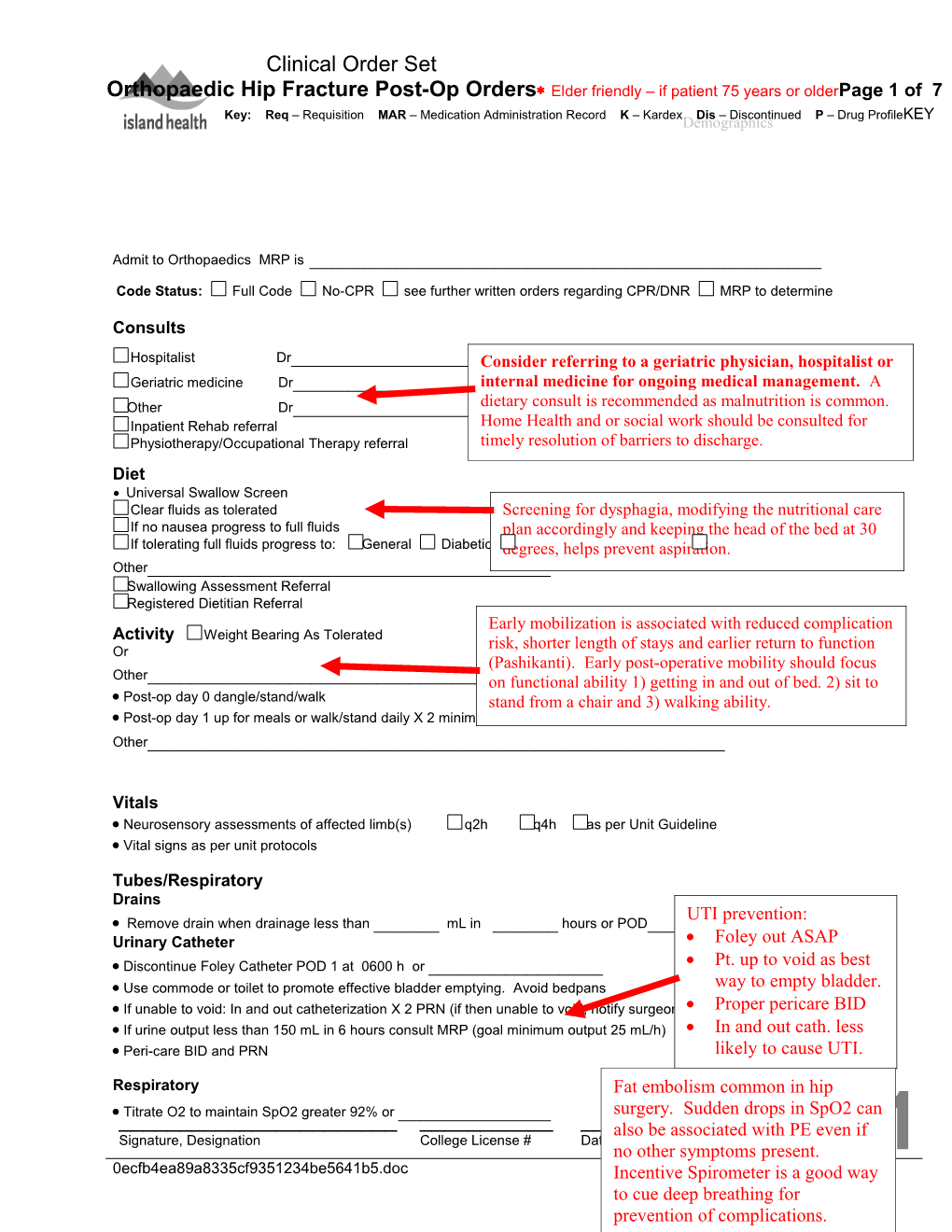
Consults Hospitalist Dr______Consider referring to a geriatric physician, aware____ hospitalist or Geriatric medicine Dr______internal medicine for ongoing medical aware management.____ A Other Dr______dietary consult is recommended as malnutrition aware____ is common. Inpatient Rehab referral Home Health and or social work should be consulted for Physiotherapy/Occupational Therapy referral timely resolution of barriers to discharge. Diet Universal Swallow Screen Clear fluids as tolerated Screening for dysphagia, modifying the nutritional care If no nausea progress to full fluids plan accordingly and keeping the head of the bed at 30 If tolerating full fluids progress to: General Diabetic degrees, High Protein, helps Highprevent Calorie aspiration. High Fibre Other______Swallowing Assessment Referral Registered Dietitian Referral Early mobilization is associated with reduced complication Activity Weight Bearing As Tolerated risk, shorter length of stays and earlier return to function Or (Pashikanti). Early post-operative mobility should focus Other______on functional ability 1) getting in and out of bed. 2) sit to Post-op day 0 dangle/stand/walk stand from a chair and 3) walking ability. Post-op day 1 up for meals or walk/stand daily X 2 minimum Other______
Vitals Neurosensory assessments of affected limb(s) q2h q4h as per Unit Guideline Vital signs as per unit protocols
Tubes/Respiratory Drains UTI prevention: Remove drain when drainage less than ______mL in ______hours or POD_____ Urinary Catheter Foley out ASAP Discontinue Foley Catheter POD 1 at 0600 h or ______ Pt. up to void as best Use commode or toilet to promote effective bladder emptying. Avoid bedpans way to empty bladder. If unable to void: In and out catheterization X 2 PRN (if then unable to void, notify surgeon) Proper pericare BID If urine output less than 150 mL in 6 hours consult MRP (goal minimum output 25 mL/h) In and out cath. less Peri-care BID and PRN likely to cause UTI.
Respiratory Fat embolism common in hip Titrate O2 to maintain SpO2 greater 92% or ______surgery. Sudden drops in SpO2 can ______also be associated______with PE even if Signature, Designation College License # Date Time Page 1/ 7 no other symptoms present. 1 0ecfb4ea89a8335cf9351234be5641b5.doc IncentiveC/8/OrthHipFracture/MD/03-15/V1/Post-op Spirometer is a good way to cue deep breathing for prevention of complications. Clinical Order Set Orthopaedic Hip Fracture Post-Op Orders Elder friendly – if patient 75 years or olderPage 1 of 7 Key: Req – Requisition MAR – Medication Administration Record K – Kardex Dis – Discontinued P – Drug ProfileKEY Demographics
Incentive spirometer q1h while awake
Wound Management
Orthopaedic dressing as per unit guidelines Hip fracture patients are at high risk for Remove clips/staples in days ______anaemia, impaired renal function, Investigations diabetes, malnutrition and cardiac events. Low haemoglobin, and high Hematology profile: Day 1 and 3 serum creatinine are predictors of Sodium, potassium, chloride, carbon dioxide total, creatinine, eGFR: Day 1 and 3 mortality. Electrolyte disturbances are Phosphorus, magnesium Day 1 common due to dehydration.
INR Day_____
Calcium, phosphorus, albumin, protein, alkaline phosphatase, TSH
Other______
Medical Imaging
X-ray ______POD______
IV Fluids IV fluids and rates must be carefully Solution considered as the hip fracture patient is susceptible to electrolyte 0.9% sodium chloride imbalance, dehydration and CHF. It’s 2/3 + 1/3 a fine like to walk.
D5W + 0.45% sodium chloride
D5W and 0.9% sodium chloride
Ringer’s Lactate
Additive KCl 20 mmol/L
Rate 75 mL/h 125 mL/h 100 mL/h 150mL/h Or ______mL/h
Bolus 500 mL Ringer’s Lactate over 90 minutes X 1 PRN when urine output less than 30mL/h for 2h and if no increase in urine output notify surgeon ______Bolus 500 mL 0.9% sodium chloride over 90 minutes______X 1 PRN when urine______output less than 30mL/h______for 2h and if Signature, Designation College License # Date Time Page 1/ 7 1 0ecfb4ea89a8335cf9351234be5641b5.doc C/8/OrthHipFracture/MD/03-15/V1/Post-op Clinical Order Set Orthopaedic Hip Fracture Post-Op Orders Elder friendly – if patient 75 years or olderPage 1 of 7 Key: Req – Requisition MAR – Medication Administration Record K – Kardex Dis – Discontinued P – Drug ProfileKEY Demographics
no increase in urine output notify surgeon IV to infusor/saline lock when tolerating fluids; discontinue when IV access no longer required
Antibiotic Prophylaxis The newest best practice standards ceFAZolin 2g IV q8h X 2 doses. Start 8h after pre-op dose reflect higher antibiotic doses preop and For patients with severe beta-lactam (penicillin/cephalosporin) allergy eg. anaphylaxis,fewer doses angioedema postop than previously clindamycin 900 mg IV q8h x 2 doses. Start 8 hours after pre-op dose recommended. Or vancomycin 1 g IV to be given 12h after pre-op dose. Infuse over 1h
Bowel Management Ensure fluids/adequate hydration within prescribed limits; frequent/encourage mobility within prescribed limits, regular bowel routine Acute care: Bowel Intervention – Adult Proactive bowel management is recommended to prevent constipation as the patient is at high risk due to opioids, if NPO:______dehydration and immobility.
RN, RPN and/or Pharmacist to complete thorough assessment of bowel function including review of Pre-Hospital Functional Screening Tool to determine if regularly scheduled laxatives are required Laxatives as indicated RN, RPN and/or Pharmacist based on assessment above and Best Possible Medication History Contact MRP to discuss docusate 100 mg PO BID; hold if patient develops diarrhea. Reassess need for docusate
Delirium CAM assessment Q shift If CAM positive, notify MD to investigate/ address underlying cause within 12 hrs CAM = Delirious if both 1 and 2 and either 3 or 4 checked Medication orders only for persistent agitation with risk of harm or injury 1. Acute onset and fluctuating course Notify MD if agitation medication given and document 2. Inattention QUEtiapine 6.25 mg to 12.5 mg PO Q4h PRN to a maximum3. of 18.75Disorganized mg in 24h thinking loxapine 2.5 to 5 mg q2h PO PRN to a maximum of 10 mg4. in 24h Altered level of consciousness If unable to use oral route give Up to 40% of hip fracture patients experience delirium. We loxapine 2.5 to 5 mg q2h subcutaneously PRN to a maximumneed of to 10 recognize mg in 24h and treat in a timely manner.
Insomnia Quetiapine is a new generation antipsychotic zopiclone 3.75 mg PO at bedtime as required for sleep and is the first line medication as it has a lower If patient has been taking another sleeping pill regularly, continue the same:side______effect profile than traditional antipsychotics. Quetiapine is dopamine sparing Diabetes Management and therefore a better choice for patients with Follow either IV or Subcut Insulin Order Set – MRP to complete Lewy Body Dementia and Parkinsons. Other______Signature, Designation College License # Date Time Page 1/ 7 1 0ecfb4ea89a8335cf9351234be5641b5.doc C/8/OrthHipFracture/MD/03-15/V1/Post-op Clinical Order Set Orthopaedic Hip Fracture Post-Op Orders Elder friendly – if patient 75 years or olderPage 1 of 7 Key: Req – Requisition MAR – Medication Administration Record K – Kardex Dis – Discontinued P – Drug ProfileKEY Demographics
The routine use of HS sedation is not recommended. If the patient was regularly taking a benzodiazepine for sleep prior to this fracture, it may be necessary to continue it in hospital to avoid withdrawal. Sedation is a leading cause of falls.
*** Systemic narcotics or other CNS depressants ordered by Anesthesiologist take precedence over those ordered by surgeon *** Pain and Nausea Management Pain acetaminophen 650 mg PO or RECTAL suppository QID to a max of 4,000 mg per 24 hours Other: ______***Do not use IV/subcutaneous and PO simultaneously*** Regular administration of low dose opioid titrated to HYDROmorphone 0.5 mg PO q4h Or effect with break through doses is the recommended HYDROmorphone 1 mg PO q4h standard of care. Relying on frail older patients, many with For patients unable to tolerate oral route cognitive impairment, to request pain medication results in HYDROmorphone 0.25 mg subcutaneously q4h under treatment and poor pain management. Poor pain Or management is a serious stressor leading to immobility, HYDROmorphone 0.5mg subcutaneously q4h delirium and long term functional impairment.
Hold opioid dose if frequently drowsy (or per sedation scale) May hold opioid if sleeping
Breakthrough pain HYDROmorphone 0.5 to 1 mg PO Q2h PRN Or for patients unable to tolerate oral route Ondansetron is recommended as the first line HYDROmorphone 0.25 to 0.5 mg subcutaneously Q2h PRN antiemetic as it is well tolerated and efficacious. Dimenhydrinate or prochlorperazine are not Nausea and Vomiting ondansetron 4 mg IV/PO Q8h PRN recommended as these drugs are highly anticholinergic metoclopramide 5 to 10 mg IV/PO Q6h PRN if ondansetron ineffectiveand increase the risk of delirium and sedation in older Other______adults.
VTE Prophylaxis (See Page 6 ) Mechanical method can be combined with anticoagulant in very high risk patients Or used alone in patients with a high risk for bleeding Anticoagulation not to start any earlier than 8h post-operatively ______No Anticoagulation required ______(reason) Signature, Designation College License # Date Time Page 1/ 7 1 0ecfb4ea89a8335cf9351234be5641b5.doc C/8/OrthHipFracture/MD/03-15/V1/Post-op Clinical Order Set Orthopaedic Hip Fracture Post-Op Orders Elder friendly – if patient 75 years or olderPage 1 of 7 Key: Req – Requisition MAR – Medication Administration Record K – Kardex Dis – Discontinued P – Drug ProfileKEY Demographics
dalteparin 5,000 units subcut q24h Patients less than 40 kg or age greater than 85 years Give first dose at ______dalteparin 2,500 units subcut q24h (time/date)
Other______Mechanical: Specify______Other______VTE prophylaxis is usually required post-op for hip fracture patients. The natural response to surgery is increased clotting. Early mobilization will also help prevent VTE in conjunction with anticoagulants. Be on the look-out for PE as well Vitamin and Mineral Supplements cholecalciferol(Vitamin D3) 2,000 units PO daily Hip# patients are commonly vitamin deficient. multivitamin PO daily: 1 tablet 5 mL liquid(RN:Vit Indicate D3 and which Calcium prep) supplementation has been calcium carbonate 1250 mg PO daily associated with both increasing bone density ferrous fumarate 300 mg (99 mg elemental iron) PO dailyand fallsstarting prevention. POD 5 Iron supplementation is Increase ferrous fumarate 300 mg (99 mg elemental iron) to BID POD 10 Or frequently necessary to promote hemoglobin production. ferrous sulphate liquid – 300 mg (60 mg elemental iron) PO daily starting POD 5.
Increase ferrous sulphate liquid – 300 mg (60 mg elemental iron) to BID POD 10
Discharge
Patient may be discharged when meets unit criteria or as per physicians order
Follow up in ______weeks post-op with Surgeon’s office or Fracture/Cast Clinic
Follow-up out-patient physiotherapy as appropriate
Follow-up Island Osteoporosis Clinic OT/PT to arrange home safety assessment PT to assess & prescribe home exercise program and fall prevention in the community
Patients will require individualized Additional Orders assessment for osteoporosis and should be ______referred to a clinic or their physician to ensure this risk is addressed. ______All patients are at risk for falls and require individualized risk ______assessment with patient and family education. Home environment ______assessment with______a Home OT/PT should______be considered. ______A physiotherapist Signature, Designation could prescribeCollege and teach License home # exercisesDate to improve strengthTime and Page 1/ 7 1 0ecfb4ea89a8335cf9351234be5641b5.docbalance as well as identifying an appropriate communityC/8/OrthHipFracture/MD/03-15/V1/Post-op based fall prevention and or exercise program. Check out the FReSH START booklet for useful information throughout the patient stay. Clinical Order Set Orthopaedic Hip Fracture Post-Op Orders Elder friendly – if patient 75 years or olderPage 1 of 7 Key: Req – Requisition MAR – Medication Administration Record K – Kardex Dis – Discontinued P – Drug ProfileKEY Demographics
______
Information provided by the Provincial Hip Fracture Redesign Project best practice focus group.
John Kristiansen for Island Health
______Signature, Designation College License # Date Time Page 1/ 7 1 0ecfb4ea89a8335cf9351234be5641b5.doc C/8/OrthHipFracture/MD/03-15/V1/Post-op Step One assess all patients admitted to hospital for level of mobility (tick one box). All surgical patients and all medical patients with significantly reduced mobility, should be considered for further risk assessment Step Two review patient-related factors against thrombosis risk, ticking each box that applies (more than one box can be ticked) any tick for thrombosis risk should prompt thromboprophylaxis according to NICE guidance. Risk factors identified are not exhaustive. Clinicians may consider additional risks in individual patients and offer thromboprophylaxis as appropriate Step Three review the patient-related factors against bleeding risk and tick each box that applies (more than one box can be ticked) any tick should prompt clinical staff to consider if bleeding risk is sufficient to preclude pharmacological intervention Balancing risk/benefit is at the discretion of the ordering physician Mobility – all patients Tick Tick Tick (tick one box) Surgical patient Medical patient expected to have Medical patient NOT expected to ongoing reduced mobility relative have significantly reduced mobility to normal state relative to normal state Assess for thrombosis and bleeding risk below Risk assessment now complete Thrombosis Risk Patient related Tick Admission related Tick Active cancer or cancer treatment Significantly reduced mobility for 3 days or more Age greater than 60 Hip or knee replacement Dehydration Hip fracture Known thrombophilias Total anaesthetic + surgical time greater than 90 min Surgery involving pelvis or lower limb with a total Obesity (BMI greater than 30 kg/m2) anaesthetic + surgical time greater than 60 minutes One or more significant medical comorbidities (eg heart disease; metabolic, endocrine or respiratory Acute surgical admission with inflammatory or pathologies; acute infectious diseases; inflammatory intra-abdominal condition conditions) Personal history or first-degree relative with a history of Critical care admission VTE Use of hormone replacement therapy Surgery with significant reduction in mobility Use of estrogen-containing contraceptive therapy Varicose veins with phlebitis Pregnancy or less than 6 weeks post partum (see NICE guidance for specific risk factors) Bleeding Risk Patient related Tick Admission related Tick Active bleeding Neurosurgery, spinal surgery or eye surgery Acquired bleeding disorders (such as acute liver failure) Other procedure with high bleeding risk Concurrent use of anticoagulants known to increase risk Lumbar puncture/epidural/spinal anaesthesia expected of bleeding (eg warfarin with INR greater than 2.0) within the next 12 hours Lumbar puncture/epidural/spinal anaesthesia within Acute stroke the previous 4 hours Thrombocytopaenia (platelets less than 75) Uncontrolled systolic hypertension (230/120 mmHg or higher) Untreated inherited bleeding disorders (such as haemophilia and von Willebrand’s disease) Reference: Risk Assessment for Venous Thromoboembolism (VTE). National Institute for Health and Clinical Excellence, London UK. March 2010. See http://www.nice.org.uk/guidance/CG92
0ecfb4ea89a8335cf9351234be5641b5.doc C/8/OrthHipFracture/MD/03-15/V1/Post-op ACUTE CARE: BOWEL INTERVENTION - ADULTClinical Decision Support
Clinical Regimen Note: not for use in patients who have had bowel surgery in the last year Newly-admitted patients experiencing constipation longer than 4 days or those unable to identify date of last bowel movement start at step 2 All other patients requiring bowel care per protocol including those where assessment not possible begin at baseline
Notify physician if vomiting and abdominal pain develop Discontinue protocol and notify MRP if step 4 reached more than once in 10 days Intervention for Constipation Medication Baseline No medication Step 2: Last BM more than lactulose 30 mL PO x 1 today and 48 hours ago If no results by next AM proceed to next step Increase lactulose to 30 mL PO BID today, and Step 3: Last BM more than 72 hours ago sennosides 24 mg PO after breakfast today, and If no results in 24 hours proceed to next step Continue with lactulose 30 mL PO BID AND sennosides 24 mg PO after breakfast today, and glycerine suppository (2.65 g) PR after breakfast today x 1 Step 4: Last BM more than 96 hours ago If no results after 3 hours give sodium citrate enema (Microlax) 5 mL PR x 1 today If no results from sodium citrate enema perform rectal examination for presence or absence of stool and inform physician Return to baseline once desired results are achieved
Page 12/7
RN’s Signature College License # Date Time
RN to sign. Send addressographed labelled order to pharmacy ACUTE CARE: BOWEL INTERVENTION - ADULTClinical Decision Support
References References
Activity
Bone & Joint Canada Hip Fracture Tool Kit 2011 Wasdell ed.
Handoll HH SCMJ. Interventions aimed at improving and restoring mobility after hip fracture. Cochrane Database Syst Rev. 2011;3.
Kristensen MT, Andersen L, Bech-Jensen R, et al. High intertester reliability of the cumulated ambulation score for the evaluation of basic mobility in patients with hip fracture. Clin Rehabil. Dec 2009;23(12):1116-1123.
Overgaard J, Kristensen MT. Feasibility of progressive strength training shortly after hipfracture surgery. World journal of orthopedics. 2013;4(4):248-258.
Sherrington C, Lord SR, Herbert RD. A randomized controlled trial of weight-bearing versus non- weight-bearing exercise for improving physical ability after usual care for hip fracture. Arch Phys Med Rehabil. May 2004;85(5):710-716.
Pashikanti, L., Von Ah, D. Impact of Early Mobilization Protocol on the Medical-Surgical Inpatient Population: An Integrated Review of Literature. Clinical Nurse Specialist, Lippincott 2012.
Laboratory
Flesher, M.E. Archer K.A., Leslie, B.D. McCollom, R. Martinka, G. P. Assessing the Metabolic and Clinical Consequences of Early Enteral Feeding in the Malnourished Patient JPEN J Parenter Enteral Nutr March 2005 vol. 29 no. 2 108-117 .
Holidk, M. F., Binkley, N.C., Bischoff-Ferrairi H. A. , Gordon C.M., Hanley D. A., Heaney R. P. Hassan, M. H., Weaver, C. M. Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline. DOI: http://dx.doi.org/10.1210/jc.2011-0385 Received: February 14, 2011
Page 12/7 Laulund AS, Lauritzen JB, Duus BR, Mosfeldt M, Jørgensen HL. Routine blood tests as predictors of mortality in hip fracture patients. Injury. 2012 Jul;43(7):1014- 20. doi: 10.1016/j.injury.2011.12.008. Epub 2012 Jan 10.
Portsmouth Hospital NHS Trust. Guidelines for the management of patients at risk for refeeding syndrome.
ACUTE CARE: BOWEL INTERVENTION - ADULTClinical Decision Support
References continued
Diet Type Björkelund,K., Hommel,A., Thorngren K.G. Lundberg, D., Larrson, S. The Influence of Perioperative Care and Treatment on the 4-Month Outcome in Elderly Patients With Hip Fracture AANA Journal ß, February 2011, ß Vol. 79, No. 1
Hearing, S. D. Refeeding syndromeIs underdiagnosed and undertreated, but treatable BMJ. 2004 April 17; 328(7445): 908–909. doi: 10.1136/bmj.328.7445.908
Hommel, A., Hertz K. & Mainz, H. Personal communication: International Collaboration of Nursing Hip Fracture Working Group. Feb 16th, 2014.
Eneroth M, Olsson UB, Thorngren KG. Insufficient fluid and energy intake in hospitalised patients with hip fracture. A prospective randomised study of 80 patients. Clin Nutr 2005; 24: 297–303.
Fossi B, Jensen P & Kehlet H. Risk factors for insufficient perioperative oral nutrition after hip fracture surgery within a multi-modal rehabilitation programme Age and Ageing 2007; 36: 538– 543
Lawson RM, Doshi MK, Ingoe LE, Colligan JM, Barton JR, Cobden I. Compliance of orthopaedic patients with postoperative oral nutritional supplementation. Clin Nutr 2000; 19: 171–5.
Radtke, F. M; Franck, M.; MacGuill, M.; Seeling, M.; Lütz, A.; Westhoff, S.; Neumann, U.; Wernecke, K. D; Spies, C. Duration of fluid fasting and choice of analgesic are modifiable factors for early postoperative delirium. European Journal of Anaesthesiology: May 2010 - Volume 27 - Issue 5 - p 411–416
Volkert D,Kreuel H, Heseker H, Stehle P. Energy and nutrient intake of young-old, old-old and very-old elderly in Germany. Eur J Clin Nutr 2004; 58: 1190–200.
Assessments & Treatments
Hommel, A., Hertz K. & Mainz, H. Personal communication:Page 12/7 International Collaboration of Nursing Hip Fracture Working Group Meeting. Feb 16th, 2014.
British Orthopaedic Association (BOA). Care of Patients with Fragility Fractures Blue Book, 2007. ACUTE CARE: BOWEL INTERVENTION - ADULTClinical Decision Support
References continued
Analgesics
Bédard,D., Purden, M.A., Sauvé-Larose,N., Certosini,C. Schein C., The Pain Experience of Post Surgical Patients Following the Implementation of an Evidence-Based Approach, Pain Management Nursing, Volume 7, Issue 3, September 2006, Pages 80-92, ISSN 1524-9042, Http://dx.doi.org/10.1016/j.pmn.2006.06.001. (http://www.sciencedirect.com/science/article/pii/S1524904206000841)
Feldn, L., et al., (2011). Comparative clinical effects of hydromorphone and morphine: a meta- analysis. British Journal of Anaesthesia, 107(3): 319-28
Osborne, R. J., Joel, S. P., & Slevin, M. L. (1986). Morphine intoxication in renal failure: the role of morphine-6-glucuronide. BMJ. 292:1548-9
Maher, A., Meehan, A., Hertz, K, Hommel, A., MacDonald, V., O’Sullivan, M., Specht, K., Taylor, A. Acute nursing care of the older adult with fragility hip fracture: An international perspective (Part 1) International Journal of Orthopaedic and Trauma Nursing Volume 16, Issue 4 , Pages 177-194, November 2012
Meineke, I. et. al, (2002). Pharmacokinetic modelling of morphine, morphine-3-glucuronide and morphine-6-glucuronide in plasma and cerebrospinal fluid of neurosurgical patients after short- term infusion of morphine. Br J Clin Pharmacol 54:592-603.
Morrison, S.r., Magaziner, J, Gilbert, M. Koval, K. McLaughlin, M.A. Orosz, G. Relationship Between Pain and Opioid Analgesics on the Development of Delirium Following Hip Fracture J Gerontol A Biol Sci Med Sci (2003) 58 (1): M76-M81. doi: 093/gerona/58.1.M76
Zywil, M. G., & Perruccio, A. V. (2013). The influence of anaesthesia and pain management on cognitive dysfunction after joint arthroplasty. Clin Orthop Relat Res, DOI: 10.1007/s11999-013- 3363-2
Trelle, S. Reichenbach, S., Wandel, s. Hildebrand, P, Tschannen, B., Billiger, P. Egger, M. Ju’ni, P. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis BMJ 2011;342:c7086doi:10.1136/bmj.c7086 Page 12/7 ACUTE CARE: BOWEL INTERVENTION - ADULTClinical Decision Support
References continued
Antiemetic
Kloth, D. D. (2009). New pharmacologic findings for the treatment of PONV and PDNV. AM J Health-Syst Parm, 66(supp1): S11-S18.
The American Geriatrics society, (2012). American geriatrics society updated Beers criteria for potentially inappropriate medication use in older adults, JAGS 2012, accessed from http://www.americangeriatrics.org/files/documents/beers/2012BeersCriteria_JAGS.pdf
Delirium
Hawkins, S., Bucklin, M. & Muzyk, A. Quetiapine for the treatment of delirium. Journal of Hospital Medicine Volume 8, Issue 4, pages 215–220, April 2013
Clinical Practice Guidelines for the Management of Delirium in Older People Clinical Epidemiology and Health Service Evaluation Unit, Melbourne Health in collaboration with the Delirium Clinical Guidelines Expert Working Group. Commissioned on behalf of the Australian Health Ministers’ Advisory Council (AHMAC), by the AHMAC Health Care of Older Australians Standing Committee (HCOASC). 2011
Sedation
The American Geriatrics society, (2012). American geriatrics society updated Beers criteria for potentially inappropriate medication use in older adults, JAGS 2012, accessed from: http://www.americangeriatrics.org/files/documents/beers/2012BeersCriteria_JAGS.pdf
Pneumonia prevention
Yoon, M.N. & Steele, C.M. (2007). The oral care imperative: The link between oral hygiene and aspiration pneumonia. Topics in Geriatric Rehabilitation, 23(3), 280-288.
Skin Preparation Page 12/7 Safer Healthcare Now! (Mar, 2011). Prevent Surgical Site Infections:Getting Started Kit. Retrieved from http://www.saferhealthcarenow.ca/en/interventions/ssi ACUTE CARE: BOWEL INTERVENTION - ADULTClinical Decision Support
References continued Bone Health
Bischoff-Ferrari H.A., Willett W. J., Endel P.H., Oray, J., Meunier P. J., Lyons R. A., Flicker L., Wark, J., Jackson R.D., Cauley J.A., Meyer H. E., Pfeifer,M., Sander, K., Stahelin,H., Theirler. R., Dawson-Hughes, B. A Pooled Analysis of Vitamin D Dose Requirements for Fracture Prevention. N Engl J Med 2012; 367:40-49July 5, 2012DOI: 10.1056/NEJMoa1109617
British Orthopaedic Association (BOA). Care of Patients with Fragility Fractures, 2007.
Parker MJ, Gillespie WJ, Gillespie LD. Effectiveness of hip protectors for preventing hip fractures in elderly people: a systematic review. BMJ. 2006;332(7541):571-574.
Stone, K.L., Seeley, G., Lui L., Cauley, J., Ensrud, K., Browner, W. Nevitt, M. Cummings, S. BMD at Multiple Sites and Risk of Fracture of Multiple Types: Long-Term Results From the Study of Osteoporotic Fractures. JOURNAL OF BONE AND MINERAL RESEARCH Volume 18, Number 11, 2003.
VTE
Scottish Intercollegiate Guidelines Network. Management of Hip Fracture in Older People: A national guideline. 2009
Antibiotic Prophylaxis
Bratzler, D. W., Dellinger, P, Olsen, K.M., Perl, T.M., Auwaerter, P.G., Bolon, M.K., Fish, D.N. Napolitano, l.M. , Sawyer, R.G. Slain, D., Steinberg,J.P. Weinstein R.A. Clinical practice guidelines for antimicrobial prophylaxis in surgery Am J Health-Syst Pharm. 2013; 70:195-283
Gehrke, T., Parvize, J. Chairmen. Proceedings of the International Consensus Meeting on Periprosthetic Joint Infection. Philidelphia 2014
Bowel Care Page 12/7
Rao, S.C. & Go, J.T. Update on the management of constipation in the elderly: new treatment options. Clin Interv Aging. 2010; 5: 163–171.Published online 2010 August 9.