Immunology Notes
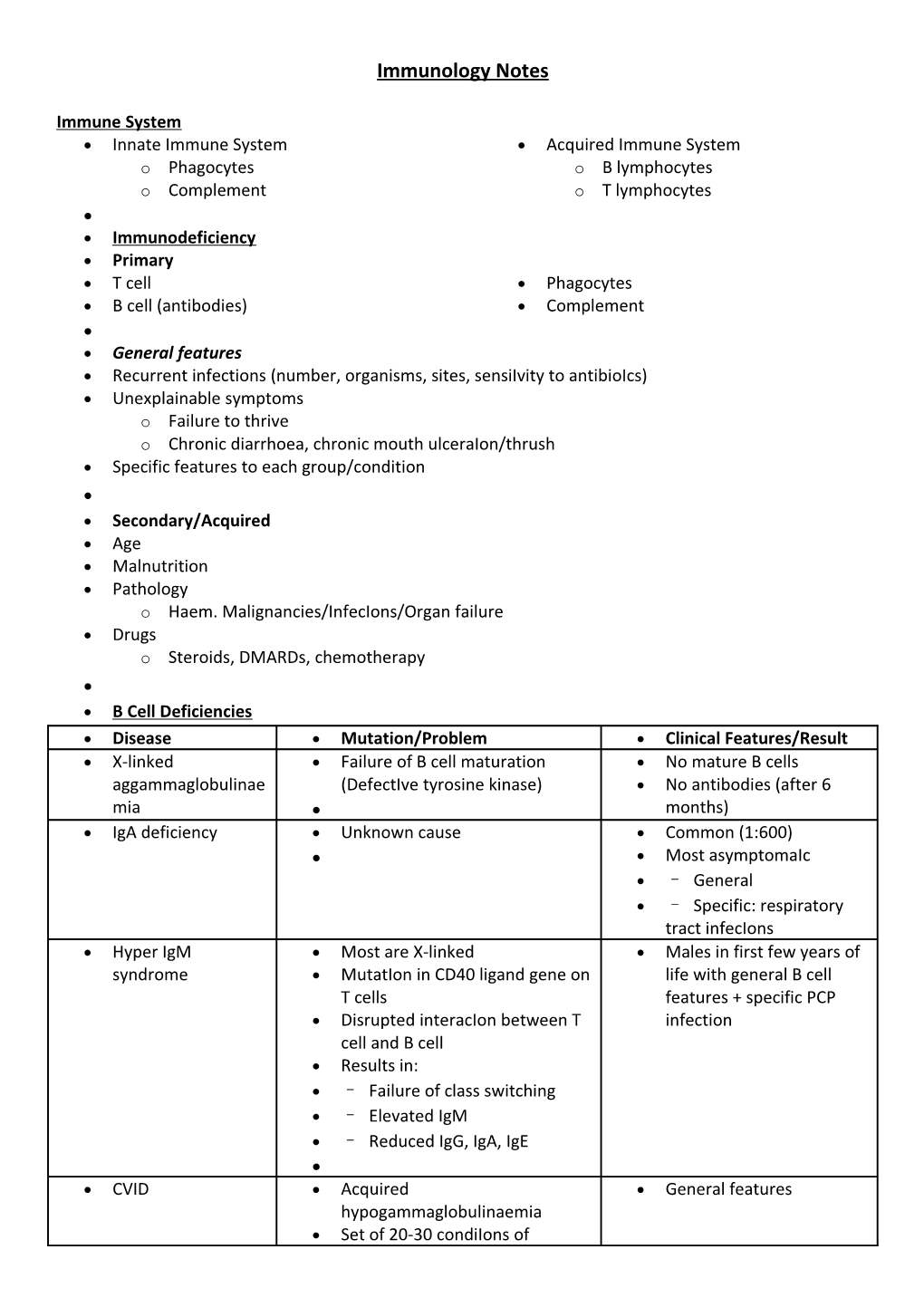
Immune System Innate Immune System Acquired Immune System o Phagocytes o B lymphocytes o Complement o T lymphocytes Immunodeficiency Primary T cell Phagocytes B cell (antibodies) Complement General features Recurrent infections (number, organisms, sites, sensiIvity to antibioIcs) Unexplainable symptoms o Failure to thrive o Chronic diarrhoea, chronic mouth ulceraIon/thrush Specific features to each group/condition Secondary/Acquired Age Malnutrition Pathology o Haem. Malignancies/InfecIons/Organ failure Drugs o Steroids, DMARDs, chemotherapy B Cell Deficiencies Disease Mutation/Problem Clinical Features/Result X-linked Failure of B cell maturation No mature B cells aggammaglobulinae (DefectIve tyrosine kinase) No antibodies (after 6 mia months) IgA deficiency Unknown cause Common (1:600) Most asymptomaIc – General – Specific: respiratory tract infecIons Hyper IgM Most are X‐linked Males in first few years of syndrome MutatIon in CD40 ligand gene on life with general B cell T cells features + specific PCP Disrupted interacIon between T infection cell and B cell Results in: – Failure of class switching – Elevated IgM – Reduced IgG, IgA, IgE CVID Acquired General features hypogammaglobulinaemia Set of 20‐30 condiIons of unknown aeIology Variable reducIon in IgG, IgA and IgE Investigations Lymphocyte counts + serum immunoglobulins Flow cytometry Measure antibody response to known pathogens (tetanus, H.influenza, Strep. Pneumoniae) Management Ig replacement – i.v. every 3‐4 weeks Immunisation is not effective (except IgA) T cell deficiencies General PresentaIon Infections Malignancy o Viral, fungal, mycobacterial Autoimmunity Disease Mutation/Problem Clinical Features/Result DiGeorgeʼs Chromosomal deleIon – 22q11 Cardiac anomalies Syndrome Pathology (Fallot’s) – Failure of thymic development Abnormal facies (low set – Immunodeficiency ears/ • Reduced T cells fish mouth/high forehead) Thymic hypoplasia (T cell • Normal/increased B cells lymphopaenia) • Reduced anIbody response Cleft Palate • Immunodeficiency can improve Hypoparathyroidism with age (hypocalcaemia) Bare L syndrome Deficiency of CD4 cells General features in – Lack of expression of MHC infancy Class II AssociaIon with primary – Normal B cells, reduced sclerosing cholangitis IgG/IgA Wiskott-Aldrich MutaIon in WASP gene Immunodeficiency + syndrome X‐linked Thrombocytopenia & Eczema Lymphoma at a young age Ataxic MutaIon in ATM gene Immunodeficiency + telangiectasia Autosomal recessive Ataxia, Nystagmus & Telangiectasia Lymphomaa/leukaemia at a young age SCID T cell +/‐ B cell problem Infants present by 3 2 important types: months X‐linked - Persistent infections • Mutation of IL‐2 receptor - Failure to thrive (gamma chain) • Reduced T cells/Normal B cells Graft vs. host disease Autosomal recessive – Funny rashes • Adenosine deaminase – Colonisation of bone deficiency marrow with maternal • Reduced T and B cells lymphocytes Phagocyte Deficiencies General Presentation Recurrent deep bacterial + fungal infecIons o Staph. Aureus o Candida albicans o Aspergillus fumigatus Poor response to antibiotics Disease Mutation/Problem Clinical Features/Result Leukocyte Delayed separation of the Adhesion umbilical cord Deficiency (LAD) No adhesion of phagocytes High neutrophils Chronic Granuloma formation Treat with IFN‐gamma Granulomatous No oxidative killing Disease (CGD) Normal or high neutrophil count Kostmannʼs Severe congenital neutropenia No granulocyte precursors syndrome (KS) No neutrophils, abnormal NBT Cyclic Episodic neutropenia neutropenia Investigations Neutrophil count Nitric‐blue test of oxidaIve killing (NBT Presence of leukocyte adhesion markers test) FormaIon of pus Treatment Conservative Definitive o Manage infections aggressively o BMT o Vaccination + septrin/itraconazole o IFN therapy in chronic o Surgical drainage of abscess granulmatous disease Complement deficiencies Allergy Type Mechanisms Examples Type I IgE-mediated Allergies, Asthma hypersensitivity Type II IgG/IgM reactive with self Grave’s disease, antigen Goodpastures Syndrome, Autoimmune haemolytic anaemia Type III Immune Lupus, Polyarteritis complexmediated damage Nodosa Type IV T-cell mediated Rheumatoid, IDDM, MS, damage/delayed Transplant rejection hypersensitivity Clinical Features Primary Delayed o Skin changes o Onset 2‐24 hours after exposure, o Smooth muscle contraction o Lasts many days (lungs/gut) o Inflammatory cell infiltration o Mucus secretion (lungs) (associated tissue damage) o Vascular permeability (shock) Investigations RAST o Quantity of IgE to proposed antigen o Less sensitive and specific cf. skin prick o Useful for dermatographism; Hx of anaphylaxis; cannot stop antihistamine Mast Cell Tryptase o During an acute episode (1‐6 hours after) Skin Prick Testing o Gold standard test o Rapid; cheap; sensitive; specific o Safe (relatively) o Anti‐histamines stopper prior to testing o Ineffective in food allergies Management Avoidance of allergen Supportive (bronchodilators/adrenaline/fluids) Drugs o Block MC activation – sodium chromoglycate o H1‐receptor antagonists – antihistamines o Anti‐inflammatory – corticosteroids o Leukotriene receptor antagonist ‐montelukast Allergen specific immunotherapy Autoimmunity Hypersensitivity Inappropriate immune reaction that produces Issue damage on exposure to an antigen Autoimmune Disease Immune reaction produces Issue damage due to a reaction against self‐protein Breakdown in self‐tolerance Central tolerance – failure to delete autoreactive T cells in thymus/ B cells in bone marrow Peripheral tolerance – reactivation of weakly autoreactive T/B cells, Inflammation, infection, tissue damage ANA’s Autoimmune Disease’s Disease Auto-antibodies Features SLE Anti-sm F:M = 9:1 Anti Ro Serositis, Oral ulcers, Arthritis, Anti-LA Photosensitivity, Blood changes, Renal Anti-dsDNA involvement, ANA, Immunological changes, Neuro stuff, Malar rash, Discoid rash Drug-induced Anti-Histone – Procainamide lupus – Hydralazine – Isoniazid – Clindamycin Sjogrenʼs Ant-LA Syndrome Anti-Ro RA Anti-CCP Diffuse Anti-SCL 70 CREST + Pulmonary fibrosis, Renal Scleroderma disease, Polyarthritis, Myopathy/muscle atrophy Limited Anti-centromere Calcinosis, Raynauds Phenomenon, Scleroderma/CRE Osephageal dismotility, Sclerodactyly, ST Telangectasia Dermatomyositis Anti-Jo-1 / polymyositis Wegnerʼs C-ANCA granulomatosis Pernicious 90% anti‐parietal cell Autoimmune attack on parietal cells - anaemia antibodies atrophic gastritis & lack of intrinsic 50% anti‐IF antibodies factor ↓serum vit. B12 Associations: other autoimmune disease, gastric adenocarcinoma Graveʼs disease Anti‐TSH receptor Low TSH antibodies Elevated free T4 (if T4 normal – Anti‐thyroid eroxidase/ consider T3) anti‐thyroglobulin AB Hashimotoʼs Anti‐microsomal Autoimmunne destruction of thyroid thyroiditis Anti‐thyroglobulin Diffuse lymphocyte infiltraIon Anti‐peroxidase High TSH Firm goitre → atrophy Mixed Anti-RNP Connective tissue disease Anti- Anti-Cardiolipin phospholipid syndrome Autoimmune Autoantibodies →RBC haemolysis Haemolytic Features of haemolysis Anaemia Raised unconjugated bilirubin ↓ haptoglobin ↑LDH ↑ urinary urobilinogen Reticulocytes Positive DAT test Addisons Disease ↑Potassium ↓Sodium Vasculitides Inflammation of blood vessels, cause is largely unknown Disease Vessels Features Affected Temporal arteritis Large Affects carotids and temporal arteries (Giant cell arteritis) 2:1 (F:M), > 50yrs Headache and tender over scalp “combing” Risk of blindness Takayasu’s Large Affects aorta and vessels coming off it Asian women 20s – 30s Difference in blood pressure between arms Polyarteritis Medium Affects many organ system nodosum Symptoms are often nonspecific Classically affects renal vessels and coronary arteries Kawasaki’s Medium Affects Children ? secondary to infection - Fever for more than 5 days -Erythema/desquamation of palms and soles - Cervical lymphadenopathy - Conjunctivitis - Changes to lips/oral cavity = dry, swollen, strawberry tongue - Erythematous rash Wegener’s Small Midline structures cANCA +ve Epistaxis, Pulmonary pain, saddle nose nodules, haemoptysis, Glomerulonephritis Churg‐Strauss Small Late onset asthma, eosinophilia Primarily the lung Gut, kidney or nerve involvement cANCA or pANCA +ve Microscopic Small Huge number of systems affected polyangitis pANCA +ve Mononeuritis Multiplex, Haemoptysis, Renal failure, Skin rash Transplantation Timefra Pathophysiology Treatment me Hyperacute Minutes Pre‐existing anti‐ None once it occurs rejection to hours donor antibodies Blood groups and Massive inflammatory HLA to detect pre‐ vasculitis→ graft existing antibodies thrombosis Acute cellular Days to Recognition of CD4 Partially treated with rejection 1 month cells → activation of immunosuppressive CD4 cells → type IV therapy hypersensitivity response Unwell, reduction in graft function, pain/tenderness Acute vascular 1‐2 Mediated by Immunosuppresion rejection weeks antibodies Results in post‐ vasculitis + transpla thrombosis nt Chronic allograft > 30 Major cause of graft Manage atherogenic rejection days loss affects all types risk post‐ of solid Drugs with low transpla organ transplant toxicity nt Risk factors: - Repeated acute rejection episodes - Pro‐atherogenic factors - Drug toxicity - Non‐compliance with medication Therapeutics in Immunology Class Examples Effects Side effects Steroids Prednisolon ↓ Phagocyte Cushingoid sx e recruitment Hydrocortis ↑WCC (neutrophils) one Lmyphocyte Dexametha SequestraIon, sone cytotoxicity, reduced cytokine gene expression Antiproliferative Azathioprin Block Purine synthesis Danger of agents e (T>B) marrow Cyclophosp Blocks DNA replication suppression hamide (B>T) Haemorrhagic Mycopheny cystitis late mofetil Inhibitors of cell Ciclosporin NephriIs signalling Tacrolimus Diabetes Gingival hypertrophy Antibodies to cell OKT3 (anti- OKT3 - prevention and surface CD3 treatment of solid antigens antibody) organ transplant Anti-IL2 rejection antibody CD25 - rejecIon (CD25) prophylaxis in transplantaIon Anti-cytokine Infliximab Infliximab - murine agents Etanercept anti‐TNF antibody Adalimuma Etanercept - human b soluble TNF receptor Adalimumab - human anti‐TNF antibody