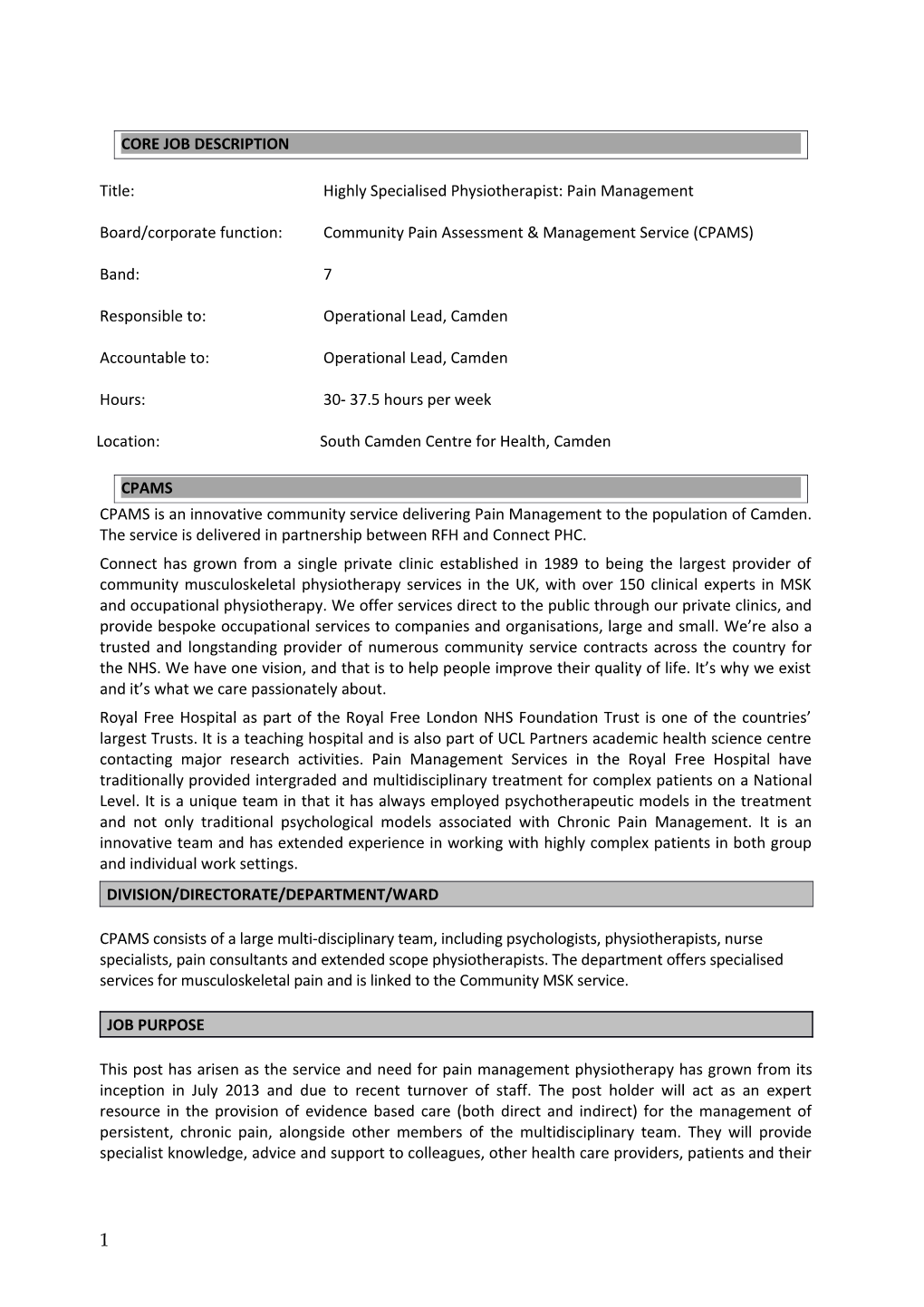
CORE JOB DESCRIPTION
Title: Highly Specialised Physiotherapist: Pain Management
Board/corporate function: Community Pain Assessment & Management Service (CPAMS)
Band: 7
Responsible to: Operational Lead, Camden
Accountable to: Operational Lead, Camden
Hours: 30- 37.5 hours per week
Location: South Camden Centre for Health, Camden
CPAMS CPAMS is an innovative community service delivering Pain Management to the population of Camden. The service is delivered in partnership between RFH and Connect PHC. Connect has grown from a single private clinic established in 1989 to being the largest provider of community musculoskeletal physiotherapy services in the UK, with over 150 clinical experts in MSK and occupational physiotherapy. We offer services direct to the public through our private clinics, and provide bespoke occupational services to companies and organisations, large and small. We’re also a trusted and longstanding provider of numerous community service contracts across the country for the NHS. We have one vision, and that is to help people improve their quality of life. It’s why we exist and it’s what we care passionately about. Royal Free Hospital as part of the Royal Free London NHS Foundation Trust is one of the countries’ largest Trusts. It is a teaching hospital and is also part of UCL Partners academic health science centre contacting major research activities. Pain Management Services in the Royal Free Hospital have traditionally provided intergraded and multidisciplinary treatment for complex patients on a National Level. It is a unique team in that it has always employed psychotherapeutic models in the treatment and not only traditional psychological models associated with Chronic Pain Management. It is an innovative team and has extended experience in working with highly complex patients in both group and individual work settings. DIVISION/DIRECTORATE/DEPARTMENT/WARD
CPAMS consists of a large multi-disciplinary team, including psychologists, physiotherapists, nurse specialists, pain consultants and extended scope physiotherapists. The department offers specialised services for musculoskeletal pain and is linked to the Community MSK service.
JOB PURPOSE
This post has arisen as the service and need for pain management physiotherapy has grown from its inception in July 2013 and due to recent turnover of staff. The post holder will act as an expert resource in the provision of evidence based care (both direct and indirect) for the management of persistent, chronic pain, alongside other members of the multidisciplinary team. They will provide specialist knowledge, advice and support to colleagues, other health care providers, patients and their
1 CLINICAL PRACTICE carers on all aspects of pain management. The successful candidate will work closely with team members, especially psychologists seeing patients both individually and within groups.
DIMENSIONS
A Pain Management Programme for 12 patients approximately 4 programmes per year run by a psychologist and physiotherapist. Other to the group work the successful candidate will be holding regular, weekly clinics for one to one sessions for the patients not eligible for group work or who need some preparation before a pain management programme.
SPECIALTY - Area specific job requirements*
to work autonomously at a highly specialised level in the management of people with pain, seeking advice where necessary from peers and colleagues within CPAMS and beyond to be responsible for delivering a high standard of service for patients who have been referred to CPAMS to be update with current practices in the field and have an awareness of cognitive behavioural treatment, acceptance and commitment therapy and compassionate treatment models to participate in special interest groups or other relative professional bodies to have experience in the set up and running of pain management programmes to be responsible for delivering physiotherapy as a part of the pain management programme in col- laboration with the clinical psychologists To be responsible for the continuous development of the pain management programme in collabor- ation with the clinical psychologists to undertake the advanced and specialised assessment and management of patients referred to CPAMS using a biopsychosocial model to work with chronic pain patients in setting value based goals and planning towards them to engage chronic pain patients with regular exercising and enable them to regulate their activity levels, possibly by developing individualised exercise and activity programmes informed by relevant psychological principles (cognitive behavioural model, compassion treatment model, acceptance and commitment model) to provide patient education on such topics as body mechanics, anatomy, pathophysiology and help- ful pain management strategies to deliver evidence based healthcare where possible to take an active role within the multidisciplinary team, in discussing patients’ clinical management to attend and actively participate in any clinics, meetings and seminars as appropriate to maintain an accurate and evaluative record keeping system to be able to exert moderate physical effort during the working week in order to deliver treatment, for demonstration, and for organisation of equipment to be able to cope with a stressful working environment with intense concentration and the man- agement of distressed people with challenging behaviours.
KEY RESULT AREAS
2 To monitor and maintain health, safety and security of self and others in own work area through ensuring own and others knowledge of appropriate national / local policies and procedure, and that these are adhered to To maintain own and others’ knowledge of appropriate professional standards and Trust professional guidelines and that these are applied to practice To act as a role model in promoting peoples’ equality, diversity and rights through ensuring that own and others practice is the best interests of users To receive direct referrals within the speciality and to provide expert assessment of patients’ needs To work in partnership with physiotherapists and other health professionals to address people’s health needs through planning and delivering interventions which are based on best practice and clinical judgement To delegate and refer to other practitioners when this will improve health outcomes or when risks and needs are beyond own competence and scope of practice To support patients in the delivery of care through maintaining the patients information needs, promoting their wishes and beliefs, and addressing their concerns To support patients in meeting their own health and wellbeing through providing expert information, advice and support To monitor and review the effectiveness of interventions with the patient and colleagues and modify this to meet changing needs and established goals of care. To identify objectives for own professional development which reflect local needs To act as a resource to others in developing and improving knowledge and skills in clinical practice, through acting as an assessor, teacher and facilitator To contribute to the development of practice knowledge within the speciality through internal and external presentation and publication. To promote a learning environment through identifying opportunities and seeking resources required for own and others learning To provide specialist input to professional development programmes. To reflect on own practice through clinical supervision / mentorship and to act as a clinical supervisor / mentor to others To maintain own and others’ awareness of relevant research evidence related to the speciality and work with others in applying this to practice. To maintain and manage own caseload To identify areas of potential research relating to the speciality and to participate in relevant research activities To develop evidence based standards, policies and guidelines at a local, network and national level to improve the practice of own and other professions To evaluate clinical effectiveness within the speciality, identifying poor quality and a plan for quality improvement To support quality improvement through offering advice and support to others. To develop and maintain others’ awareness of role within the speciality, the organisation and local networks and maintain mechanisms for contact and referral To review and evaluate services collaboratively with own and other professions and users, identify- ing areas for service development To facilitate service changes collaboratively with the multi-disciplinary team to make best use of re- sources, improve practice and health outcomes in line with local and national best practice.
To lead in the implementation of national policy and practice initiatives and to implement these at a local level within the speciality To provide expert advice and support to colleagues internally and externally within speciality
3 To ensure that appropriate information is disseminated within the speciality, the organisation and within external agencies and forums. To develop and maintain partnership working with other practitioners, local and national bodies and forums To identify, develop and sustain mechanisms to support patient involvement and feedback. To participate in developing a shared vision of the service and work with the multi-disciplinary team, organisation and external agencies to achieve this To negotiate and agree with individuals, groups and other practitioners’ outcomes, roles and responsibilities, and action to be taken to develop resources, services and facilities To maintain appropriate channels and styles of communication to meet the needs of patients, relatives and carers, managers, peers and other professions / agencies. To employ effective decision making skills to address complex issues and use effective change management skills to implement these To use effective prioritisation, problem solving and delegation skills to manage time effectively To establish networks with other specialists at a local, national and international level, to exchange and enhance knowledge and expertise.
GENERAL
Adopt a professional approach to customer care at all times. To treat staff, patients, colleagues and potential employees with dignity and respect at all times. To take personal responsibility for promoting a safe environment and safe patient care by identifying areas of risk and following the Incident, Serious Incidents and Near Misses reporting policy and procedure. To take personal responsibility for ensuring that resources are used efficiently and with minimum wastage. To comply with policies for personal and patient safety and for prevention of healthcare- associated infection (HCAI); this includes a requirement for rigorous and consistent compliance with policies for hand hygiene, use of personal protective equipment and safe disposal of sharps. To be aware of and adhere to all policies and procedures, the Health and Safety at Work Act and the Data Protection Act. To maintain confidentiality at all times.
Other
These guidelines are provided to assist in the performance of the contract but are not a condition of the contract. The job description is not intended to be exhaustive and it is likely that duties may be altered from time to time in the light of changing circumstances and after consultation with the post- holder.
All staff will be regularly assessed on their knowledge, skills and behaviour, and application of all aspects of the job description, in line with the Individual Performance Review (IPR) process.
Staff will also be expected to work according to HPC guidelines and code of professional practice and relevant professional guidelines.
4