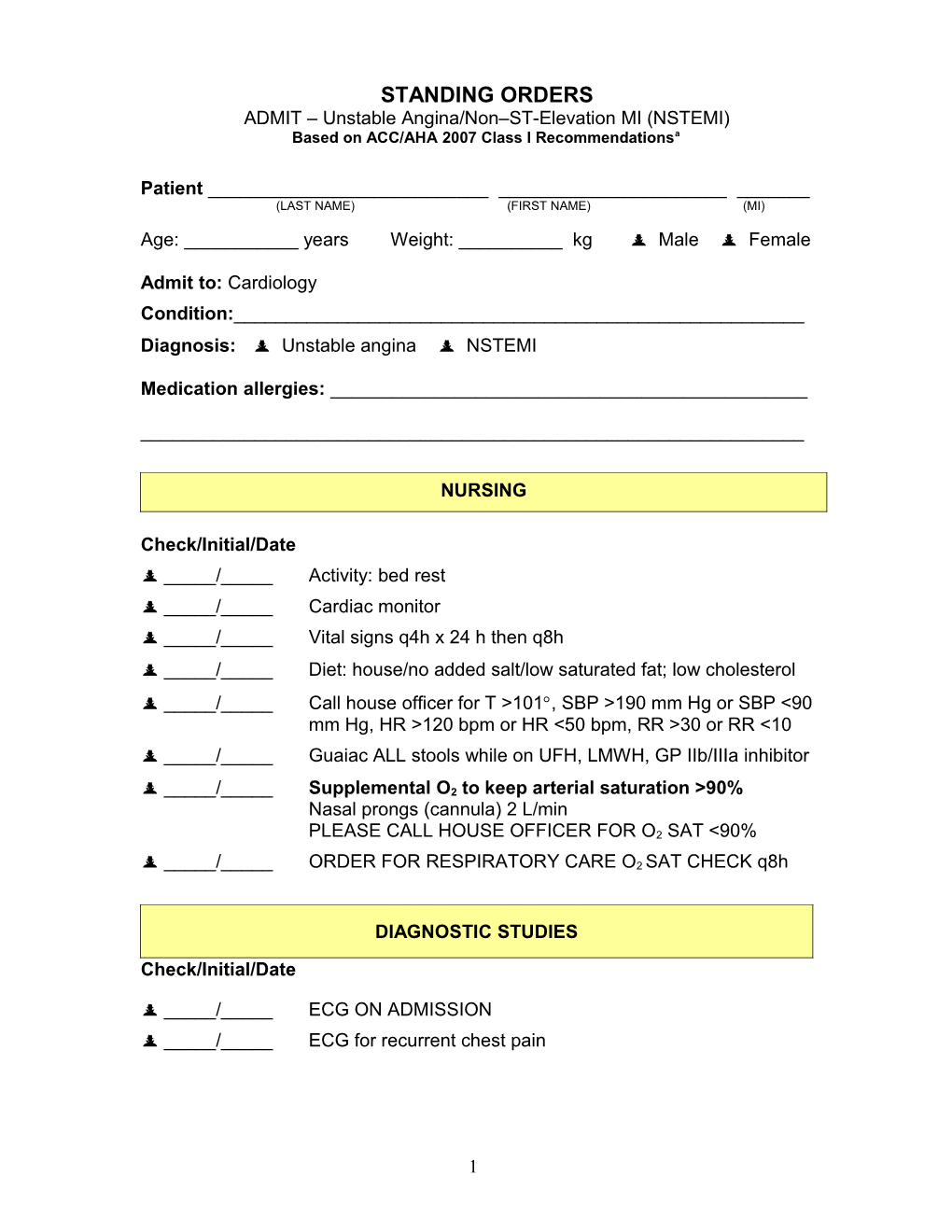
STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
Patient ______(LAST NAME) (FIRST NAME) (MI) Age: ______years Weight: ______kg Male Female
Admit to: Cardiology Condition:______Diagnosis: Unstable angina NSTEMI
Medication allergies: ______
______
NURSING
Check/Initial/Date _____/_____ Activity: bed rest _____/_____ Cardiac monitor _____/_____ Vital signs q4h x 24 h then q8h _____/_____ Diet: house/no added salt/low saturated fat; low cholesterol _____/_____ Call house officer for T >101, SBP >190 mm Hg or SBP <90 mm Hg, HR >120 bpm or HR <50 bpm, RR >30 or RR <10 _____/_____ Guaiac ALL stools while on UFH, LMWH, GP IIb/IIIa inhibitor
_____/_____ Supplemental O2 to keep arterial saturation >90% Nasal prongs (cannula) 2 L/min PLEASE CALL HOUSE OFFICER FOR O2 SAT <90%
_____/_____ ORDER FOR RESPIRATORY CARE O2 SAT CHECK q8h
DIAGNOSTIC STUDIES
Check/Initial/Date
_____/_____ ECG ON ADMISSION _____/_____ ECG for recurrent chest pain
1 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
LABORATORY STUDIES
Check/Initial/Date
CARDIAC MARKERS _____/_____ Troponin T/Troponin I: NOW AND EVERY _____hrs ___ times _____/_____ CK-MB: NOW AND EVERY _____ hrs ___ times
CHEMISTRY PANEL _____/_____ CBC, Lipid Profile, PTT, Chemistry (7) panel in AM – FASTING
MEDICATIONS
Check/Initial/Date
_____/_____ Aspirin 162-325 (______insert dose) mg po chewed (loading dose) now, then 75-162 mg/d po (or 162-325 mg/d after stent implantation) daily maintenance dose
_____/_____ If aspirin intolerant, use clopidogrel 300-600 (______insert dose) mg po x 1(loading dose),b then 75 mg/d po
_____/_____ Stop all NSAIDs except aspirin
2 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
MEDICATIONS cont
Check/Initial/Date -BLOCKER Hold if signs of HF, evidence of a low-output state, increased risk for cardiogenic shock (age >70 y, SBP <120 mm Hg, sinus tachycardia >110 bpm or heart rate <60 bpm, increased time since onset of UA/NSTEMI symptoms), or other relative contraindications to β-blockade (PR interval >0.24 s, second- or third-degree heart block, active asthma, or reactive airway disease).
Choose one:
IV -Blocker (optional; reserved for patients with refractory tachycardia or refractory hypertension; otherwise, oral β- blockade is sufficient) _____/_____ Drug: ______mg IV every ____ hrs Oral -Blocker _____/_____ METOPROLOL TARTRATE 50-200 mg bid _____/_____ ATENOLOL 50-200 mg/d _____/_____ CARVEDILOL 6.25 mg bid, uptitrated to max. 25 mg bid
NITROGLYCERIN
_____/_____ NITROGLYCERIN 1/150 (0.4 mg) 1 TAB SL q5min x 3 prn chest pain; HOLD IF: SBP <100 mm Hg _____/_____ NITROGLYCERIN 5-200 µg/min IV in D5W continuous IV _____/_____ NITROGLYCERIN, transdermal, 0.2 to 0.8 mg/h q12h, tolerance in 7 to 8 h
3 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
EARLY RISK STRATIFICATION
Check/Initial/Date
_____/_____ High risk Intermediate risk Low risk
High risk: elevated cardiac biomarkers, ST depression, transient ST elevation, >20 min of rest pain, hemodynamic instability, signs of CHF INITIAL INVASIVE STRATEGY (Diagnostic angiography with intent to revascularize)
Intermediate risk: no high-risk features, prior MI, prior CABG, T-wave inversions, rest angina <20 min relieved promptly with nitroglycerin, age >70 years EITHER INITIAL INVASIVE OR INITIAL CONSERVATIVE STRATEGY
Low risk: No high- or moderate-risk features, progressive angina without prolonged rest pain, normal cardiac markers, normal ECG with pain INITIAL CONSERVATIVE STRATEGY
_____/_____ Invasive strategy Conservative strategy
Selection of Initial Treatment Strategy: Patient Characteristics Invasive Strategy Preferred ● Recurrent angina or ischemia at rest or with low-level activities ● Elevated cardiac biomarkers (TnT or TnI) ● New or presumably new ST-segment depression ● Signs or symptoms of HF or new or worsening mitral regurgitation ● High-risk findings from noninvasive testing ● Hemodynamic instability ● Sustained ventricular tachycardia ● PCI within 6 months ● Prior CABG ● High risk score (eg, TIMI, GRACE) ● Reduced LV function (LVEF <40%) Conservative (Selectively Invasive) Strategy Preferred ● Low risk score ● Patient or physician preference in absence of high-risk features
It is reasonable for initially stabilized high-risk patients with UA/NSTEMI* (GRACE risk score >140) to undergo an early invasive strategy within 12 to 24 hours of admission. For patients not at high risk, an early invasive approach is also reasonable (Class IIa, LOE: B).c
*Immediate catheterization/angiography is recommended for unstable patients.
4 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
INITIAL INVASIVE STRATEGY (High- or Intermediate-Risk Patients)
Check/Initial/Date
Initiate at least one (Class I, LOE: A) or both (Class IIa, LOE: B) of the following:
_____/_____ Clopidogrel 300-600 (______insert dose) mg po x 1 (loading dose),b then 75 mg/d po. Withhold for 5 days if CABG is planned.
OR
_____/_____ Prasugrel (at the time of PCI) 60 mg po x 1 (loading dose),c then 10 mg/d po. Do not use prasugrel in patients with active pathological bleeding or a history of TIA or stroke. In patients ≥75 years of age, prasugrel is generally not recommended because of the increased risk of fatal and intracranial bleeding and uncertain benefit, except in high-risk situations (patients with diabetes or a history of prior MI) for which its effect appears to be greater and its use may be considered. Do not start prasugrel in patients likely to undergo urgent CABG. When possible, discontinue prasugrel at least 7 days before any surgery.
AND/OR
GLYCOPROTEIN IIB/IIIA INHIBITOR THERAPY (choose one): _____/_____ Eptifibatide 180 µg/kg IV bolus x 2, 10 min apart, followed by IV infusion of 2.0 µg/kg/min, reduce to 1.0 µg/kg/min if CrCl <50 mL/min. Continue for 18 to 24 hours post-PCI. OR _____/_____ Tirofiban IV infusion of 0.4 µg/kg/min for 30 min, reduce to 0.2 µg/kg/min for CrCl <30 mL/min, followed by IV infusion of 0.1 µg/kg/min, reduce to 0.05 µg/kg/min if CrCl <30 mL/min. Continue for 18 to 24 hours post-PCI. OR _____/_____ Abciximab 0.25 mg/kg IV bolus administered 10-60 min before the start of PCI, followed by IV infusion of 0.125 µg/kg/min (to a maximum of 10 μg/min). Continue for 12 hours post-PCI. Indicated only if there is no appreciable delay to angiography and PCI is likely to be performed. Reserve only for patients with planned PCI within 24 hours.
5 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
INITIAL INVASIVE STRATEGY (High- or Intermediate-Risk Patients) cont
Either an IV GP IIb/IIIa inhibitor (eptifibatide or tirofiban; Class I, LOE: A) or clopidogrel (loading dose followed by daily maintenance dose; Class I, LOE: A) should be added to aspirin and anticoagulant therapy before diagnostic angiography.
For UA/NSTEMI patients in whom an initial invasive strategy is selected, it is reasonable to initiate antiplatelet therapy with both clopidogrel (loading dose followed by daily maintenance dose) and a GP IIb/IIIa inhibitor (Class IIa, LOE: B).
Factors favoring administration of both clopidogrel and a GP IIb/IIIa inhibitor include delay to angiography, high-risk features, and early recurrent ischemic discomfort.
Check/Initial/Date
ANTICOAGULANT THERAPY (choose one): (A) or (B) denotes level of evidence designation.
_____/_____ Unfractionated Heparin (A) (for 48 hours) 60 U/kg IV bolus (not to exceed 4000 U), followed by IV infusion of 12 U/kg/h (not to exceed 1000 U/h) to achieve goal aPTT 1.5 to 2.0 times control (approximately 50 to 70 s); check aPTT in 6 h and adjust heparin as indicated (see appendix for titration nomogram) OR _____/_____ Enoxaparind (A) 1 mg/kg SC q12h (if CrCl <30 mL/min, give 1 mg/kg every 24 h). Continue for the duration of hospitalization, 8 days, or until PCI or CABG is performed. OR _____/_____ Fondaparinux (B) 2.5 mg SC once daily (avoid if CrCl <30 mL/min). Continue for the duration of hospitalization, 8 days, or until PCI or CABG is performed. UFH, per institutional practice, should be administered for any PCI procedure. OR _____/_____ Bivalirudin (B) 0.1 mg/kg IV bolus, then IV infusion of 0.25 mg/kg/h (use with caution if CrCl <30 mL/min). Continue until PCI is performed or for up to 4 h post-PCI. Discontinue 3 h before CABG and dose with UFH per institutional practice.
6 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
INITIAL CONSERVATIVE STRATEGY (Low- or Intermediate-Risk Patients)
Check/Initial/Date
_____/_____ Clopidogrel 300 mg po x 1 (loading dose), b then 75 mg/d po
ANTICOAGULANT THERAPY (choose one): (A) or (B) denotes level of evidence designation.
_____/_____ Unfractionated Heparin (A) (for 48 hours) 60 U/kg IV bolus (not to exceed 4000 U), followed by IV infusion of 12 U/kg/h (not to exceed 1000 U/h) to achieve goal aPTT 1.5 to 2.0 times control (approximately 50 to 70 s); check aPTT in 6 h and adjust heparin as indicated.
OR
_____/_____ Enoxaparinc (A) 1 mg/kg SC q12h (if CrCl <30 mL/min, give 1 mg/kg every 24 h) OR _____/_____ Fondaparinux (B) 2.5 mg SC once daily (avoid if CrCl <30 mL/min). Preferred if high risk of bleeding. Continue IV UFH for at least 48 h (Class I, LOE: A) or enoxaparin or fondaparinux for the duration of the hospitalization (Class I, LOE: A). Enoxaparin or fondaparinux is preferable to UFH as anticoagulant therapy, unless CABG is planned within 24 h (Class IIa, LOE: B). For UFH, consult Unfractionated Heparin Dosing Chart.
_____/_____ Schedule assessment of LVEF _____/_____ Schedule stress test _____/_____ Start early invasive strategy if patient has recurrent symptoms/ischemia, HF, arrhythmias, positive cardiac biomarkers, or positive stress test
7 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
INITIAL CONSERVATIVE STRATEGY (Low- or Intermediate-Risk Patients) cont
GLYCOPROTEIN IIB/IIIA INHIBITOR THERAPY
For UA/NSTEMI patients in whom an initial conservative (ie, noninvasive) strategy is selected, it may be reasonable to add eptifibatide or tirofiban to anticoagulant and oral antiplatelet therapy (Class IIb, LOE: B).
_____/_____ Eptifibatide 180 µg/kg IV bolus, followed by IV infusion of 2.0 µg/kg/min (reduce to 1.0 µg/kg/min if CrCl <50 mL/min) OR _____/_____ Tirofiban IV infusion of 0.4 µg/kg/min for 30 min, reduce to 0.2 µg/kg/min for CrCl <30 mL/min, followed by IV infusion of 0.1 µg/kg/min, reduce to 0.05 µg/kg/min if CrCl <30 mL/min
8 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
AS-NEEDED MEDICATIONS
Check/Initial/Date
_____/_____ DOCUSATE SODIUM 100 mg po bid _____/_____ MAALOX PLUS EX STR 15 mL po q6h prn indigestion _____/_____ OXAZEPAM 15-30 mg po qhs prn insomnia _____/_____ ACETAMINOPHEN 650 mg po q4h prn headache _____/_____ MAGNESIUM HYDROXIDE 30 mL po daily prn constipation _____/_____ MAGNESIUM SULFATE Sliding Scale IV daily Call house officer if serum Mg <1.2; hold order for creatinine >1.9 If serum Mg <1.4 give 5 g MgSO4 IV If serum Mg <1.6 give 4 g MgSO4 IV If serum Mg <1.8 give 3 g MgSO4 IV If serum Mg <2.0 give 2 g MgSO4 IV
_____/_____ LAB, MG, K daily _____/_____ KCL IMMEDIATE REL Sliding Scale Target K >4.5 mg/dL po daily Call house officer if K <3.4; hold order for creatinine >1.9 If K <3.7 give 60 mEq If K <4.1 give 40 mEq If K <4.6 give 20 mEq
Additional Orders: ______
9 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
_____/_____ CHEST PAIN PROTOCOL _____/_____ ECG x 1 prn chest pain _____/_____ For CP: check VS, call house officer _____/_____ Mark if cardiac cath is planned: Time ______ _____/_____ NPO except meds Now After midnight _____/_____ LAB, TYPE AND HOLD NEXT AVAILABLE
_____/_____ NUTRITION CONSULT Patient admitted to cardiology ischemia pathway with known or suspected CAD. Please facilitate outpatient education in low- cholesterol, low-salt diet _____/_____ SOCIAL SERVICE CONSULT Patient admitted to cardiology ischemia pathway with known or suspected CAD. Please assess and assist in need for outpatient support (including VNA) services
10 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
DAY 2 OR LATER: REMINDERS
Check/Initial/Date
_____/_____ If on UFH (consult Unfractionated Heparin Dosing Chart) ______ _____/_____ Calcium channel blocker (if β-blocker contraindicated) Drug: ______mg ____times/d
_____/_____ ACE inhibitor or ARB; recommended if diabetic Drug: ______mg ____times/d
_____/_____ Lipid-lowering therapy (statins) regardless of LDL; dose target to LDL <100 mg/dL (further reduction to <70 mg/dL reasonable) Drug: ______mg once daily
_____/_____ Echocardiography. FIRST 24 HR if evidence of CHF, hemodynamic instability, mechanical complication
_____/_____ Warfarin: RECOMMENDED if LV thrombus, extensive wall dyskinesis, LVEF <20%-30%
11 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
PRIOR TO DISCHARGE
Check/Initial/Date _____/_____ Patient had stent implanted OR _____/_____ Patient had medical therapy without stenting
MEDICATIONS _____/_____ Aspirin ______mg/d for ______
_____/_____ Clopidogrel ______mg/d for ______OR _____/_____ Prasugrel 10 mg/d for ______
_____/_____ -blocker Drug: ______Dosage: ______
_____/_____ ACE inhibitor or ARB Drug: ______Dosage: ______
_____/_____ Aldosterone receptor blocker Drug: ______Dosage: ______
_____/_____ Calcium channel blocker Drug: ______Dosage: ______
_____/_____ Statin Drug: ______Dosage: ______
_____/_____ Nitroglycerin Drug: ______Dosage: ______
_____/_____ Drug: ______Dosage: ______
_____/_____ Drug: ______Dosage: ______
12 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
PRIOR TO DISCHARGE cont
PATIENT/FAMILY EDUCATION AND FOLLOW-UP INSTRUCTIONS
Check/Initial/Date
_____/_____ Medication instructions/disease education
_____/_____ Smoking cessation
_____/_____ Diabetes management
_____/_____ Nutrition, weight, and blood pressure management
_____/_____ Exercise program
_____/_____ Referral to cardiac rehab
Time: ______Date: ______Signature: ______a Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50(7):e1-e157. b Some uncertainty exists about optimum dosing of clopidogrel. Randomized trials establishing its efficacy and providing data on bleeding risks used a loading dose of 300 mg orally followed by a daily oral maintenance dose of 75 mg. Higher oral loading doses such as 600 or 900 mg of clopidogrel more rapidly inhibit platelet aggregation and achieve a higher absolute level of inhibition of platelet aggregation, but the additive clinical efficacy and the safety of higher oral loading doses have not been rigorously established. c Kushner FG, Hand M, Smith SC Jr, et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54(23):2205-2241. d Limited data are available for the use of other LMWHs in UA/NSTEMI.
13 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
14 STANDING ORDERS ADMIT – Unstable Angina/Non–ST-Elevation MI (NSTEMI) Based on ACC/AHA 2007 Class I Recommendationsa
Heparin Adjustment Nomogram for Standard Laboratory Reagents With a Mean Control aPTT of 26-36 s
aPTT (s) Bolus Dose Stop Infusion Rate Change Repeat aPTT (U) (min) (mL/h)
<40 3000 0 +2 6 h
40-49 0 0 +1 6 h
50-75 0 0 0 (no change) Next AM
76-85 0 0 –1 Next AM
86-100 0 30 –2 6 h
101-150 0 60 –3 6 h
>150 0 60 –6 6 h aPTT indicates activated partial thromboplastin time. Heparin infusion concentration = 50 U/mL. Target aPTT = 50-75 s.
For aPTTs obtained before 12 h after initiation of thrombolytic therapy: 1. Do not discontinue or decrease infusion unless significant bleeding or aPTT >150 s. 2. Adjust infusion upward if aPTT <50 s. For aPTTs obtained 12 h after initiation of thrombolytic therapy, use entire nomogram: Deliver bolus, stop infusion, and/or change rate of infusion based on aPTT, as noted on appropriate line of nomogram.
Adapted with permission from Hirsh J, Raschke R, Warkentin TE, Dalen JE, Deykin D, Poller L. Heparin: mechanism of action, pharmacokinetics, dosing considerations, monitoring, efficacy, and safety. Chest. 1995;108(4 suppl):258S-275S. Reprinted with permission from Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol. 1996;28(5):1328-1428.
15