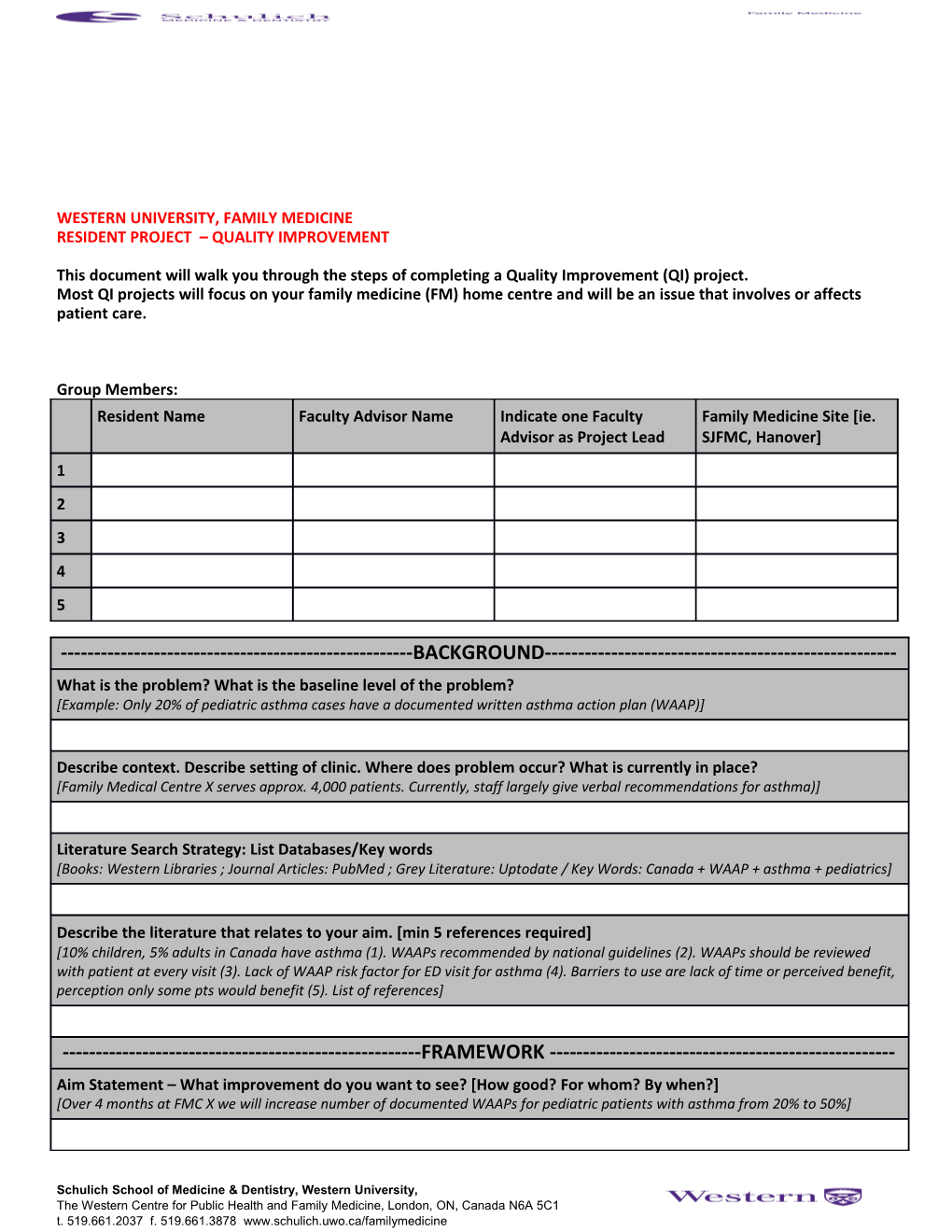
WESTERN UNIVERSITY, FAMILY MEDICINE RESIDENT PROJECT – QUALITY IMPROVEMENT
This document will walk you through the steps of completing a Quality Improvement (QI) project. Most QI projects will focus on your family medicine (FM) home centre and will be an issue that involves or affects patient care.
Group Members: Resident Name Faculty Advisor Name Indicate one Faculty Family Medicine Site [ie. Advisor as Project Lead SJFMC, Hanover] 1 2 3 4 5
------BACKGROUND------What is the problem? What is the baseline level of the problem? [Example: Only 20% of pediatric asthma cases have a documented written asthma action plan (WAAP)]
Describe context. Describe setting of clinic. Where does problem occur? What is currently in place? [Family Medical Centre X serves approx. 4,000 patients. Currently, staff largely give verbal recommendations for asthma)]
Literature Search Strategy: List Databases/Key words [Books: Western Libraries ; Journal Articles: PubMed ; Grey Literature: Uptodate / Key Words: Canada + WAAP + asthma + pediatrics]
Describe the literature that relates to your aim. [min 5 references required] [10% children, 5% adults in Canada have asthma (1). WAAPs recommended by national guidelines (2). WAAPs should be reviewed with patient at every visit (3). Lack of WAAP risk factor for ED visit for asthma (4). Barriers to use are lack of time or perceived benefit, perception only some pts would benefit (5). List of references]
------FRAMEWORK ------Aim Statement – What improvement do you want to see? [How good? For whom? By when?] [Over 4 months at FMC X we will increase number of documented WAAPs for pediatric patients with asthma from 20% to 50%]
Schulich School of Medicine & Dentistry, Western University, The Western Centre for Public Health and Family Medicine, London, ON, Canada N6A 5C1 t. 519.661.2037 f. 519.661.3878 www.schulich.uwo.ca/familymedicine Family of Measures – How will you measure it? [describe what and how you will collect data] 1. Outcome Measure [# of documented WAAPs in electronic medical record, search EMR for all cases by…] 2. Process Measure [Rate of WAAP use per month, ask staff to keep track/assess during monthly meets] 3. Balance Measure [Qualitative feedback on staff satisfaction with these appointments as monitored per monthly staff meeting] Changes - Brainstorm changes to improve [use QI tools -cause and effect and process diagrams, literature, etc] [Develop context specific WAAP, staff education, Implement reminder in EMR, focus group with staff to identify change idea, etc] [Changes might be working towards: developing a change idea, testing a change, or implementing a change]
Describe barriers and how will be addressed? Is idea realistic within context of staff/setting/resources? [Technology- Access a local expert? Change behavior of staff- Get ‘champions’ in centre to endorse, etc]
Who are key stakeholders and what are their roles in the planned changes? [Staff physicians, nurses, residents, allied health- all stakeholders must be willing to adapt and/or participate, patients, etc]
After completing above section, identify a change to test within a Plan-Do-Study-Act (PDSA) cycle. PDSA 1 should be a very small test. Subsequent PDSAs can be larger if PDSA 1 is successful. IF PDSA 1 does not work, think ‘why’ and determine another change to test. For this project, you should aim to complete at least 2 PDSAs.
------PLAN DO STUDY ACT------Cycle # : Start Date: End Date: PLAN Describe a short objective of this cycle. What do you predict will happen? [After developed a WAAP specific to FMC X, pilot test it on 3 patients over 1 month. I predict staff will find it useful]
Test/implementation plan:
Version date: 2015-01-23 3 What change tested? Who will run the test? How is it tested? When and where will it take place? [The WAAP can be used during any pediatric visit where the [One physician and two residents on the team will use one WAAP patient has asthma. Forms will be available in each room] during a relevant visit during 1 month period at FMC X]
Data collection plan: What information will you collect and why? Who will collect and analyze the data? How will the data be collected? When and where will data collection take place? [Team meeting with questions such as: Was the WAAP effective? [Two residents will take notes during meeting in conference room What could be changed to improve WAAP?] at end of month and group responses into themes]
STOP: YOU HAVE NOW COMPLETED THE PROPOSAL. SUBMIT THIS DOCUMENT TO OWL.
AFTER MAKING REVISIONS TO PROPOSAL BASED ON FEEDBACK FROM FACULTY ADVISOR AND RESIDENT PROJECT COORDINATOR, IMPLEMENT YOUR PLAN. DO Observations not related to the plan. Did you need to change original plan? How? Observations related to the plan. [One resident did not use WAAP. Forms mistakenly [Two WAAP forms used.] moved/relevant patients not seen. Electronic WAAP stored/printed when needed]
STUDY Summarize what was learned. Begin analysis of data [Overall WAAP effective. WAAP focus much on alerts and little on preventive care. WAAP takes time as patients had many questions]
Did the change lead to improvement? Why or why not? Compare data to your predictions. [WAAP appears to be effective and might lead to improvements but needs modification for content and timing]
ACT Describe what modifications should be made. [Adjust WAAP to focus more on preventive care. Modify readability of WAAP for patients.]
Describe next PDSA cycle: What is your next test? [Modify WAAP and test during all relevant visits for one month]
FOR THE RESIDENT PROJECT SHOULD COMPLETE AT LEAST ONE MORE PDSA. IF REQUIRE MORE PDSA FORMS, COPY/PASTE THE BELOW FORM AS NEEDED.
------PLAN DO STUDY ACT------
Version date: 2015-01-23 Cycle # : Start Date: End Date: PLAN Describe a short objective of this cycle. What do you predict will happen?
Test/implementation plan What change tested/implemented? Who will run the test/implementation? How tested/implemented? When and where will it take place?
Data collection plan: What information will you collect and why? Who will collect and analyze the data? How will the data be collected? When and where will data collection take place?
DO Observations not related to the plan. Observations related to the plan. Did you need to change original plan? How?
STUDY Summarize what was learned. Begin analysis of data [collect outcome, process, balance measures]
Did the change lead to improvement? Why or why not? Compare data to your predictions.
ACT Describe what modifications should be made.
Describe next PDSA cycle: What is your next test?
Version date: 2015-01-23 5
AFTER COMPLETING AT LEAST TWO PDSAS, COMPLETE SUMMARY REPORT BELOW ------SUMMARY REPORT------Give brief summary of results for each family of measure below Outcome Measure Process Measure Family Measure Present your results for the outcome measure with the below graph (or create your own chart within word or excel) [Right click on chart area and select “Edit Data”. Change data to reflect your numbers]
If results did not reach goal, what are possible explanations for the variance from the target?
Describe successes during this project Describe challenges encountered during project
------CONCLUSION ------Summarize the project. Discuss significance and relate findings to the literature (minimum 5 references)
Might the project be generalizable to other systems? Is this project sustainable?
What are your reflections on quality improvement after completing this project?
YOU HAVE NOW COMPLETED THE SUMMARY REPORT. FINAL SUBMISSION TO OWL INCLUDES: -COMPLETED QUALITY IMPROVEMENT FORM (THIS DOCUMENT) -ANY FORMS, DATA COLLECTION INSTRUMENTS, HANDOUTS, PRESENTATIONS, PROCESS MAPS, CAUSE AND EFFECT DIAGRAMS, ETC USED DURING PROPOSAL STAGE OR PDSAs
Version date: 2015-01-23