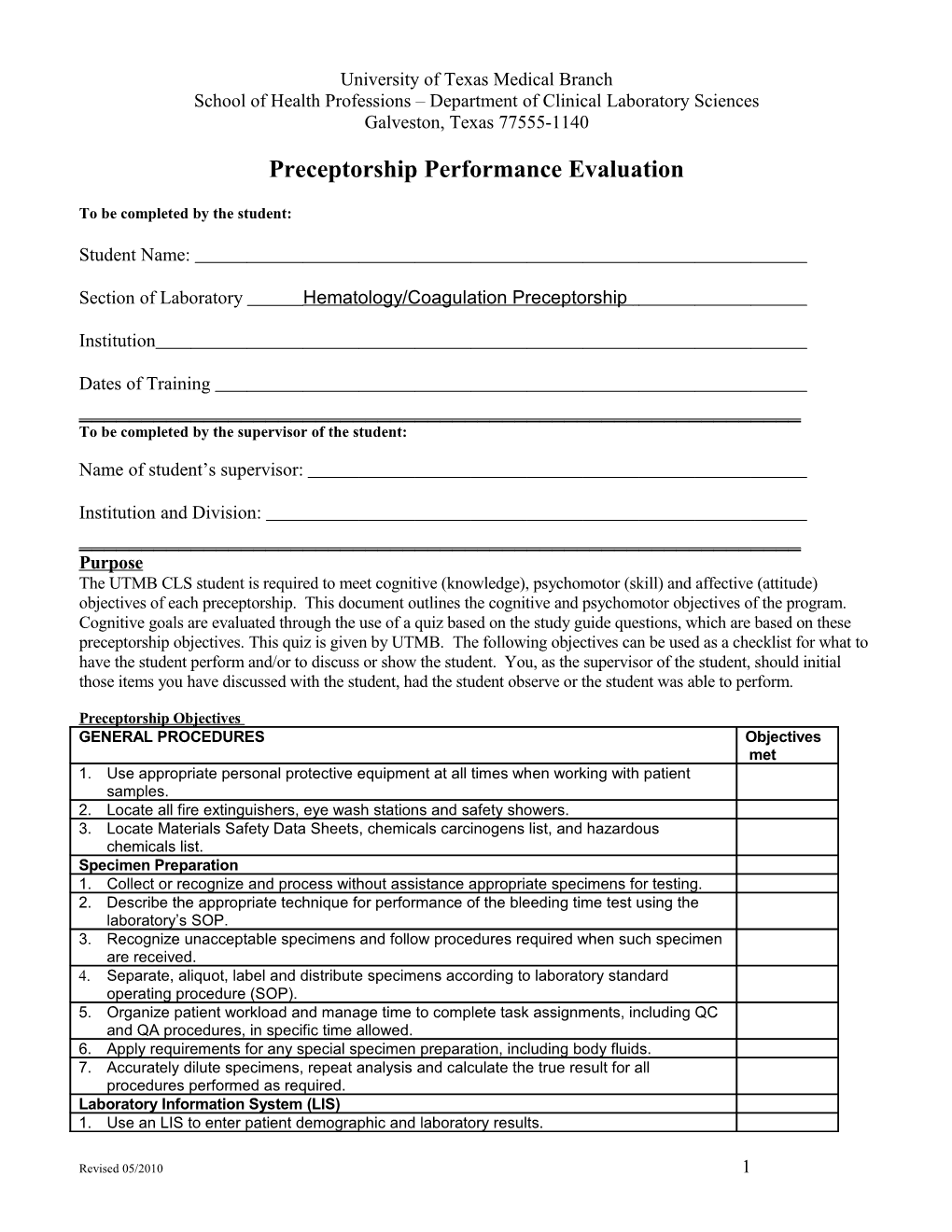
University of Texas Medical Branch School of Health Professions – Department of Clinical Laboratory Sciences Galveston, Texas 77555-1140
Preceptorship Performance Evaluation
To be completed by the student:
Student Name:
Section of Laboratory Hematology/Coagulation Preceptorship
Institution
Dates of Training ______To be completed by the supervisor of the student:
Name of student’s supervisor:
Institution and Division: ______Purpose The UTMB CLS student is required to meet cognitive (knowledge), psychomotor (skill) and affective (attitude) objectives of each preceptorship. This document outlines the cognitive and psychomotor objectives of the program. Cognitive goals are evaluated through the use of a quiz based on the study guide questions, which are based on these preceptorship objectives. This quiz is given by UTMB. The following objectives can be used as a checklist for what to have the student perform and/or to discuss or show the student. You, as the supervisor of the student, should initial those items you have discussed with the student, had the student observe or the student was able to perform.
Preceptorship Objectives GENERAL PROCEDURES Objectives met 1. Use appropriate personal protective equipment at all times when working with patient samples. 2. Locate all fire extinguishers, eye wash stations and safety showers. 3. Locate Materials Safety Data Sheets, chemicals carcinogens list, and hazardous chemicals list. Specimen Preparation 1. Collect or recognize and process without assistance appropriate specimens for testing. 2. Describe the appropriate technique for performance of the bleeding time test using the laboratory’s SOP. 3. Recognize unacceptable specimens and follow procedures required when such specimen are received. 4. Separate, aliquot, label and distribute specimens according to laboratory standard operating procedure (SOP). 5. Organize patient workload and manage time to complete task assignments, including QC and QA procedures, in specific time allowed. 6. Apply requirements for any special specimen preparation, including body fluids. 7. Accurately dilute specimens, repeat analysis and calculate the true result for all procedures performed as required. Laboratory Information System (LIS) 1. Use an LIS to enter patient demographic and laboratory results.
Revised 05/2010 1 Quality Assurance 1. Accurately and legibly log in and maintain required records at all times. Pipet accurately at all times 2. Reconstitute control sera and standards with accuracy and reliability without direct supervision 3. Perform quality assurance procedures for each test analysis and consistently maintain required documentation. 4. Evaluate quality control data, recognize out-of-control data and perform troubleshooting measures according to laboratory policies for all laboratory procedures 5. Apply Westgard rules to quality control decisions, recognize out-of-control situations, and perform actions outlined in the SOP when these situations occur. 6. Determine and implement the course of action to be taken when delta checks are not correlated. 7. Recognize test results that need to be checked by repeat testing and those that are beyond the limits of linearity and perform procedures as defined by SOP when these occur.
Reference Ranges 1. Recognize reference ranges, therapeutic ranges, and critical values and perform procedures at all times that are required by the SOP when these occur
AUTOMATION Hematology 1. State the principle of operation and method of determination, for the instrument(s) utilized in the laboratory in which you are rotating, for each of the following: Cell counts (white cell, red cell, platelets, and reticulocytes [where appropriate]) Cell identification Hemoglobin Hemactocrit Red cell indices RDW. 2. Compare impedance and photo-optical methods for counting cells. 3. For each of the tests listed below, perform/describe (NOTE: as appropriate for the rotation laboratory) the procedure, including reagent and control preparation, state the normal range and panic values: Cell count Hb Hct Red cell indices RDW ESR Reticulocyte count 4. Observe/perform maintenance on the primary automated cell counter/analyzer, microhematocrit centrifuge, automated ESR [where appropriate]. 5. Given an error code or common instrument malfunction, find the appropriate trouble-shooting information and discuss the action to be taken. Hemostasis 1. State the principle of operation and method of clot detection for the instrument(s) utilized in the laboratory in which you are rotating. 2. Compare and contrast optical vs. elctromechanical methods for clot detection. 3. For each of the tests listed below, perform/describe (NOTE: as appropriate for the rotation laboratory) the procedure, including reagent and control preparation, state the normal range and panic values, and describe the portion of the hemostatic mechanism being tested: Prothrombin time Activated partial thromboplastin time Fibrinogen FDP Revised 05/2010 2 D-dimer Factor assays Mixing/correction studies Bleeding time Platelet aggregation studies 4. Observe/perform maintenance on the primary coagulation instrument. 5. Given an error code or common instrument malfunction, find the appropriate trouble-shooting information and discuss the action to be taken. MORPHOLOGY 1. Recognize, identify and grade [where appropriate], according to laboratory standard operating procedure (SOP), the following in peripheral blood smears (criteria for evaluation – differentials and morphology grade within 20% of predetermined values: Normal mature cells Immature cells of each cell line Red cell inclusions Red cell abnormal shapes and sizes (e.g., anisocytosis, poikilocytosis, dacryocytes, ovalocytes, microcytes, etc.) White cell inclusions Abnormalities of white cell structure 2. Recognize, identify and grade [where appropriate], according to laboratory standard operating procedure (SOP), the following in various body fluid smears: Normal mature cells Immature cells of each cell line Abnormal cells (e.g., tumor cells, L.E. cells, disease specific cells, etc.) Abnormalities of white and red cell structure
BODY FLUIDS
1. Discuss the technique for preparation of body fluids for performance of cell counts and differentials. 2. Perform/observe preparation of body fluids for performance of cell counts and differentials. 3. Discuss special stains that may be performed on body fluids to detect cells and inclusions that are indicative of certain disease states. 4. Perform cell counts with 100% accuracy and differentials within 20% of the predetermined values on body fluids.
BONE MARROW
1. Explain the procedure used for collection of bone marrow samples, including sites, types of sample processing, and preparation of smears. 2. Describe the principle and method for the special stains listed below: LAP Prussian blue peroxidase, Sudan Black B non-specifc and specific esterase dual esterase PAS TRAP 3. Compare the staining properties of each of the stains listed above and the utility of the stains in identifying specific cell types.
Revised 05/2010 3 Scale: 3 = exceeds entry level requirements (>80%) – produces work of high quality 2 = Meets entry level requirements (70%) – requires little duplication of instruction and makes few errors 1 = does not meet entry level requirements (<70%) - improvement needed.
) ) y
l l r s
Criteria: please circle the box which you feel represents this % % e e t t 0 0 v v n n 8 7 e e e e ( l student’s ability during and/or after this preceptorship rotation. l
>
t ( s m y ) y e t e s r r e n t r t t % i e n n n m 0 u e e e m 7
q T s e s m < e t r ( d e O i e R e r
e u i N l e
q u e c s M e v x q e r e e o E l R D
Technical Knowledge and Competence 1. Recalled the scientific principles of laboratory test procedures 3 2 1 2. Discussed technical and procedural concepts 3 2 1 3. Detected the need for and used problem solving procedures 3 2 1 4. Integrated and practiced safety regulations 3 2 1 5. Explained the principles of quality assurance and quality control 3 2 1 6. Discussed scientific information and the application of principles 3 2 1 as they related to tests performed/sent to reference lab by this area. 7. Recognized abnormal laboratory data and made correlations with 3 2 1 associated pathology 8. Confirmed the validity of test results and selected additional test 3 2 1 procedures 9. Performed and interpreted diagnostic tests with accuracy 3 2 1 10. Used quality control procedures 3 2 1 11. Calibrated instruments or determined QC requirements for 3 2 1 instruments. 12. Evaluated computer generated data 3 2 1 13. Effectively analyzed malfunctions and trouble shoots instruments 3 2 1 and/or procedures 14. Selected appropriate samples and test methods 3 2 1 15. Selected appropriate reagents/ blood products and instruments. 3 2 1 16. Evaluated laboratory Data 3 2 1
Revised 05/2010 4 Please indicate your appraisal of the individual’s performance as a clinical laboratory science professional by checking one box:
EXCELLENT [ ] Average [ ] Below Average [ ]
Please provide examples of any marks of “Does not meet entry level Requirements” level 1 and/or any other comments you would like to make about this student:
Supervisor: Please sign below. Thank you for you appraisal of this student’s experience at your facility.
Signature: Date:
This evaluation may be given to the student to give to the Education Coordinator at UTMB or you may mail or fax:
University of Texas Medical Branch School of Health Professions Clinical Laboratory Sciences Department Preceptorship Coordinator 301 University Blvd Galveston, Texas 77555-1140
Fax: 409-772-9470
Revised 05/2010 5