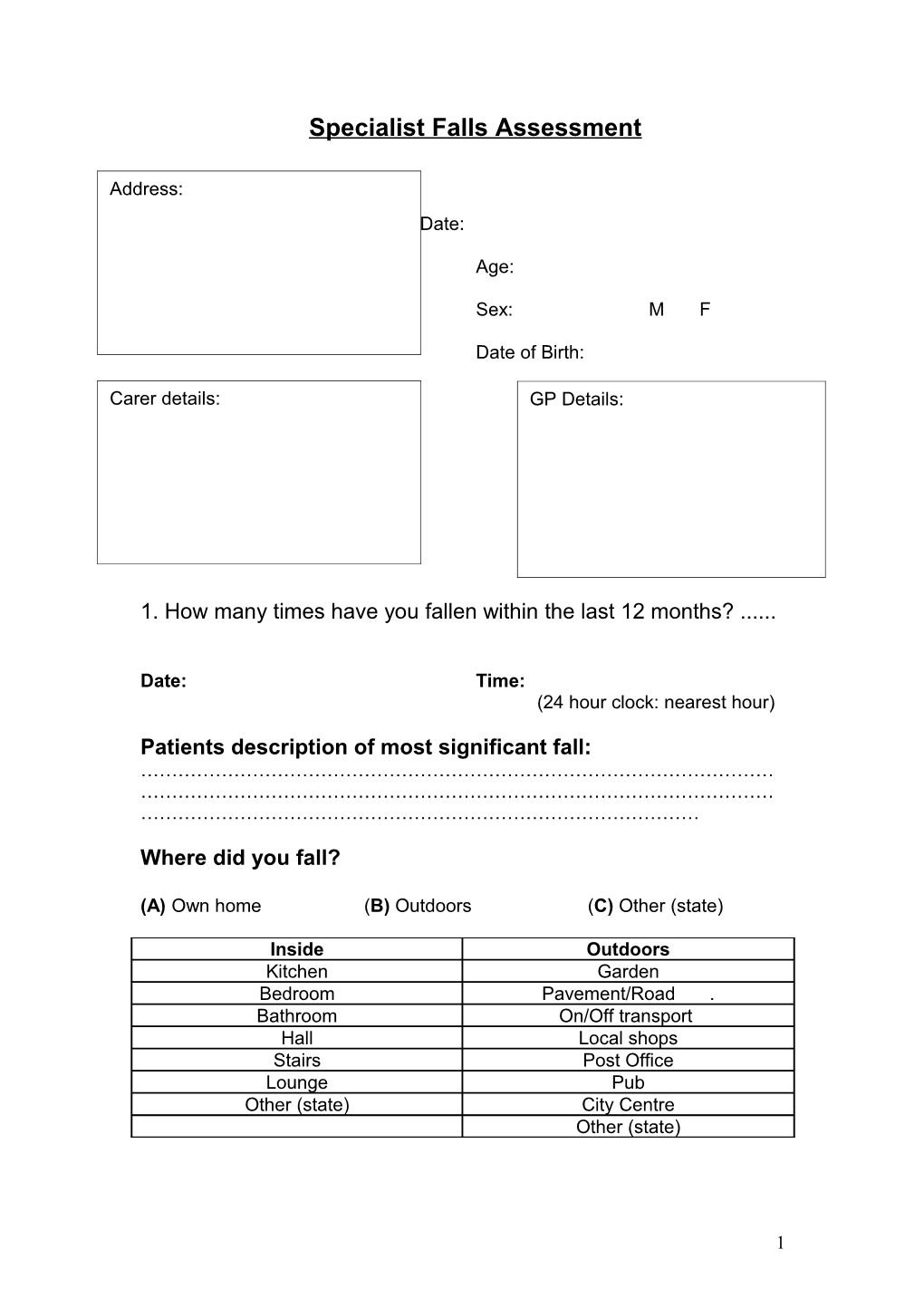
Specialist Falls Assessment
Address:
Date:
Age:
Sex: M F
Date of Birth:
Carer details: GP Details:
1. How many times have you fallen within the last 12 months? ......
Date: Time: (24 hour clock: nearest hour)
Patients description of most significant fall: ………………………………………………………………………………………… ………………………………………………………………………………………… ………………………………………………………………………………
Where did you fall?
(A) Own home (B) Outdoors (C) Other (state)
Inside Outdoors Kitchen Garden Bedroom Pavement/Road . Bathroom On/Off transport Hall Local shops Stairs Post Office Lounge Pub Other (state) City Centre Other (state)
1 How did the fall happen?
Answer questions Y/N:
Did you trip? Y / N Did you slip? Y / N Did you feel dizzy before the fall Y / N Did you were know you were about to fall? Y / N Did you remember falling? Y / N Did you black out? Y / N Were you able to get up unaided? Y / N Do you have a pendent alarm? Y / N If yes, did you use it? Y / N Did you see your GP? Y / N If Yes, how many times? Have you been admitted with a fall? Y / N If Yes, how many times? Did you attend A&E? If no, how did you get up? How long were you on the floor? Approximate tine minutes/hours Did you suffer a fracture? Wrist/clavicle/hip/spine/pubic rami/shoulder(circle) Do you use a walking aid? Did you suffer a soft tissue injury? Do you live alone? Abe to prepare own meals? Are there stairs to your property? Have you got continence issues? Do you have fear of falling?
Activity before the fall?
Inactive Reaching Transferring Walking Up/Dow Turning Just Other / n stairs stood (specify) bending up
Abbreviated Mental Test Score (AMTS)
Place Yes No Person Yes No Time Yes No DOB Yes No Age Yes No Year Yes No 1st Yes No Monarch Yes No 20-1 Yes No W.War Recall Yes No Score 1 point for each Correct answer 8–10 = Normal 5-7 = Moderate Impairment 0-4 = Severe Impairment
Comments
Summary Record/Checklist:
2 Risk factor Y N Interventions Referral Ref Date of Ref & sign History of falling 1 or more in last 12 months Loss of consciousness Dizziness Medications > 4 medications day CNS Suppressants Use of 1 or> for longer than 2 weeks Hypnotics Antidepressants Antipsychotics Cognitive impairment Depression Alcohol Intake > 1 unit per day Postural Hypotension >20mmHG drop between lying & standing BP symptomatic - dizziness Vision Difficulty in reading newspaper/books Difficulty in recognising objects across the room Wear bifocals Cataracts/ Glaucoma/ Macular degeneration Hearing Difficulty in reading Difficulty in conversational speech Tinnitus Walking/Gait Unsteady on feet Shuffles Takes uneven steps House bound Transfers Lack of control when Transferring Synscope Previous stroke Previous orthopaedic surgery Arthritis
3 Continence Balance Needs to hold on to furniture Uses stick/frame Parkinson’s Disease Feet Problems with feet Poor footwear Cognition Any cognitive impairment? AMTS<7/10 MMSE<23/30 Known to have dementia Osteoporosis Smoker Ex-smoker Social Circumstances Carer Coping Receiving attendance allowance Any help at home Are you afraid of falling How spends day
Reflective Practice: 1. Is the person & family aware of the risks? 2. Have I given general lifestyle advice? 3. Have I asked about expectations? 4. Think about the risk of falls & serious injury & immediate priority? 5. Have I asked about drug compliance? 6. Would SMART technology be useful? 7. Have I put person on falls register?
Indications for a Falls Clinic Loss of consciousness with a fall Recurrent falls despite intervention Diagnostic uncertainty gait & balance problems
If yes to any of above, please complete the following:
Pre Falls Clinic Assessment:
4 Weight (Kg): Height (cm):
Measure Yes / No Action
Previous Falls: One or More falls in Previous Yes / No Year
Medications: Four or more excluding Vitamins Yes / No Any Psychotropic Yes / No
Vision: Low Contrast Visual Acuity Test Yes / No Unable to see all of line 16
Peripheral Sensation: Tactile sensitivity Test Yes / No Unable to feel 2 out of 3 trials
Strength/reaction time/balance: Near Tandem stance Test Yes / No Unable to stand for 10 seconds Alternate step Test Yes / No Unable to complete in 10 seconds Sit-to-stand Test Yes / No Unable to complete in 12 seconds :
Number of risk factors 0 1 2 3 4 5+ Total Risk Increase 1 1.4 2.1 4.7 8.7 12
The patient has …………times risk of falling as someone with no risk factors.
TUGT: Time: Steps: Turn steps::
Comments:
MMSE: /30 Less than 24 is abnormal.
5 HAD: A: /21 D: /21 N: 0-7, > 8 needs further assessment.
TFES: /100 A score of > 70 is abnormal.
CVS:
Lying and standing BP: Carotid bruit: Yes/No Right/Left
Lying BP after 5 min. rest:
Standing BP 1 min ………/…….mmHg
Standing BP 3min………../………mmHg
Drop in mmHg : systolic:………. mmHg diatolic:……. mmHg
Postural symptoms yes/no
Visual System:
Visual Acuity:
High Contrast: Low Contrast
Test Distance 1m/3m Test Distance 1m/3m
Lowest line Lowest line Number correct Number correct
Depth Perception:
Score Front Back Front Back
Melbourne Edge Contrast Sensitivity:
Hamilton –Veale Contrast Sensitivity:
Sensory System:
6 Vibration sense: Tibial tuberosity: 128hz tuning fork present/absent
Tactile Sensation: Tested at the right ankle :
Semmes-Weinstein Monofilament: gm pressure/number ......
Proprioception:
1 2 3 4 5
Motor:
Reaction Time: in ms. Trial Hand Foot Practice: Trial Hand Foot 1 1 2 2 3 3 4 4 5 5 6 7 8 9 10
Strength: tested with Dynamometer: kg pressure generated. Best of 3 efforts in the dominant limb tested. (all in kg) force
Knee extension: Knee flexion: Right left Right left
Ankle Dorsiflexion: Right left Hand Grip: Right left
7 Balance:
Posture:
Erect: Yes/No Leaning Backwards: Yes/No
Parkinsonian: Yes/No Hemiplegic: Yes/No
Vestibular:
Truncal Control to external perturbation:
Steady: Yes/No Staggers: Yes/No Begins to fall: Yes/No
Dix Hallpike: Horizontal Rotatory Nystagmus: +ve/-ve Right/Left/Both:
Fukuda steeping: +ve /-ve.
Turned > 45°: Right/Left. Walked forward: yes/No. Distance:
Modified CTSIB: see attached report:
Postural Sway: Standard
Firm EO: Firm EC:
Foam EO: Foam EC:
Limits of Stability:
Coordinated stability:
Postural Sway: Balance Master
8 Mean COG Sway: deg/sec
Firm-EO Firm-EC Foam-EO Foam-EC
COG Alignment: Back Right/Left Forward Right/Left
Limits of Stability:
RT: sec
Forward: Backward Right Left Composite:
MVL:deg/sec
Forward: Backward Right Left Composite:
EPE:%
Forward: Backward Right Left Composite:
MXE:
Forward: Backward Right Left Composite:
DCL:%
Forward: Backward Right Left Composite:
Walk Across: Balance Master:
Step Width:……. Cm Step Length:………cm
Speed: ………….cm/sec Step Length Symmetry:……..%
Gait: Normal/abnormal:
Symmetry Velocity Cadence:
Path deviation: Yes/No. Right/Left.
Type: Hemiplegic: Yes/No High Stepping: Yes/No Right/Left/Both
9 Parkinsonian: Yes/No Gait Apraxia: Yes/No Antalgic: Yes/No
Cerebellar: Yes/No waddling: Yes/No Unclassified: Yes/No
Neurology:
Stroke:
Hemiparesis Yes/No Right/left:
VF defect: yes/no Right/Left Sensory Inattention: Yes/No
Cerebellar signs: Yes/No
Finger Nose: +ve right /left/both Heel shin: +ve. Right/left/both
Interferes with balance and mobility: Yes/No
PD:
Yes/No Well controlled: yes/no
Postural hypotension: Yes/No Symptomatic: Yes/No
Gait instability: Yes/No Truncal Control: Normal/Lost
Freezing: Yes/No On/Off Phenomenon: Yes/No
Peripheral neuropathy:
Yes/No Severity: minimal/moderate/severe
Impairs mobility: Yes/No Impairs Balance: Yes/No
Cervical Myelopathy:
UL Reflexes:
Biceps: +ve/-ve Supinator:+ve/-ve Inverted: +ve/-ve Triceps: +ve/-ve
LL reflexes:
Knee: +ve/-ve/Brisk. Ankle: +ve/-ve/brisk,
Plantar: Flexor/Extensor/Equivocal/Withdrawal Eye Movements:
10 Saccadic: normal/abnormal. Right/Left/Both
Smooth Pursuit: Normal/abnormal Right/Left/Both
Convergence: Normal/abnormal: Right/Left
Visual Fields:
Hemianopia: Yes/No. Right/Left. Inattention: Yes/No. Right/Left
OKN: Normal/abnormal
MSK:
Foot Problems:
Arthritis: Yes/No Right/Left/Both
Flat foot: Yes/No Right/Left/Both Bunions : Yes/No Right/Left/Both
Callus: yes/no Right/Left/Both Ulcer:Yes/No Right/Left/Both Clawing of toes: Yes/No Right/left/both
Amputation of toes: yes/No Right /left: Pain: Yes /No
Impairs Mobility impaired|: Yes/No: Foot Drop: Yes/No Right/Left/Both
Knees:
Right /Left/Both Range of Motion: normal/ restricted Right /Left
Flexion deformity: Yes/No Right/Left/both
Degree of deformity: right left:
Varus /Valgus deformity: Right/Left/Both
Joint instability: yes/no Right/left/Both
Pain: Yes /No Right /Left/Both Impairs Mobility: Yes/No
Hip:
OA: Right/left/Both Pain: Yes/No Right/Left/Both
11 Externally/Internally rotated: Yes/No Right/Left/Both
Impairs Mobility: Yes/No
Limb shortening: Yes/No Right/Left Cm shortening:
Back:
OA: Yes/No Pain Yes/No Impairs Mobility: Yes/No
Restricted movements: Yes/No
Osteoporosis Risk: Ten year Probability of fracture without BMD: %
Major Osteoporotic:
Hip:
Risk factors: Age Sex Weight Height Previous fracture Parent fractured hip Current smoking Glucocorticoids Rheumatoid arthritis Secondary osteoporosis Alcohol 3 or more units/day Bone mineral density (BMD)
Secondary Enter yes if the patient has a disorder strongly associated with osteoporosis. These include type I osteoporosi (insulin dependent) diabetes, osteogenesis imperfecta in adults, untreated long-standing MMSEScore:s hyperthyroidism, /30 hypogonadism or premature menopause (<45 years), chronic malnutrition, or malabsorption and chronic liver disease
Low Contrast visual acuity: Vision is assessed by low contrast visual acuity chart. Acuity is assessed binocularly with the chart at a distance of three
12 meters and the patient wearing their distance glasses if applicable. The patient is asked to read aloud the letters on the chart and must be able to correctly identify all of the letters on the third line from the top to pass the test.
Tactile Sensitivity: peripheral sensation is measured by using tactile sensitivity test at the ankle. A Semmes-Weinstein type pressure aesthesiometer containing a nylon filament is applied to the centre of the lateral malleolus of the ankle on the patient’s dominant side. The patient must keep their eyes closed and indicate to the tester if they are able to feel the monofilament. A total of 3 trials are given and the patient must be able to feel at least two of the 3 trials to pass the test.
Near Tandem Stand: The near tandem stand is a measure of lateral stability. It is a modification of tandem stand test. The subject is asked to stand in a near tandem position, with their feet parallel and separated laterally by 2.5 cm, and the heel of the front foot 2.5 cm anterior to the great toe of the back foot. The subject is require to stand in this position for 10 seconds with their eyes closed. If a score of < 5 is obtained a second trial is allowed. Must stand in this position for ten seconds without moving their feet or opening their eyes in order to pass the test.
Alternate Step Test: Modified version of the stool stepping task, which is one of the 14 components of the Berg Balance scale. It is a practical measure of the requirements of walking and stair climbing and is also a measure of medio-lateral balance. The test involves placing the whole foot onto a step- 19 cm high and 40 cm deep – and alternating right and left feet, four times for each foot, as fast as possible. The time taken(measured in seconds) to complete the eight foot taps is recorded and the patient must complete the task within 10 seconds to pass the test.
Sit - to - stand test: is predominantly a measure of lower limb strength. It involves standing up and sitting down five times from seated position in a 45 cm high chair, with the arms folded in front of the body. The bare-footed subject is asked to perform the five repetitions as quickly as possible to complete the task, measured in seconds, is noted. To pass the test subject must complete the task within 12 seconds.
Proprioception:
• Assessed using a lower-limb matching task. • Proprioception is assessed by asking seated subjects with eyes closed to align the lower limbs on either side a 60cm by 60cm by 1cm thick clear acrylic sheet inscribed with a protractor. • Any difference in matching the great toes is measured in degrees. • After 2 practice trials, an average of five experimental trials are recorded.
Lower-limb strength:
13 • The strength of three leg muscle groups (knee flexors and extensors and ankle dorsiflexors) is measured while subjects are seated. • In each test, there are three trials and the greatest force is recorded. • Performed using a spring gauge attached to the subjects leg using a webbing strap with a velcro fastener or with a handheld dynamometer.
Reaction Time:
• Assessed in milliseconds using a handheld electronic timer and a light as the stimulus & depression of a switch by the finger & the foot as the responses. • The light stimulus is situated adjacent too the response switches and is bright to ensure that the tests are not influenced by the subjects visual acuity. • The timer has a built-in variable delay of 1-5 seconds to remove cues that could be gained from the test administrator commencing each trial by pressing the ‘start’ button. • Five test trials are undertaken, followed by ten experimental trials.
Postural Sway: • Is measured using a sway meter that measures displacements of the body at the waist level. • The device consists of a 40-cm-long rod with a vertically mounted pen at its end. • The rod is attached to the subject by a firm belt and extends posteriorly. • As the subject attempts to stand as still as possible for 30 seconds, the pen records the subjects sway on a sheet of millimeter graph paper fastened to the top of an adjustable height table. • Testing is performed, with eyes open and closed, on a firm surface and on a medium density foam rubber foam mat. • Total sway(number of square millimeter squares traversed by the pen) & A-P & M-L sway are recorded for the 4 tests.
Maximal balance range:
• Subject are asked to lean forward from the ankles without moving the feet, as far as possible. – Point where they can just retain balance. • Lean back as far as possible • Sway-meter attached to the subject at waist level with rod extending anteriorly. • A pen attached to the end of the rod records anterior & posterior movements of the pen on a sheet of graph paper that is fastened to the top of an adjustable-height table. • The score recorded is the maximal A-P excursion of the pen recorded during the three trials.
14 Coordinated stability: • Sway-meter is attached to the subject at waist level with rod extending anteriorly. • The subject is asked to adjust balance by bending or rotating body without moving the feet • The pen on the end of the rod follows & remains within a convoluted track that is marked on a sheet of paper attached too the top of an adjustable-height table. • To complete the test without errors, the pen to remain within the track, which is 1.5 cm wide and adjust the position of the pen 29 cm laterally & 18 cm in the A-P plane. • Total error score is calculated by summing the number of occasions the pen on the sway-meter fails to stay within the path. • When subject fails to negotiate an outside corner, five error points are accrued. • Subject attempts the test twice, with the better trial taken as the test result.
Interpretation of Results:
MET:
15 Excellent 24
Good 20-23 Fair 16-19
Poor 1-15
Depth Perception Performance (cm error):
Excellent < 1 Good 1-2 Fair 2-3 Poor > 3
Low and High Contrast Visual Acuity:
High Contrast Low Contrast Excellent ≤ Line 4 ≤ Line 6 Good Line 5 and Line 6 Line 8 Fair Line 8 and line 10 Line 10, 12, and 16. Poor ≥ Line 12 ≥ Line 20
Touch Thresholds: (filament number / gm pressure):
Good 1-3 Fair 4-5 Poor 6-8
Proprioception: performance (degrees error):
16 Good ≤ 2 Fair 2-4 Poor ≥ 4
Knee Extension:
Performance (Kg) Women Men Excellent >35 >45 Good 20-35 30-45 Fair 15-20 15-30 Poor < 15 < 15
Knee Flexion:
Women Men Excellent > 20 > 25 Good 15-20 20-25 Fair 5-15 5-20 Poor < 5 < 5
Ankle Dorsiflexion:
Women Men Excellent > 15 > 20
17 Good 10-15 10-20 Fair 6-10 -10 Poor < 5 < 5
Reaction Time – Hand:
Performance ms Excellent < 200 Good 200-250 Fair 250-300 Poor > 300
Reaction Time – Foot:
Performance ms Excellent < 250 Good 250-300 Fair 300-350 Poor > 350
Maximal Balance Range
Performance cm Excellent > 22 Good 18-21 Fair 15-18 Poor < 18
Performance Sway: sway area= AP X lateral)
Sway EO Floor Sway EC Floor Sway EO-Foam Sway EC- Foam Excellent ≤ 200 ≤ 300 ≤ 400 ≤ 500 Good 200-400 300-600 400-800 500-1500 Fair 400-800 600-1800 800-1300 1500-3000 Poor ≥ 800 ≥ 1800 ≥ 1300 ≥ 3000
18 Co-ordinated Stability:
Performance Errors:
Excellent ≥ 3 Good 4-8 Fair 8-16 Poor ≥ 16
19