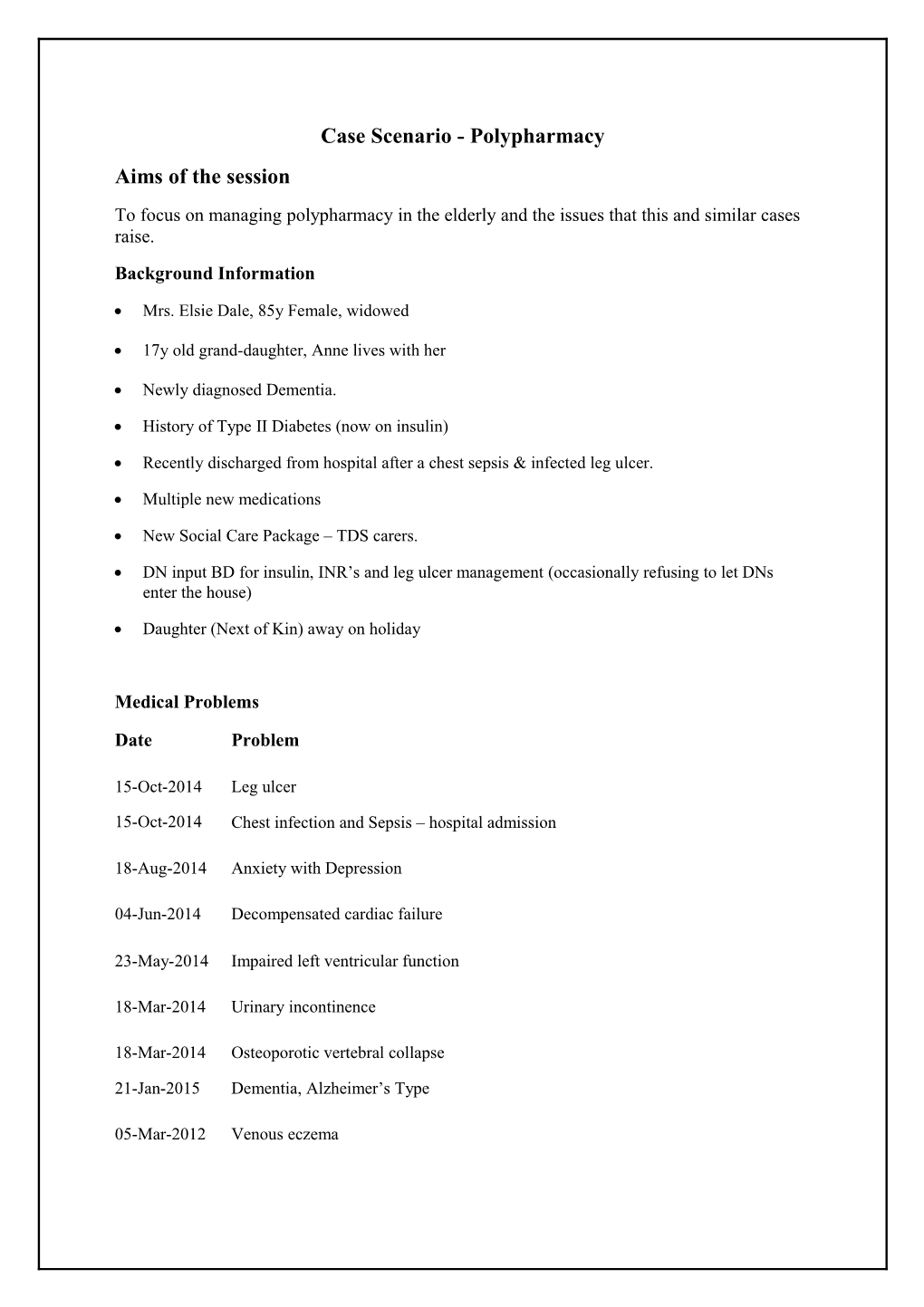
Case Scenario - Polypharmacy Aims of the session To focus on managing polypharmacy in the elderly and the issues that this and similar cases raise. Background Information
Mrs. Elsie Dale, 85y Female, widowed
17y old grand-daughter, Anne lives with her
Newly diagnosed Dementia.
History of Type II Diabetes (now on insulin)
Recently discharged from hospital after a chest sepsis & infected leg ulcer.
Multiple new medications
New Social Care Package – TDS carers.
DN input BD for insulin, INR’s and leg ulcer management (occasionally refusing to let DNs enter the house)
Daughter (Next of Kin) away on holiday
Medical Problems
Date Problem
15-Oct-2014 Leg ulcer
15-Oct-2014 Chest infection and Sepsis – hospital admission
18-Aug-2014 Anxiety with Depression
04-Jun-2014 Decompensated cardiac failure
23-May-2014 Impaired left ventricular function
18-Mar-2014 Urinary incontinence
18-Mar-2014 Osteoporotic vertebral collapse
21-Jan-2015 Dementia, Alzheimer’s Type
05-Mar-2012 Venous eczema 16-Jan-2012 Paroxysmal AF – Anticoagulation started
12-Jun-2010 Exacerbation of COPD- admitted to hospital
03-Nov-2009 Knee osteoarthritis NOS
31-Jan-2007 Chronic kidney disease stage 3
08-Dec-2005 Type 2 Diabetes Mellitus
11-Dec-2002 COPD
07-Jun-2002 Urge incontinence pelvic floor exercises- cystoscopy showed irritative bladder
27-Feb-2002 Essential hypertension
16-Dec-2001 Gout
Medications Acute Drug Dosage Quantity Ibuprofen 400mg One To Be 56 tablet Three Times Daily PRN Repeat
Drug Dosage Quantity
Bisoprolol 1.25mg One To Be Taken 56 tablet tablets Daily 100 tablet Warfarin 5mg ASD 100 tablet Warfarin 3mg ASD
Aspirin 75mg tablets One To Be Taken 56 tablet Daily
Bumetanide 1mg One To Be Taken on 28 tablet tablets Alternative Days
Omeprazole 20mg One To Be Taken Each 56 capsule gastro-resistant Morning capsules Citalopram 10mg One To Be Taken 56 tablet tablets Daily
Zerobase 11% cream Use PRN 500 gram
Atorvastatin 10mg tablets One To Be Taken Daily 56 tablet
Laxido Orange oral powder sachets 1 sachet mixed with water SD 90 sachet Donepezil 10mg tablets 1 to be Taken Daily 56 tablets Hydroxyzine 10mgs tablets 1 to be Taken at night 56 tablets Ramipril 5mgs tablets 1 to be Taken Daily 56 tablets Co-codamol 8/500 tablets 1-2 tablets QDS PRN 112 tablets Novomix 30 flexpen 22u am/ 18u pm 100units/mls Freestyle light testing strips ASD 50 strips Salbutamol 100mcgs/dose inhaler 2 puffs prn/qds 1 inhaler Tiotropium bromide 180mcg inhalation powder capsule 1 capsule daily 56 capsules Metformin 500mgs tabs 1 to be Taken TDS 168 tablets Diazepam 2mg 1 TDS PRN 28 tablets Allevyn Gentle Border ASD 20dressing Dressing 15cm x 15cm Aquacel Ag Dressing 5cm x 5cm ASD 5 dressing Tubigrip Elasticated Support Bandage Stockinette 10cm x1m ASD 3m Allopurinol 100mg 1 to be Taken Daily 56 tablets Solifenacin 5mg 1 to be Taken Daily 56 tablets Past Medication Gliclazide 80mgs tabs 1 to be Taken BD 56 tablets Last investigations (1 month ago): HBA1c: 78, U&E: Na 133, K 5.1, Ur 11.2, Cr 132, eGFR: 56 ml/min Stage 3 FBC: Hb 11.2, MCV 78, Plt 156, WCC 4.9 INR (3 weeks ago): 3.2. (Patient refused INR blood test due 1w ago) Other healthcare information
Pharmacy Notes: Elsie’s notes red-flagged at the pharmacy as not ordering repeat medications regularly
Hand held social care notes record that seems doesn’t always take her medication as prescribed and sometimes won’t let carers in or eat the food they prepare.
DNs records – slow healing ulcer, using dressings advised by hospital on discharge; sometimes refuses BMs, insulin and INRs
Areas for Discussion/Decision Making 1) In a patient who has newly been diagnosed with dementia, what issues does the list of medication raise? 2) How would you ensure compliance? 3) Who else would you like to be involved in the management of this patient’s medications? 4) Are there any medications that you would consider stopping? How would you organise it? 5) Which tablet/s do you think Mrs Dale would be most and least willing to stop? Please discuss the pros and cons of each decision above 6) What other questions/anxieties has this case and discussion raised for you? Further Discussion (Time permitting) 1 week later the GP on-call visits the patient following a request from the DN who visited her earlier in the day concerned that the patient has developed diarrhoea and vomiting. Entry from EMIS records from visiting GP: Problem Viral Gastroenteritis History 2d hx of vomiting with loose brown stool, says no blood, no abdo pain, initially feverish, now settled. Taking insulin although ?missed insulin last night as refused to let carer and DN into the house. Says stopped vomiting, now only loose stool x5-6/day, no mucus. No hx of diverticulitis. No wt loss, reduced eating since being unwell, drinking better now, says passing urine, able to produce sample Examination Pleasantly confused 8/10, Temp 37.4, pulse 66 bpm, irreg, BP 106/64 BM 18.6 Abdo – soft, non-tender. No peritonism. BS N, PR refused. Urinalysis – Ketones trace, nil else Comments Imp: Viral Gastroenteritis DNs to watch BMs, patient encouraged to drink plenty fluids
Area for Discussion
What medications would you stop/change during this acute illness and how would you ensure that this happens?