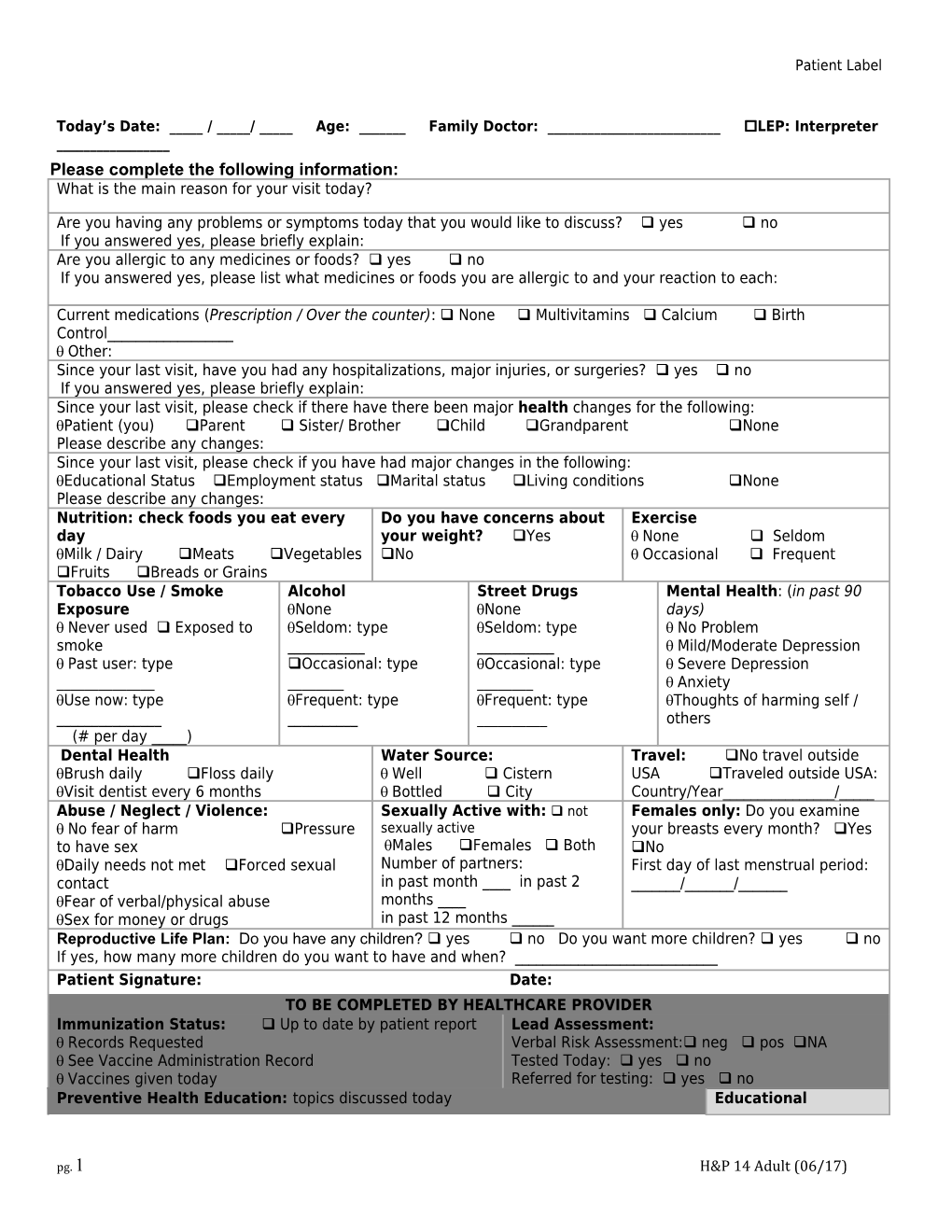
Patient Label
Today’s Date: _____ / _____/ _____ Age: ______Family Doctor: ______LEP: Interpreter ______Please complete the following information: What is the main reason for your visit today?
Are you having any problems or symptoms today that you would like to discuss? yes no If you answered yes, please briefly explain: Are you allergic to any medicines or foods? yes no If you answered yes, please list what medicines or foods you are allergic to and your reaction to each:
Current medications (Prescription / Over the counter): None Multivitamins Calcium Birth Control______ Other: Since your last visit, have you had any hospitalizations, major injuries, or surgeries? yes no If you answered yes, please briefly explain: Since your last visit, please check if there have there been major health changes for the following: Patient (you) Parent Sister/ Brother Child Grandparent None Please describe any changes: Since your last visit, please check if you have had major changes in the following: Educational Status Employment status Marital status Living conditions None Please describe any changes: Nutrition: check foods you eat every Do you have concerns about Exercise day your weight? Yes None Seldom Milk / Dairy Meats Vegetables No Occasional Frequent Fruits Breads or Grains Tobacco Use / Smoke Alcohol Street Drugs Mental Health: (in past 90 Exposure None None days) Never used Exposed to Seldom: type Seldom: type No Problem smoke ______ Mild/Moderate Depression Past user: type Occasional: type Occasional: type Severe Depression ______ Anxiety Use now: type Frequent: type Frequent: type Thoughts of harming self / ______others (# per day _____) Dental Health Water Source: Travel: No travel outside Brush daily Floss daily Well Cistern USA Traveled outside USA: Visit dentist every 6 months Bottled City Country/Year______/_____ Abuse / Neglect / Violence: Sexually Active with: not Females only: Do you examine No fear of harm Pressure sexually active your breasts every month? Yes to have sex Males Females Both No Daily needs not met Forced sexual Number of partners: First day of last menstrual period: contact in past month ____ in past 2 ______/______/______Fear of verbal/physical abuse months ____ Sex for money or drugs in past 12 months ______Reproductive Life Plan: Do you have any children? yes no Do you want more children? yes no If yes, how many more children do you want to have and when? ______Patient Signature: Date: TO BE COMPLETED BY HEALTHCARE PROVIDER Immunization Status: Up to date by patient report Lead Assessment: Records Requested Verbal Risk Assessment: neg pos NA See Vaccine Administration Record Tested Today: yes no Vaccines given today Referred for testing: yes no Preventive Health Education: topics discussed today Educational
pg. 1 H&P 14 Adult (06/17) Child development Physical activity Preconception /Folic Acid Pelvic / Handouts: Pap FPEM PTEM Immunizations Safety Prenatal / Genetics SBE CSEM Other: /Mammogram Dental Mental Health CVD STE / PSA Patient Verbalizes Hearing/Vision DV/SA Arthritis HRT Understanding of Lead exposure (ACH-25a) ATOD / Cessation / SHS Osteoporosis Education given STD / HIV Diet / Nutrition Diabetes Cancer Reproductive Life Plan Options Counseling MINOR Family Planning: Sexual coercion. Abstinence. Benefits of parental involvement.
Healthcare Provider Signature: Date:
SUBJECTIVE / PRESENTING PROBLEM:
OBJECTIVE: General Multi-System Examination SYSTEM WNL ABNORMAL SYSTEM WNL ABNORMAL General appearance Lymphatic Neck, Axilla, Constitution Groin al Nutritional status Spine Vital signs Musculoskele ROM Head: Fontanels, tal Symmetry Scalp Eyes: PERRL Inspection(rash Skin / SQ es) Conjunctivae, lids Tissue Palpation (nodules) HEENT Ear: Canals, Drums Reflexes Neurological Hearing Sensation Nose: Mucosa/ Orientation Septum Psychiatric Mouth: Lips, Palate Mood / Affect Teeth, Gums EXPLANATION OF ABNORMAL FINDINGS: Throat: Tonsils Overall appearance Neck Thyroid Respiratory effort Respiratory Lungs Heart Cardiovascu Femoral/Pedal lar pulses Extremities Thorax Chest Nipples Breasts Abdomen Gastro- Tanner Stage: typical atypical Liver / Spleen intestinal Anus / Perineum X-Ray: Type: Result: Male: Scrotum Date taken:No Change Testes Date read: Neg/Non-remarkable Penis Date compared with: Improved Worsening Genitourinar y
Prostate Female:Genitalia Patient Label
Vagina TB Classification: TB suspect Cervix 0 No TB exposure, not infected Uterus I TB exposure, no evidence of infection Adnexa II TB infection, without disease III TB, clinically active IV TB, not clinically active Site of infection: Pulmonary __Cavity __Non Cavity Other: ASSESSMENT:
PLAN:
Testing today: N/A Medications/Supplies: Recommendations made to client, Referrals made: N/A GC /Chlamydia urine N/A for scheduling of follow-up testing PCP/Medical Home GC/Chlamydia swab MV / Folic Acid and Pediatrician UA TST Number of bottles procedures, based on assessment: WIC VDRL HIV Hep given_____ N/A Specialist: C Birth Control Method Vision Hearing FBS FP Pap Lead ______/GTT Radiology Hgb Cholesterol Given Rx Dental Lipid Screen Medicaid Blood Glucose Foam Issued (#) ______ Hgb MNT with RD HANDS Urine PT / UCG: Pos Condoms Issued (#) Pap Smear Sickle Cell Lead Social Services Neg Planned ______ Mammogram Ultrasound 1-800-QUIT-NOW pregnancy? Yes No Foam/Condoms offered; Other: Freedom from Smoking Wet Mount pt. declined UCG/HCG TST / CXR Other: Other: Other: Bone Density Liver Panel Blood Glucose Colorectal Scr. Ovarian Cancer Scr. : Healthcare Provider Signature: Date: Recommended RTC:
pg. 3 H&P 14 Adult (Rev. 06/17)