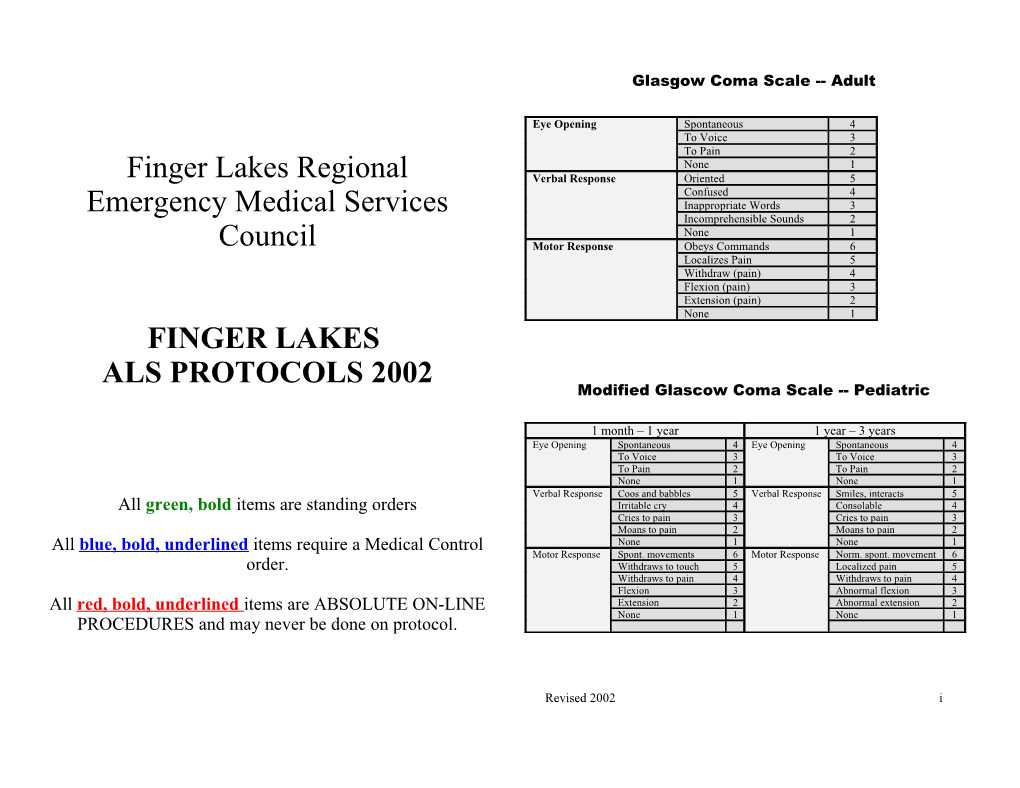
Glasgow Coma Scale -- Adult
Eye Opening Spontaneous 4 To Voice 3 To Pain 2 None 1 Finger Lakes Regional Verbal Response Oriented 5 Confused 4 Emergency Medical Services Inappropriate Words 3 Incomprehensible Sounds 2 None 1 Council Motor Response Obeys Commands 6 Localizes Pain 5 Withdraw (pain) 4 Flexion (pain) 3 Extension (pain) 2 None 1 FINGER LAKES ALS PROTOCOLS 2002 Modified Glascow Coma Scale -- Pediatric
1 month – 1 year 1 year – 3 years Eye Opening Spontaneous 4 Eye Opening Spontaneous 4 To Voice 3 To Voice 3 To Pain 2 To Pain 2 None 1 None 1 Verbal Response Coos and babbles 5 Verbal Response Smiles, interacts 5 All green, bold items are standing orders Irritable cry 4 Consolable 4 Cries to pain 3 Cries to pain 3 Moans to pain 2 Moans to pain 2 All blue, bold, underlined items require a Medical Control None 1 None 1 Motor Response Spont. movements 6 Motor Response Norm. spont. movement 6 order. Withdraws to touch 5 Localized pain 5 Withdraws to pain 4 Withdraws to pain 4 Flexion 3 Abnormal flexion 3 All red, bold, underlined items are ABSOLUTE ON-LINE Extension 2 Abnormal extension 2 None 1 None 1 PROCEDURES and may never be done on protocol.
Revised 2002 i Table of Contents Toxemia of Pregnancy ...... 38
Glasgow Coma Scale…………………………………………………….. i Preface ...... iv Revised 2002 ii Statement of Philosophy ...... iv Table of Contents Authorization / Verification ...... iv Acknowledgments ...... v PEDIATRIC PROTOCOLS Levels of Care ...... vi, vii Routine Pediatric Medical Care / General Principles ...... 41 ALS Dispatch Criteria………...... viii Pediatric Normal Weights / Vital Signs ...... 42 Pediatric Hypotension ...... 42 ADULT PROTOCOLS Pediatric Airway Management – Equipment Sizes ...... 43 Routine Medical Care – Standing Orders ...... ….2 APGAR Scoring System ...... 43 Routine Trauma Care ...... …. 3, 4 Pediatric Drug Dosage Table ...... 44 Airway Management ...... …. 5 Airway Management ...... 45 Oxygen Therapy ...... … 6 Oxygen Therapy ...... 45 Airway Obstruction ...... …. 7 Airway Obstruction (Foreign Body)...... 46 IV Therapy ...... 8 IV Therapy ...... 47 Fluid Challenge / Replacement ...... …8 Fluid Challenge / Replacement ...... 48 Altered Mental Status – Unknown Origin ...... 9 Routine Trauma Care ...... 49,50 Analgesia (Pain Control) ...... 10 Altered Mental Status – Unknown Origin ...... 51 Anaphylactic Shock / Allergic Reaction ...... 11 Analgesia (Pain Control) ...... 52 Behavioral Emergencies ...... 12 Anaphylactic Shock / Allergic Reaction ...... 53 Burns ...... 13 Burns ...... 54 Cardiac Arrest – General ...... 14 Cardiac Arrest – General ...... 55 Asystole ...... 15 Asystole ...... 56 VF / Pulseless VT (semi-automatic defibrillator)...... 16 VF ...... 57 VF / Pulseless VT (manual defibrillator) ...... 17 PEA ...... 58 PEA ...... 18 Cardiac – Bradycardia ...... 59 Cardiac – Bradycardia ...... 19 SVT ...... 60 Postconversion of VF / VT ...... 20 VT ...... 61 SVT ...... 21 Chest Trauma ...... 62 VT ...... 22 Diabetic Related Emergencies ...... 63 Chest Pain - Poss. Cardiac Origin ...... 23 Head Trauma ...... 64 Chest Trauma ...... 24 Hyperthermia – Heat Exhaustion / Heat Stroke ...... 65 CHF / Pulmonary Edema ...... 25 Hypotension / Shock ...... 66 Diabetic Related Emergencies ...... 26 Hypothermia ...... 67 Sedation Facilitated Intubation …………………………………………… 27 Near Drowning ...... 68 RSI…………………………..……………………………………………. 28 Neonatal Resuscitation ...... 69 Head Trauma ...... 29 Poisoning / Overdose ...... 70 Hyperthermia – Heat Exhaustion / Heat Stroke ...... 30 Respiratory Distress ...... 71 Hypotension / Shock ...... 31 Seizures ...... 72 Hypothermia ...... 32 SPECIAL PROTOCOLS Near Drowning ...... 33 Initiation/Termination of Resuscitation...... ………………...... 75, 76 OB / GYN Emergencies ...... …... 34 Helicopter Utilization Guidelines ...... 77 Poisoning / Overdose ...... 35 Mass Casualty Incident (MCI) ...... 78 Respiratory Distress Secondary to Asthma or COPD ...... …. 36 Medical Control ...... 79 Seizures ...... 37 On Scene Medical Personnel ...... 80 Patient Refusal Of Transport / AMA ...... 81 800 of the Codes and Regulations of the State of New York. The Finger Lakes Radio / Phone Failure ...... 82 REMAC approved these protocols on December 18, 2001. Transportation / Destination ...... 83 Universal Precautions ...... 84 Epinephrine Auto-injector ………………………………………………… 85 Nebulized Albuterol ……………………………………………………… 86 ______Surgical Airway …………………………………………..………………. 87 Frank Edwards, MD, FLREMSC Medical Director Date Dopamine Chart ………………………………………………………….. 88 Chairman, FLREMAC Formulary …………………………………………………..……………… 89 Preface Revised 2002 iv Acknowledgements These are the Finger Lakes A-EMT Protocols, as developed by the REMAC and approved by the Finger Lakes Regional EMS Council and its System Medical Director in 2002. Protocols for each patient care situation are listed in algorithmic We wish to thank all physicians and EMS providers who provided comments and format. These protocols assume that EMTs in the region stay well-versed in suggestions during 2001-2002 protocol revision process. emergency medical care to their level of certification, and maintain a good understanding of the emergency situations contained in this document. Both adult Protocol Subcommittee and pediatric protocols will be found herein. Frank Edwards, MD, Chair John Sullivan, MD Advanced technicians working in Finger Lakes Regional EMS area are expected to Everett Ferguson, EMT-P observe these protocols at all times. They may not be altered without approval from Jeff Harloff, EMT-P the Agency Medical Director. These protocols are designed to act as STANDING Bruce Lee, PA, EMT-P ORDERS within the guidelines stated on each page. Finger Lakes REMAC Frank Edwards, MD, Chair Statement of Philosophy Jack Davidoff, MD Sandra Eckhert, MD John Sullivan, MD No protocol can be written to cover all situations an advanced technician may Mark Winsberg, MD encounter while practicing in the field, nor are protocols a substitute for good Deborah Fratangelo, RN judgment seasoned by long experience. Technicians are expected to always utilize Karole Shafer, RN their best judgment, and to deliver care in the most prudent and reasonable fashion Michael Healy, EMT-D possible. Sande Johnson, EMT-D Everett Ferguson, EMT-P Any order given to the advanced technician by a medical control physician--or an Bruce Lee, PA, EMT-P on-scene physician--which directly contradicts or lies outside these protocols and/or Ken Kelly, EMT-P the advanced technician’s scope of training, shall be respectfully declined by the William Stubba, RN, EMT-P technician. Jeff Harloff, EMT-D, Ontario Co. EMS William Liddle, EMT-D, Wayne Co. EMS Authorization / Verification Patricia Paddock, EMT-I, Yates Co. EMS Jack Trutschel, EMT-CC, Seneca Co. EMS
The Medical Director for the Finger Lakes Regional EMS Council attests that these ALS Protocols constitute reasonable guidelines for off-line and on-line medical control of the Advanced Life Support System of the Finger Lakes Region in the State of New York, as required by Article 30, subsection 31 of the State of New York Public Health Law, as well as the requirements for medical direction specified in Part Revised 2002 v Levels of Care
Persons at the appropriate level of certification are allowed to perform the Revised 2002 vi following skills:
EMT-D Cardiac: Defibrillation with AED or semi-automatic defibrillator if approved by corps medical director. EMT-Ds are NOT authorized to utilize cardiac monitoring devices. Airway: Basic airway management only Evaluation: Blood glucose determination using a commercially available device with approval of the corps medical director and completion of appropriate training. Medication Administration: Assist patient in taking his / her prescribed medication. If the agency has received approval and the EMT-D has completed the required training, he/she may administer the epinephrine auto-injector and/or nebulized albuterol per protocol.
EMT-Intermediate All of the above skills plus: Cardiac: Defibrillate with AED; monitor and defibrillate with semi- automatic device or with manual defibrillator if approved by corps medical director. Airway: • Oral tracheal intubation using a laryngoscope (direct vision). • Use of the CombiTube airway IV Therapy: • Venous cannulation of peripheral veins • IV attempts limited to three; do not delay transport • IV sites limited to arms • IO • Blood draws
EMT-Critical Care All of the above skills plus: Cardiac: • Monitor rhythm with a manual monitor/defibrillator • Rhythm interpretation • Defibrillation with a manual defibrillator • Synchronized cardioversion • External cardiac pacing Airway: • Tracheal suctioning through ETT • Needle chest decompression, with approval of the agency medical director Levels of Care Cont. Revised 2002 vii
IV Therapy: • Peripheral venous cannulation • External jugular cannulation in cardiac arrest situations only • IV attempts limited to three in ten minutes; repeated attempts should not delay transport per protocol and medical control order Medication Administration: • Administer medication from the Regional medication schedule per protocol and medical control order.
EMT-Paramedic All of the above skills plus: Airway: • Needle chest decompression • Needle cricothyrotomy (only with jet insufflation) ALS Dispatch Criteria
EMS dispatch centers in the Finger Lakes region are encouraged to use the following criteria as warranting simultaneous automatic dispatch of the closest available ALS unit:
• Allergic reactions (anaphylactic shock) • Breathing problems (asthma and COPD) • Burns (2° and 3°) • Cardiac and/or respiratory arrest • Chest trauma • Chest pain • Childbirth • Choking • Diabetic with altered LOC • Drowning • Drug overdose • Electrocutions • Hazardous Material • Hemorrhaging (massive, acute, severe) • Falls from a height • Fires with people trapped • Gunshot wounds • MCI • MVA with people trapped • Motorcycle accidents with cyclist down • Pedestrian struck • Pediatrics (serious nature) • Physician request • Poisoning • Seizures • Unconscious / unresponsive person
ALS services should be automatically dispatched in the above situations.
Revised 2002 viii Routine Medical Care
STANDING ORDERS:
The following procedures will be performed on ALL patients:
ALL – Patient care equipment will always be brought to the patient. This includes: • Oxygen, suction, bag with BP cuff, oxygen masks, BVM, and oropharyngeal airways. • Advanced airway kit (I / CC / P only) • Monitor / defibrillator per technician’s level of care • Medication box and telemetry unit (CC / P only) Adult Protocols – Airway management, ventilatory assistance, and oxygen therapy as appropriate. – Serial vital signs and patient assessment.
CC / P – EKG monitoring for all patients requiring CC / P level care. – Contact medical control within 15 minutes of initial patient contact, if conditions will allow, for every patient > 16 Years of in need of advanced life support measures. If patient requires CC/P level of care, begin transport and attempt intercept en route. BLS units should NOT delay transport to await either CC/P or air ambulance; arrange a rendezvous as Age necessary. Routine Trauma Triage Protocol (Adult)
Revised 2002 -2- I Blunt or Penetrating Trauma With Unmanageable Airway • Except for special circumstances, on-scene time should not exceed ten minutes. • Condition present: • Medical command may be contacted any time during the assessment process – begin airway management measures • If there are any questions, concerns, or extenuating circumstances (weather, etc.) it – transport to nearest hospital is recommended that medical command be contacted • Condition absent– assess for: II Trauma Arrest • Condition present: Revised 2002 -3- – begin CPR – transport to nearest hospital • Condition absent– assess for: III. Multi-system Trauma With: – unstable V.S. – hemodynamic compromise (shock symptoms) – respiratory compromise (RR < 10 or > 28) – altered mental status or LOC > 5 minutes • Condition present: – begin routine trauma care – transport to trauma center – if > 15 minutes to trauma center, launch helicopter • Condition absent– assess for: IV. Anatomic Injury – penetrating injury head, neck, torso, groin – 2° / 3° burns > 15% BSA, or any burn involving face, airway, hands, feet, or genitalia – partial or complete paralysis of new onset – flail chest / major blunt chest injury – > 2 long bone fractures – suspected open or depressed skull fracture – suspected unstable pelvis or pelvic fracture – partial or full amputation proximal to digits • Condition present: – begin routine trauma care – transport to trauma center – if > 15 minutes to trauma center, launch helicopter • Condition absent– assess for: V. Increased Risk For Severe Injury – > 60 y/o w/ significant mechanism – ejection from vehicle – death of occupant in same vehicle – auto crash w/ significant intrusion into passenger compartment – significant fall from a height – bent steering column – significant auto-pedestrian impact – significant motorcycle, ATV, horse, or bicycle incident – major chronic illness (respiratory, cardiac, etc.) – high risk medical condition (on anticoagulants like coumadin, etc.) – pregnancy > 20 week gestation • Condition present: – begin routine trauma care – if pt < 18 y/o, transport to trauma center – if pt > 18 y/o, contact medical command to consider trauma center – if medical command not available, transport to trauma center – if decision made for trauma center and if > 15 minutes to trauma center, launch Routine Trauma Care (Adult) Cont.
STANDING ORDERS :
• Determine Trauma Triage Criteria (see previous page)
______|______| |
Criteria Present Criteria Absent
• Spinal immobilization & transport • Perform secondary survey • IV NS • Stabilize patient prn If BP < 90 with signs of shock • IV NS prn • Consider second IV line • Transport to nearest facility • EKG monitoring • Contact medical control • Contact medical control
Note: the use of blood administration set is recommended in place of standard IV sets.
AS NEEDED, see also protocols for:
Airway Management (5) IV Therapy (p. 8) Cardiac Arrest (pp. 14-18) Chest Trauma (p. 24)
Revised 2002 -4- Airway Management
STANDING ORDERS : Revised 2002 -5- ALL • Establish patent airway – Manually open airway prn – Head tilt / chin lift (non-trauma) – Modified jaw thrust (trauma) • Suction prn • Oropharyngeal / nasopharyngeal airway prn • Ventilation with BVM and 100 % oxygen prn
I / CC / P • May attempt orotracheal intubation up to three times per patient on patients requiring definitive airway management. – with manual stabilization for trauma
• In a tiered response situation, a CC / P technician arriving after ILS technicians have already attempted intubation may also attempt intubation up to three times per patient.
• Following intubation, ventilate patient with 100 % oxygen.
• Perform primary airway placement check: auscultate for bilateral breath sounds and absence of epigastric sounds, look for chest rise and condensation of tube with exhalation.
• Perform secondary airway placement assessment: for cases other than full arrest, use ETCO2 Detector and/or Esophageal Detector Device. For full arrest patients, use Esophageal Detector Device.
• CombiTube device may be utilized in case of failed intubation.
ABSOLUTE ON-LINE MEDICAL CONTROL:
P • When all else has failed, perform needle cricothyroidotomy with jet insufflation. Oxygen Therapy
STANDING ORDERS:
ALL • Administer oxygen via a non-rebreathing mask. The flow rate Revised 2002 -6- should be sufficient to keep the bag on the mask inflated (10-15 lpm).
• If patient does not tolerate the mask, use nasal cannula at 6 lpm.
• Assist respirations as needed. Patients with COPD may require coaching or ventilation assistance. DO NOT WITHHOLD HIGH CONCENTRATIONS OF OXYGEN FROM ANY DYSPENIC PATIENT, REGARDLESS OF COPD HISTORY.
CC / P • Administer oxygen to patients to maintain an O2 Sat > 95% if the following are absent: – LOC – Signs of respiratory distress or cyanosis – Signs of shock or inadequate tissue perfusion – Mechanism suggests the possibility of toxic substance inhalation (i.e. carbon monoxide, cyanide, etc.) – Hypothermia
• If any of the above criteria are present, administer oxygen at high concentrations and assist ventilations as necessary. Airway Obstruction IV Therapy (I / CC / P)
STANDING ORDERS: STANDING ORDERS :
CONSCIOUS PATIENT: Assess air exchange and oxygenation status of patient. ILS – ILS technicians will only start IVs on patients if one or more of ALL the following conditions is present: ______|______| | – The ILS agency is a non-transporting rescue agency awaiting the arrival of a transporting unit which has not arrived. Adequate air exchange – Inadequate air exchange – – The ILS agency is transporting the patient and the IV can be able to cough / speak / breathe cannot cough / speak / breathe started en route. – By order of medical control or on scene CC/P. • Encourage coughing • Administer 5 abdominal / chest – At the scene when a prolonged patient extrication is involved. • Rapid transport thrusts • Oxygen as tolerated • Repeat as necessary • Start IV of NS or saline lock on all patients requiring ALS-level care unless otherwise specified.
UNCONSCIOUS PATIENT: • Run at KVO rate (10 ml/hr), unless directed differently by protocol or medical control. ALL • Manually open airway, attempt to ventilate with 2 breaths CC / P • May start external jugular in patients in cardiopulmonary arrest. • Reposition and reattempt to ventilate • Administer 5 abdominal / chest thrusts ONLY INTERMEDIATE, CRITICAL CARE AND PARAMEDIC LEVEL • Suction and finger sweep prn TECHNICIANS WITHIN THE FLREMS REGION MAY MONITOR IVs • Repeat this sequence as needed DURING TRANSPORT. BLS units, however, may transport patients with saline or heparin locks in place. I / CC / P • Attempt direct laryngoscopy and removal of foreign object with Magill forceps
ON-LINE MEDICAL CONTROL ( standin g order if communication failure): Fluid Challenge / Replacement (I / CC / P)
P • Needle cricothyrotomy, if still obstructed STANDING ORDERS: • Fluid Challenge appropriate only if signs and symptoms of CHF are absent, and systolic BP is less than 90 mmHg. IF INITIAL EFFORTS TO DISLODGE OBJECT ARE UNSUCCESSFUL, • Start IV of NS using large bore needle and standard administration set, or BEGIN RAPID TRANSPORT AND CONTINUE EFFORTS EN ROUTE. blood administration set. • Infuse 250 ml rapidly and reassess vital signs. • May infuse repeat 250 ml NS boluses, up to 1000 ml total, if systolic BP remains <90 mmHg and no signs or symptoms of CHF develop.
Trauma situations: • Penetrating trauma – IV TKO and contact Medical Control. Revised 2002 -7- • Blunt trauma – IV 250ml boluses to maintain a SBP of 90-100 mmHg. Revised 2002 -8- Altered Mental Status – Unknown Origin
STANDING ORDERS:
ALL • Routine medical care (p. 2) • Be prepared to assist respirations with BVM if respiratory rate decreases to < 12, or becomes ineffective. Ineffective respirations means minimal air movement, decreasing level of consciousness, falling respiratory rate, or persisting cyanosis. • Assess blood glucose. (EMT-D’s can perform fingerstick glucose testing only if the corps has prior off-line approval by its medical director. Glucose may be administered without checking BG if EMT is not cleared for fingerstick testing.)
______|______| |
Glucose < 60 Glucose > 60
CC / P CC / P • If history of possible alcoholism, • Naloxone (Narcan) 2 mg IV, IM, administer Thiamine 100mg IV or ET or IM • 50 ml D50 IV push • Naloxone (Narcan) 2 mg IV, IM, or ET • Reassess blood glucose and repeat D50 prn • If unable to place IV, glucagon 1 mg IM Revised 2002 -9- Analgesia (Pain Control)
STANDING ORDERS:
ALL • Routine medical care (p. 2) • Identify and treat cause of the underlying cause of pain, if possible.
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P • Nalbuphine (Nubain) 5-10 mg IV or IM
OR
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • Morphine sulfate 1-10 mg IVP or IM; may repeat as ordered by Medical Control q5 min to desired analgesic response.
• If hypotension, respiratory depression or stupor develops secondary to the analgesic, administer Naloxone ( Narcan) 0.4-2 mg IVP, IM or ET
Revised 2002 -10- Anaphylactic Shock / Allergic Reaction
STANDING ORDERS:
ALL • Routine medical care (p. 2) • If patient has own epinephrine auto-injector, all EMTs may assist the patient in administering the epinephrine injection. • If the agency has been approved to carry an epinephrine auto- injector, see epinephrine auto-injector protocol (p. 85). • Rapid transport.
I / CC / P • IV NS. If systolic BP < 90, Fluid Challenge protocol (p. 8).
CC / P • Epinephrine 1:1,000 0.3 ml IM or SQ. • Diphenhydramine 25-50 mg IM or IV. • Nebulized albuterol 2.5 mg, if wheezing present.
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P • Repeat epinephrine 1:1,000 0.3 ml IM or SQ q5 min prn, if hypotension persists.
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • If patient remains hypotensive, contact Medical Control for possible use of epinephrine 1:10,000 IV at dosage to be determined by Medical Control.
Revised 2002 -11- Behavioral Emergencies
STANDING ORDERS :
ALL • ASSURE SCENE SAFETY. • Routine medical care (p. 2) • Consider law enforcement • Perform secondary assessment. • Look for medical or traumatic causes for the patient’s behavior • Refer to Altered Mental Status protocol (p. 9)
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P • Physically or chemically restrain if suicidal/homicidal, or if patient represents a danger to himself or to the crew.
Chemical Restraint: 1) Haloperidol (Haldol) • Adult: 2.5-5.0 mg IV/IM/PO. May repeat q10 min. prn, to a maximum dose of 10 mg.
• Patients ≥ 70 years or with chronic illness, haloperidol 1 to 2.5 mg IV/IM/PO, max dose 2.5 mg.
• For dystonic reactions to haloperidol, administer diphenhydramine 25-50 mg IM or IV.
OR
2) Diazepam (Valium) • Adult: 2-5 mg IV over 2-5 minute, max dose 5mg.
O OR 3) Lorazepam (Ativan) • Adult: 0.5 – 2.0 mg IM/IV over 2-5 minutes, max dose 2mg.
For all of the above: If inadequate or no effect response, contact Medical Control.
Revised 2002 -12- Burns – Thermal Revised 2002 -13-
STANDING ORDERS: ALL • ASSURE SCENE SAFETY • Remove constricting clothing and jewelry. • High concentration O2 (10-15 lpm) if airway burn / inhalation injury suspected. • Do not rupture blisters or apply any ointment or medication to burns. • Cover burns with sterile gauze soaked in saline*. Avoid ice or cold compresses. • Maintain body temperature (keep patient covered) • Consider transport to a Burn Unit (see Trauma protocol p. 3)
I / CC / P • If 2° burns cover > 15 % BSA, start IV of NS at 1000 ml over 30 minutes, then 500 ml/hr.
CC / P • Analgesia protocol (p. 10)
* If burns > 15% BSA, cool for no longer than 1 minute, then dress with dry sterile dressings.
Burns – Electrical
STANDING ORDERS : ALL • Determine current source. Remove patient after current shut off. USE CAUTION! • Cover entrance and exit burns with dry sterile dressing.
I / CC / P • Start IV NS at KVO rate.
CC / P • Monitor EKG ASAP and treat arrhythmias as appropriate. • Analgesia protocol (p. 10)
Burns – Chemical
STANDING ORDERS : ALL • Remove clothing, jewelry, etc. and flush skin with large quantities of water. • Flush eyes with NS, if appropriate.
CC / P • Analgesia protocol (p. 10) Cardiac Arrest – General
The following applies in all cardiac arrest situations.
STANDING ORDERS:
ALL • Survey scene for indications of DNR status. • Routine medical care, CPR and airway management up to level of training. • CPR to be continued at all times except during defibrillation and/or interruptions < 30 sec for patient transfer. • If ALS not on scene, initiate rapid transport to nearest hospital or plan for ALS intercept. • Advise receiving hospital ASAP.
EMT-D • Connect and operate AED/semi-automatic device. Observe EMT-D VF / pulseless VT protocol (p. 16), if shock indicated by machine and patient is pulseless.
EMT-I • Intubation should be performed ASAP following any initial defibrillation attempts. • IV NS KVO as time allows. DO NOT delay initiation of transport.
CC / P • Intubation should be performed ASAP following any initial defibrillation attempts. • IV NS KVO. • Attach monitor or “quick look” paddles and refer to appropriate cardiac arrest dysrhythmia protocol.
NOTE: Biphasic technology has been approved by the Finger Lakes REMAC for manual and AED defibrillation. Follow each manufacturer's energy settings for cardioversion and defibrillation as their energy settings for cardioversion and defibrillation differ.
Revised 2002 -14- Cardiac Arrest - Asystole Cardiac Arrest – VF / Pulseless VT – AED/Semi-Automatic Defibrillator
Also see Cardiac Arrest – General protocol (p. 14) Also see Cardiac Arrest – General protocol (p. 14) STANDING ORDERS: STANDING ORDERS : EMT-D / I • If witnessed arrest, precordial thump (optional) CC / P • Survey scene for indications of DNR status. • CPR until automatic defibrillator is attached • If NO DNR present and family of patient wishes DNR, • Press ANALYZE; defibrillate 200 joules contact Medical Control. • Press ANALYZE; defibrillate 200-300 joules • Initiate CPR, if indicated • Press ANALYZE; defibrillate up to 360 joules • Confirm asystole in 2 leads • If pulseless, CPR for one minute • If possibility of fine VF exists, treat patient as for VF • Press ANALYZE; defibrillate up to 360 joules • Intubate as soon as possible; establish IV access • Press ANALYZE; defibrillate up to 360 joules • Consider transcutaneous external pacemaker, if available • Press ANALYZE; defibrillate up to 360 joules • Epinephrine 1:10,000 1 mg IV or 2 mg ET. Repeat q3-5 min • If pulseless, CPR for one minute during arrest • Atropine 1 mg IV or 2 mg ET. Alternate epinephrine doses ______|______with atropine up to a maximum of 0.04 mg/kg | | • Review quality of resuscitation. • Consider possible causes (hypovolemia; hypoxia; cardiac Short transport Long Transport Time / tamponade; hypothermia; hypoglycemia; drug OD such as tricyclics, time ALS Back-up Nearby digitalis, ß-blockers, calcium channel blockers; massive acute myocardial infarction; tension pneumothorax; hyperkalemia; acidosis) and refer to relevant protocols. • Continue CPR • Repeat set of 3 stacked shocks with • Transport up to 360 joules If asystole continues 25 min., consider termination of resuscitation in • If pulseless, CPR for one minute the field (termination of resuscitation protocol, p.75-76 ) • Transport
ABSOLUTE ON-LINE MEDICAL CONTROL: • Defibrillation can be monophasic (listed above) or biphasic -- follow each CC/P • Consider Sodium Bicarbonate 1 mEq/kg IV in the following manufacturer's energy settings for cardioversion and defibrillation. situations: • Known pre-existing non-respiratory acidosis • If "no shock indicated" appears, check pulse, repeat one minute of CPR and then • Known pre-existing hyperkalemia reanalyze. After 3 "no shock indicated" messages are received, repeat analyze • Drug overdose (especially tricyclic antidepressant) period every 1-2 minutes. • Long arrest interval (> 10-15 min) and patient is intubated • Pulse checks are not required after shocks 1, 2, 3, and 5 unless the "no shock indicated" message appears. • If VF recurs after transiently converting (rather than persisting without ever converting), restart the treatment algorithm from the top. • In the event that VF persists after 9 shocks, repeat sets of 3 stacked shocks with one minute of CPR between each set.
Revised 2002 -15- Revised 2002 -16- Cardiac Arrest – VF / Pulseless VT – Manual Defribillator
STANDING ORDERS:
CC / P • If witnessed arrest, may attempt precordial thump • Defibrillate up to 3 times prn (200 j, 200-300 j, 360 j) • Intubate at once; obtain IV access when able without delaying treatment • Epinephrine 1:10,000 1 mg IV or 2 mg ET. Repeat q3-5 min during arrest OR Alternative: Vasopressin 40 Units IV ONE TIME DOSE • Defibrillate 360 j • Lidocaine 1.5 mg/kg IV or 3 mg/kg ET OR Alternative: Amiodarone 300mg IV Push; consider repeating 150mg IV Push q3-5 minutes, prn--max dose 2.2 gm. • Defibrillate 360 j • Repeat Lidocaine 0.75 mg/kg IV or 1.5 mg/kg ET • Defibrillate 360 j • Consider Procainamide 20 mg/min infusion, or may give as 100mg IV boluses q5 minutes up to 17 mg/kg. • Defibrillate 360 j TRANSPORT
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P • Consider Magnesium sulfate 2g IV in the following situations: • Torsade de pointes • Suspected hypomagnesia • Severe refractory VF • Defibrillate 360 j
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • Consider Sodium Bicarbonate 1 mEq/kg IV in the following situations: Known pre-existing non-respiratory acidosis (eg. diabetic ketoacidosis); known pre-existing hyperkalemia; drug overdose (especially tricyclic antidepressant).
NOTE: Following conversion, refer to other appropriate dysrhythmia protocols and/or Postconversion protocol (p. 20) prn.
• Defibrillation can be monophasic (listed above) or biphasic -- follow each manufacturer's energy settings for cardioversion and defibrillation.
Revised 2002 -17- Cardiac Arrest -- PEA Cardiac – Bradycardia
STANDING ORDERS : Also see Cardiac Arrest – General Protocol (p. 14) ALL • Routine medical care (p. 2) STANDING ORDERS: CC / P • Assess hemodynamic status – asymptomatic bradycardias CC / P • Intubate at once; obtain IV access when able without delaying require no treatment. Treatments listed below are to be used treatment only if one or more of these conditions exist: • Epinephrine 1:10,000 1 mg IV or 2 mg ET. Repeat q3-5 min • Altered mental status during arrest • Severe chest pain • If bradycardic rhythm present, atropine 1 mg IV or 2 mg ET • Lightheadedness, dizziness, nausea Repeat q3-5 min up to a maximum dose of 2 mg IV or 4 mg • Systolic BP < 90 ET • PVCs • Transport • Atropine 0.5-1 mg IV or 2 mg ET; repeat q3-5 min up to • Consider possible causes: (hypovolemia; hypoxia; cardiac maximum dose of 2 mg IV or 4 mg ET unless tamponade; hypothermia; massive pulmonary embolism; drug OD such contraindications: as tricyclics, digitalis, ß-blockers, calcium channel blockers; massive • Atropine contraindicated in 3 o heart block; go directly to acute myocardial infarction; tension pneumothorax; hyperkalemia; use of pacemaker or contact Medical Control. acidosis) and refer to relevant protocol. • Transcutaneous external pacemaker, if available.
ABSOLUTE ON-LINE MEDICAL CONTROL: ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • Consider Sodium bicarbonate 1 mEq/kg IV in the following CC / P • Dopamine drip @ 5-20 µg/kg/min IV. . situations: Known pre-existing non-respiratory acidosis (eg. diabetic • Epinephrine drip @ 2-10 µg/min IV ketoacidosis); known pre-existing hyperkalemia; drug overdose • Only ONE of these agents should run at a time. (especially tricyclic antidepressant). Discontinue other drips as new agents are used.
ANALGESIC / SEDATION for cardioversion / transcutaneous pacing:
• Note: Do not delay immediately necessary treatment for sedation or analgesia
• Diazepam 2-5 mg IV
• OR, lorazepam 0.5-2 mg IV • If hypotension, respiratory depression or stupor develops, administer Flumazenil 0.2 mg IVP over 30 seconds. If no response, contact Medical Control.
• OR, may consider using morphine sulfate 2-4 mg IVP. • If hypotension, respiratory depression or stupor develops, administer Naloxone (Narcan) 0.4-2 mg IVP, IM or ET.
Revised 2002 -18- Revised 2002 -19- Cardiac – Postconversion of VF / VT
STANDING ORDERS:
ALL • Assure presence of pulse. Routine medical care (p. 2)
CC / P • Assess rhythm. Treatment listed to be used only in presence of supraventricular rhythm with pulse at adequate rate. Refer to other dysrhythmia protocols (bradycardia, PEA, etc.) prn. • What was the last antiarrhythmic drug administered during the arrest? ______|______| | None Lidocaine
• Lidocaine bolus 1 mg/kg IV / ET • Begin lidocaine drip at 2-4 • Begin lidocaine drip at 2 mg/min mg/min IV IV ABSOLUTE ON-LINE: ABSOLUTE ON-LINE: • Repeat lidocaine boluses prn (up • Repeat lidocaine boluses prn (up to 3 mg/kg) and increase drip to 3 mg/kg) and increase drip rate prn (up to 4 mg/min) per rate prn (up to 4 mg/min) per medical control medical control
Revised 2002 -20- Cardiac – SVT (Narrow Complex) Cardiac – VT (Wide Complex) If there is no pulse, refer to the Cardiac Arrest/ VF protocol (pp. 16, 17) STANDING ORDERS : STANDING ORDERS: ALL • Routine medical care (p. 2) ALL • Routine medical care (p. 2) CC / P • Assess hemodynamic status / stability of patient • If QRS complex is wide, treat as VT CC / P • Assess hemodynamic status / stability of patient ______|______|______| | | | Unstable Stable Unstable Stable HR > 150 bpm • Sync cardioversion 100 j • Lidocaine 0.5-0.75 mg/kg IV • Sync cardioversion 50-100 j • Valsalva maneuver • Sync cardioversion 200 j • Sync cardioversion 200 j • Consider Adenosine 6 mg IV • Sync cardioversion 300 j ON-LINE MEDICAL • Sync cardioversion 300 j • Sync cardioversion 360 j CONTROL: • Sync cardioversion 360 j ON-LINE MEDICAL CONTROL: • Transport / drug therapy en route • Transport / drug therapy en route per medical control • Consider Amiodarone 150 mg IV per medical control • Adenosine 12 mg IV over 10 min. ON-LINE MEDICAL CONTROL: • May consider trial of adenosine ON-LINE MEDICAL CONTROL: ABSOLUTE ON-LINE: 6mg IVP. • Pharmacological therapy, repeat • Pharmacological therapy, repeat • Diltiazem 0.25 mg/kg (average 20 cardioversion at 360 j ABSOLUTE ON-LINE: cardioversion at 360 j mg) IV • May repeat diltiazem in 15 min at HR < 150 bpm • Cardiovert as in unstable pts 0.35 mg (average 25 mg) IV • Call Medical Control • Verapamil 2-5 mg IV • Cardiovert as in unstable Following cardioversion, refer to other appropriate dysrhythmia protocols and/or patients Postconversion protocol (p. 20) prn.
ABSOLUTE ON-LINE MEDICAL CONTROL: ABSOLUTE ON-LINE MEDICAL CONTROL: ANALGESIC / SEDATION for cardioversion / transcutaneous pacing: ANALGESIC / SEDATION for cardioversion / transcutaneous pacing: • Note: Do not delay immediately necessary treatment for • Note: Do not delay immediately necessary treatment for sedation or analgesia sedation or analgesia • Diazepam 2-5 mg IV • Diazepam 2-5 mg IV • OR Lorazepam 0.5-2 mg IVP. • OR Lorazepam 0.5-2 mg IVP. • If hypotension, respiratory depression or stupor develops, • If hypotension, respiratory depression or stupor develops, administer Flumazenil 0.2 mg IVP over 30 seconds. If no administer Flumazenil 0.2 mg IVP over 30 seconds. If no response, contact Medical Control. response, contact Medical Control. • OR Morphine sulfate 2-4 mg IVP. • OR Morphine sulfate 2-4 mg IVP. • If hypotension, respiratory depression or stupor develops, • If hypotension, respiratory depression or stupor develops, administer Naloxone (Narcan) 0.4-2 mg IVP, IM or ET. administer Naloxone (Narcan) 0.4-2 mg IVP, IM or ET. Revised 2002 -21- Revised 2002 -22- Chest Pain – Poss. Cardiac Origin Chest Trauma
STANDING ORDERS: Includes pneumothorax, tension pneumothorax, penetrating chest injuries, rib fractures, and flail chest. ALL • Routine medical care (p. 2) • If systolic BP > 120, may assist patient with taking own STANDING ORDERS: nitroglycerin tablets if patient has them. (One tablet should be given sublingually q5 minutes up to a total of 3 tablets, unless ALL • Routine trauma care (p. 3) BP drops below 100 systolic.) • Stabilize and do not remove penetrating objects • Rapid transport to emergency department. • Use occlusive dressing to seal open wounds • Stabilize flail segments with bulky dressings CC / P • If systolic BP > 100, NTG 0.4 mg SL q5 min up to 3 tablets • Rapid transport total. • Aspirin 325 mg p.o (preferably by chewing baby tablets). ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P • If signs / symptoms of tension pneumothorax present, perform ON-LINE MEDICAL CONTROL ( standin g order if communication failure): needle thoracostomy
CC / P • Additional NTG 0.4 mg SL q5 min, as long as systolic BP > 100.
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • Morphine sulfate 1-5 mg IVP q5 min to desired analgesic response. • OR Nalbuphine (Nubain) 5-10 mg IV • If hypotension, respiratory depression or stupor develops, administer Naloxone 0.4-2 mg IVP, IM or ET
• If nausea / vomiting develop—promethazine (Phenergan) 12.5 mg IV, or 25 mg IM.
Revised 2002 -23- Revised 2002 -24- CHF / Pulmonary Edema
STANDING ORDERS:
ALL • Routine medical care (p. 2) • Rapid transport • Be prepared to assist respirations with BVM if respiratory rate decreases to < 12, or becomes ineffective. Ineffective respirations means minimal air movement, decreasing level of consciousness, falling respiratory rate, or persisting cyanosis
I / CC / P • If severe respiratory distress/respiratory arrest, intubate per protocol
CC / P • Assess systolic BP
______|______| |
Systolic BP > 100 Systolic BP < 100
• NTG 0.4 mg SL, repeated q5 min ABSOLUTE ON-LINE: as long as systolic BP > 100 • Furosemide (Lasix) 40-80 mg IV • Dopamine 5-10 µg/kg/min IV drip. ON-LINE MEDICAL CONTROL:
• Albuterol 2.5 mg nebulized, if wheezing present
ABSOLUTE ON-LINE:
• Nalbuphine (Nubain) 5-10 mg IV. (Refer to page 9) OR • Morphine sulfate 1-5 mg IVP q5 min to desired response. • If hypotension, respiratory depression or stupor develops, administer Naloxone (Narcan) 0.4-2 mg IVP, IM or ET
Revised 2002 -25- Diabetic Related Emergencies
STANDING ORDERS :
ALL • Routine medical care (p. 2) • Assess signs, symptoms and medical history • If patient appears hypoglycemic, administer glucose gel under tongue while protecting airway. If patient is conscious they may eat any form of available sugar, such as non-diet soda, candy, orange juice, or granular sugar • Whenever possible—especially before giving glucose--assess blood glucose by approved bedside fingerstick method. (EMT- D’s can perform fingerstick glucose testing only if the corps has prior off-line approval by its medical director. Glucose may be administered without checking BG if EMT is not cleared for fingerstick testing.)
Glucose < 60 Glucose > 300
CC / P I / CC / P • D50 50 ml IV push • IV NS at 500 ml/hr, if signs of • Reassess blood glucose CHF not present • Repeat D50 prn • If not able to place IV line, administer glucagon 1 mg IM
If level of consciousness does not improve in the hypoglycemic patient following administration of D50 , proceed with Altered Mental Status protocol (p. 9).
Revised 2002 -26- Sedation-Facilitated Intubation by EMT-CC/P
ABSOLUTE ON-LINE MEDICAL CONTROL:
For conscious adult patients in severe respiratory distress (potential respiratory failure) due to: CHF, life-threatening asthma, COPD, trauma, and all other causes:
CC/P • Administer high-flow oxygen via nonrebreather mask or give ventilation assistance with bag valve mask . • Prepare patient, calm and reassure, inform of procedure. • Establish IV NS • Sedate • Lorazepam 0.5 mg IV, OR diazepam 2-5 mg IV. • Lidocaine spray 2 seconds OR lidocaine gel on ETT • Perform cricoid pressure / Sellick’s maneuver and intubate patient. • Verify tube placement with ETCO2 device and/or esophageal detector device. • If unable to place ETT after three (3) attempts, consider CombiTube. • Maintain sedation throughout transport using: • Lorazepam 0.5-2.0 mg IV q15 min • OR Diazepam 2-5 mg IV q15 min. • Continue airway management and transport as per protocol • Include documentation of utilization of sedation-facilitated intubation protocol and follow REMAC-approved QA/CQI procedures
Revised 2002 -27- Rapid Sequence Intubation – by EMT-P Only
Any ALS (P) corps considering the use of RSI must submit a special request for approval by REMAC. Such a request must include a detailed protocol, a corps-specific training plan, evidence of approval and involvement by the Corps Medical Director , and a detailed description of a Corps- specific RSI QA/CQI program.
ABSOLUTE ON-LINE MEDICAL CONTROL:
For awake patients in severe respiratory distress due to: CHF , life-threatening asthma, COPD, trauma, and all other causes:
P • Hyperventilate with manual airway management • Establish IV NS • Administer lidocaine 2% 1-1.5 mg/kg IV to maximum dose 100 mg, if head injury • Administer etomidate 0.3 mg/kg IV Push. (Adults only) • Perform cricoid pressure / Sellick’s maneuver • Administer succinylcholine 1-1.5 mg/kg IV • Attempt ET intubation after paralysis occurs (usually < 1 min. and lasts 8-10 minutes) • Verify ETT placement with ETCO2 device and/or esophageal detector device. • If unable to place ETT after three (3) attempts, place CombiTube • Maintain sedation throughout transport using: • Lorazepam 0.5-2.0 mg IV q15 min. • OR Diazepam 2-5 mg IV q15 min. • Include documentation of utilization of RSI and REMAC- approved QA/CQI procedures
Revised 2002 -28- Head Trauma
STANDING ORDERS :
ALL • Administer high concentration O2 and assure airway patency • If respirations slow / shallow / irregular, assist with 100% O2 • If spontaneous respirations absent: • Begin immediate ventilation with 100% O2 • Hyperventilate patient* • Airway management up to level of training (intubation preferred--with appropriate spinal precautions). • Refer to Cardiac Arrest protocols if patient becomes hemodynamically unstable (pp. 14-18) prn • All patients to receive spinal immobilization as appropriate • Monitor vital signs and level of consciousness • Refer to Seizures protocol (p. 37) prn • Consider possibility of other trauma. Refer to Trauma protocols (p. 3-4) prn
CAUTION: If head injury is suspected, the GCS score is less than 8, and active seizures, or one or more of the following signs of brain herniation are present, hyperventilate the patient with high concentration oxygen at a rate of 20 breaths per minute: fixed or asymmetric pupils, abnormal flexion or abnormal extension (neurologic posturing), hypertension and bradycardia (Cushing’s reflex), intermittent apnea (periodic breathing), further decrease in GCS score of 2 or more points (neurologic deterioration).
*DO NOT HYPERVENTILATE UNLESS THE ABOVE CRITERIA ARE MET.
I / CC / P • If hypotensive, Hypotension protocol (p. 31), establish IV NS and provide fluid bolus as per Fluid Challenge protocol (p. 8). • Contact medical control
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • If nausea / vomiting present, promethazine (Phenergan) 12.5 mg IV, 25 mg IM. • If patient requires intubation, medics may refer to sedation- facilitated intubation protocol (p. 27).
Revised 2002 -29- Hyperthermia – Heat Exhaustion / Heat Stroke
STANDING ORDERS:
ALL • Routine medical care (p. 2) • Cool patient using whatever means immediately available • ice packs at groin, axillary sites • air conditioned ambulance • flushing with cool water
NOTE: Rapid cooling may cause vomiting
CAUTION: Wet sheets without good air circulation will retain heat rather than dissipate it.
I / CC / P • IV NS at 1000 ml/hr, if no signs of CHF
Also proceed with Altered Mental Status protocol (p. 9), if there is a decreased level of consciousness.
Revised 2002 -30- Hypotension / Shock Hypothermia
Defined as systolic BP < 90; one or more of the following signs are usually present: • Tachycardia STANDING ORDERS: • Delayed capillary refill > 3 seconds • Pallor, diaphoresis, cyanosis ALL • Routine medical care (p. 2) • Nausea, dizziness / lightheadedness, vomiting • Remove wet clothing, protect patient from environment • Altered mental status, confusion • Avoid rough handling • Rewarming of severely hypothermic patient best carried out in STANDING ORDERS: hospital • Rapid transport ALL • Routine medical (p. 2), or trauma (p. 3), care as appropriate • Consider other treatable causes – anaphylaxis, hypoglycemia, I / CC / P • IV NS at KVO dysrhythmia, trauma, bleeding, hypovolemia • Check blood glucose – refer to Diabetic Emergencies protocol p. 26) I / CC / P • Fluid challenge protocol (p. 8), if signs / symptoms of CHF absent. In the event of hypothermic cardiac arrest, MEDICAL CONTROL SHOULD BE CC / P • Treat dysrhythmias prn CONTACTED PRIOR TO ANY MEDICATION ADMINISTRATION. If there is any question as to the need for CPR, begin CPR and contact medical control for ABSOLUTE ON-LINE MEDICAL CONTROL: further advice.
CC / P • If no improvement and hypovolemia absent, dopamine 5-20 Proceed with Altered Mental Status protocol (p. 9) if there is a decreased level of µg/kg/min IV drip.. consciousness.
Revised 2002 -31- Revised 2002 -32- Near Drowning
STANDING ORDERS:
ALL • Routine medical (p. 2) or trauma (p. 3) care as appropriate.
• Institute standing BLS resuscitation measures and contact Medical Control.
• Institute spinal precautions if there is any chance of trauma.
• Refer to cardiac arrest protocols (pp. 14-18).
Revised 2002 -33- OB / GYN Emergencies
STANDING ORDERS:
ALL • Obtain history – prenatal care, due date, bleeding, edema of face / extremities, prior problems with pregnancy, other pertinent medical history and number of pregnancies. • Routine medical care (p. 2) Refer to Hypotension / Shock protocol (p. 31) prn. • Immediate rapid transport if: previous Cesarean section, multiple births, abnormal presentations, excessive bleeding. • Position patient on left side or, if not possible, with right buttock / hip slightly elevated.
I / CC / P • IV of NS at KVO
If delivering: • Allow baby to deliver spontaneously. Support infant, but do not attempt to retard or hasten delivery • Assess infant and proceed with Neonatal Resuscitation protocols (p. 69) prn • Clamp cord in two places 8-10" from infant; cut cord. • Wrap baby in clean / sterile blanket. Protect from hypothermia • Uterine massage and Hypotension / Shock protocol (p. 31) prn • Do not wait for or attempt delivery of placenta; if it delivers spontaneously, bring to hospital in plastic bag • Apply high flow O2
Breech presentation: • Transport prior to delivery if possible. If already in progress, allow to deliver spontaneously • If head delivers spontaneously, proceed with normal delivery procedures • If head does not deliver in 4-6 minutes, insert sterile gloved hand into vagina and create airway for baby. Rapid transport to hospital. Do not remove hand until relieved by hospital staff • Apply high flow O2
Prolapsed cord: • Insert gloved hand into vagina and gently push baby's head off cord. Initiate rapid transport and do not remove hand until relieved by hospital staff • Position patient in knee-chest position or Trendelenburg • Apply high flow O2 Revised 2002 -34- Poisoning / Overdose
STANDING ORDERS:
ALL • Routine medical care (p. 2) • CONTACT MEDICAL CONTROL • Save all emesis for analysis by hospital and bring poison container and all medications from scene to hospital
CC / P • Consider Naloxone (Narcan) for altered mental status – see Altered Mental Status protocol (p. 9)
ABSOLUTE ON-LINE MEDICAL CONTROL:
ALL • Medical control may order: • Sorbitol-free activated charcoal 50 - 100 g PO AND/OR • If not contraindicated, ipecac syrup 30 ml PO followed by 2 large glasses of water or other clear liquid
Revised 2002 -35- Respiratory Distress Secondary to Asthma or COPD
STANDING ORDERS:
ALL • Routine medical care (p. 2) • Assess history • Assess signs / symptoms, hemodynamic status • Rapid transport • Be prepared to assist respirations with BVM if respiratory rate decreases to < 12, or becomes ineffective. Ineffective respirations means minimal air movement, decreasing level of consciousness, falling respiratory rate, or persisting cyanosis • If patient is between one and sixty-five years of age and is experiencing an exacerbation of his/her previously diagnosed asthma, see nebulized albuterol protocol. (p. 86)
CC / P • Albuterol 2.5 mg nebulized (Alternate treatment: albuterol 2.5 mg and ipratropium (Atrovent) 0.5 mg mixed). May give under pressure using BVM, if necessary • Repeat albuterol 2.5 mg nebulized, if needed.
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P • Consider intubation
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • If no improvement and transport time lengthy, consider epinephrine 1:1,000 0.3 mg SQ, if not contraindicated. Specific contraindications for epinephrine in this situation: • Patient with cardiac history • Tachycardia / hypertension • Age > 40 years
P • Consider RSI protocol (p. 28) or sedation-facilitated intubation protocol (p. 27) if patient in respiratory failure. Revised 2002 -36- Seizures
STANDING ORDERS:
ALL • If pregnant refer to Toxemia of Pregnancy protocol (p. 38) • Routine medical care (p. 2) • If seizures are recurrent or status epilepticus, immediate transport • Protect patient from injury; maintain airway • Assess blood glucose. (EMT-D’s can perform fingerstick glucose testing only if the corps has prior off-line approval by its medical director. Glucose may be administered without checking BG if EMT is not cleared for fingerstick testing.)
I / CC / P • IV NS at KVO
CC / P • If patient is hypoglycemic, administer D50 per criteria under Altered Mental Status protocol (p. 9)
P • Lorazepam 1-2 mg IV or IM • OR Diazepam 2-5 mg.
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • Lorazepam 1-2 mg IV or IM OR • Diazepam 2-5 mg IV
CC / P • If seizures continue, Lorazepam 0.5-1 mg IV or IM, (Max 5 mg) or Diazepam 1-2.5 mg IV (Max 10 mg) may be repeated in 5-10 min. to maximum 5 mg.
SUPPORT AIRWAY AND BREATHING AS NEEDED. Revised 2002 -37- Toxemia of Pregnancy
STANDING ORDERS:
ALL • Obtain a careful OB history and blood pressures • Position patient on left side • Apply high flow O2 • Immediate transport
I / CC / P • IV NS at KVO
CC / P • Cardiac monitor • Contact Medical Control ASAP for BP > 150 systolic, or > 90 diastolic
If seizures develop:
• Refer to seizure protocol (p. 37)
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • Magnesium sulfate 4 g IV, then 2 g/hr IV drip.
• If hypotension, respiratory depression or stupor develops after administration of magnesium sulfate, consider Calcium gluconate 5-10 mEq (10-20 ml).
Revised 2002 -38- Pediatric Protocols
< 16 Years of Age **Technicians should utilize the Broselow tape to Routine Pediatric Medical Care – General determine medication dosages and equipment size selection. DEFINITIONS
Neonate – Newborn – 1 mos Infant – 1 mos – 1 yr Toddler – 1 – 3 yrs Child – 3 – 16 yrs
• Pediatric care equipment will always be brought to the patient, to include: • Oxygen, suction, bag with pediatric BP cuff, pediatric oxygen masks, pediatric BVM, and pediatric oropharyngeal airways. • Advanced airway kit (I / CC / P) • Monitor / defibrillator, medication box, and telemetry unit (CC / P)
• Ensure adequate oxygenation. Administer high flow oxygen to any patient who needs it. Assist ventilations and suction prn. Parents may administer “blow-by” oxygen to very young children.
• Continued monitoring and serial vital signs as needed. EKG monitoring by CC / P as necessary.
• Avoid separation from parents whenever possible (may further aggravate distress).
• Airway and oxygenation are the primary management tools; medications and IV / IO therapy are secondary.
• Pediatric patients more vulnerable to hypothermia. Assure warm environment.
• Do not forget communication with parents.
• Use Broselow Tape for weight estimation, drug dosages, and equipment size selection whenever possible.
Revised 2002 -41- Pediatric Normal Weights / Vital Signs
Normal AGE WT (KG) Systolic BP HR Resp Rate
Birth 3.5 60-80 80-160 30-60 6 mos 7 70-100 100-120 30-50 1 yr 10 80-85 100-120 25-35 2 yr 13 80-85 80-100 20-30 3 yr 15 80-85 80-100 20-30 4 yr 17 80-85 80-100 20-30 5 yr 19 80-85 80-100 20-30 6 yr 22 80-85 80-100 20-30 7 yr 25 80-85 70-90 15-25 8 yr 28 80-85 70-90 15-25 9-10 yrs 30 90-130 70-90 10-20 8-12 yrs 37 90-135 70-90 10-20
Pediatric Hypotension
To rapidly determine hypotension status in pediatric patients:
Age < 1 mos Systolic BP < 60 1 mos - 1 yr < 70 > 1 yr < 70 + (2 x age)
Revised 2002 -42- Pediatric Airway Management – Equipment Sizes*
Laryngoscope Suction AGE Blade ETT Catheter Preemie Miller 0 2.5-3.0 uncuffed 6 French Term Infant Miller 0-1 3.0-3.5 uncuffed 6 French 6 mos Miller 0-1 3.5-4.0 uncuffed 8 French 1 yr Miller 1 4.0-4.5 uncuffed 8 French 2 yrs Miller 2 4.5 uncuffed 8 French 4 yrs Miller 2 5.0 uncuffed 10 French 6 yrs Miller 2 5.5 uncuffed 10 French 8 yrs Miller 2, Mac 2 6.0 cuffed 10 French 10 yrs Miller 2, Mac 2 6.5 cuffed 12 French 12 yrs Miller 3, Mac 3 7.0 cuffed 12 French Adolescent Miller 3, Mac 3 7.0-8.0 cuffed 12 French *Use Broselow tape to assist in determination
Apgar Score
Points Category 0 1 2 Appearance Blue / Pale Body pink / Completely pink (skin color) Extremities blue Pulse Absent <100 > 100 (heart rate) Grimace No response Grimaces Cries (irritability) Activity Limp Some flexion of Active motion (muscle tone) extremities Respiratory Absent Slow / Irregular Strong cry (effort) Performed 1 minute and 5 minutes after birth
Score: 7 - 10 active and vigorous neonate 4 - 6 moderately depressed neonate < 4 severely depressed neonate Revised 2002 -43- Pediatric Drug Dosage Table
Minimum Maximum Administratio Medication Dosage Dose Single Dose n Routes Adenosine 0.1-0.2 mg/kg – 12 mg IV, IO Albuterol 1.25-2.5 mg 1.25 mg 2.5 mg Nebulizer Amiodarone 5 mg/kg bolus - - IV/IO Atropine 0.02 mg/kg 0.1 mg 0.5-1.0 mg IV, IO, ET Diazepam 0.05-0.3 mg/kg - 5 mg IV, IO, ET Diphenhydramine 1-2 mg/kg – 50 mg IV, IM Dopamine 2-20 µg/kg/min – 20 µg/kg/min IV, IO Epi 1:1000 See Below Epi 1:10,000 See Below Glucagon 0.1 mg/kg 0.1 mg 1 mg IM Ipecac < 5 y/o 15 ml 15 ml 30 ml PO > 5 y/o 30 ml Lidocaine 1 mg/kg – 3 mg/kg IV, IO, ET Lorazepam 0.1 mg/kg - 1 mg IV, IO, IM, ET Morphine sulfate 0.1 mg/kg – 5 mg IV, IO, IM Naloxone ≤ 5 y/o or < 20 kg 0.1 mg/kg – 2 mg IV, IO, ET, > 5 y/o or > 20 kg 2 mg IM 8.4% Sodium 1 mEq/Kg – 50 mEq IV, IO bicarbonate (use 4.2% Sodium bicarbonate solution for infants < 3 months) NOTE: drugs administered via ETT route should be diluted to a volume of 3-5 ml of normal saline and follow with several positive-pressure ventilations
EPINEPHRINE 1:1000
Cardiac Arrest: Initial dose 0.1 mg/kg ET
Subsequent doses 0.1 mg/kg IV/IO/ET
*Epinephrine 1:1000 doses up to 0.2 mg/kg IV/IO may be effective.
Asthma: 0.01 mg/kg up to 0.3 mg IM or SQ
EPINEPHRINE 1:10,000
Cardiac Arrest: Initial dose 0.01 mg/kg IV/IO Airway Management – Pediatrics Revised 2002 -44- STANDING ORDERS:
ALL • Establish patent airway – Manually open airway prn – Head tilt / chin lift (non-trauma) – Modified jaw thrust (trauma) • Suction prn • Oropharyngeal / nasopharyngeal airway prn • Ventilation with BVM and 100% oxygen prn
I / CC / P • Appropriate airway management with BVM and adjunct airways. • Attempt orotracheal intubation up to three times per patient in the following situations: – Cardiac / respiratory arrest – Suspected thick meconium aspiration in newborn • Manual in-line neck stabilization should be employed for trauma • Uncuffed tubes only should used in patients under age 8. • Use Broselow tape for definitive tube size choice. • In other situations requiring definitive airway management, CONTACT MEDICAL CONTROL BEFORE INTUBATING. Especially true for suspected epiglottitis, status asthmaticus, conscious patients, and severe oral maxillofacial trauma. • Following intubation, ventilate patient with BVM and 100 % oxygen, assuring that the pop-off valves, if present, are disengaged. Auscultate for bilateral breath sounds and absence of epigastric sounds.
Note: Confirmation of tube placement by ETCO2 detector device is MANDATORY in pediatric patients > 2 kg. Because, however, ETCO2 detectors are less accurate in cardiopulmonary arrest, it is recommended that further confirmation be obtained with an esophageal detector device.
Oxygen Therapy STANDING ORDERS:
ALL • Administer oxygen to patients requiring high concentrations of oxygen using an appropriate size nonrebreather mask. The flow rate should be sufficient to keep the bag on the mask inflated (10-15 lpm). Patients who do not tolerate the mask should have a stream of oxygen blown as close to the face as possible. Revised 2002 -45- Airway Obstruction (Foreign Body)
STANDING ORDERS :
Conscious Patient • Assess air exchange and oxygenation status of patient • AIRWAY NOT TO BE UNNECESSARILY STIMULATED OR EXAMINED in situation of possible epiglottitis / severe croup. See Respiratory Distress protocol (p. 71), and initiate rapid transport. • Manual maneuvers to clear airway to be used only in case of foreign body obstruction. Perform no blind finger sweeps.
ALL ______|______| | Adequate Air Exchange – Inadequate Air Exchange – Able to cough / speak / breathe / cry Cannot cough / speak / breathe / cry
• Encourage coughing • < 1 y/o – administer 5 back blows • Rapid transport with head lower than body • Avoid agitating child (may worsen • Administer 5 chest thrusts (< 1 y/o) distress) or abdominal thrusts (> 1 y/o) • Oxygen as tolerated • Clear oropharynx prn • Repeat as necessary • Rapid transport
Unconscious patient
ALL • Manually open airway, attempt to ventilate with 2 breaths • Reposition and reattempt to ventilate • < 1 y/o administer 5 back blows with head lower than body • Administer 5 chest thrusts (< 1 y/o) or abdominal thrusts (> 1 y/o) • Inspect mouth, suction, and remove visible obstruction. Do not perform blind finger sweep • Repeat this sequence as needed
CC / P • Attempt direct laryngoscopy and removal of foreign object with Magill forceps
If initial efforts to dislodge object are unsuccessful, begin rapid transport and continue efforts en route.
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
P • Needle cricothyrotomy, if still obstructed Revised 2002 -46- IV Therapy
STANDING ORDERS:
I / CC / P • Ensure adequate oxygenation and patent airway • Vascular access to be performed only where expressly called for by specific protocols • IV placement may be difficult. Excessive time should not be spent establishing IV in any situation (no more than 5 minutes) • Use readily accessible veins (in hand or antecubital area) • Unless otherwise specified, NS is primary fluid of choice. • Run at KVO rate (10 ml/hr) or rate specified by protocol
I / CC / P • For patients under 6 y/o, but older than 1 mos, use intraosseous technique for establishing vascular access in situations where it is rapidly required (cardiac arrest, hypotension, shock) • Place IO line using NS at rate specified by protocol
Revised 2002 -47- Fluid Challenge / Replacement Routine Trauma Triage Protocol (Pediatrics)
STANDING ORDERS:
ALL • Confirm indications for fluid challenge: – Hypotension – Tachycardia with evidence of poor peripheral perfusion – Absent peripheral pulses – Altered mental status – Cold extremities – Capillary refill > 2 sec – Cardiac disease / CHF absent (check for liver edge / hepatomegaly, rales)
CC/ P • Establish IV • Bolus 20 ml/kg NS IV
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
I • Establish IV • Bolus 20 ml/kg NS IV
CC / P • OR establish IO line (using NS to administer bolus 20 ml/kg NS IV)
ABSOLUTE ON-LINE MEDICAL CONTROL:
I • OR establish IO line to administer bolus 20 ml/kg NS IV
I / CC / P • Repeat fluid boluses as specified by medical control
Revised 2002 -48- I. Blunt or Penetrating Trauma With Unmanageable Airway • Except for special circumstances, on-scene time should not exceed ten minutes. • Condition present: • Medical command may be contacted any time during the assessment process – begin airway management measures • If there are any questions, concerns, or extenuating circumstances (weather, etc.) it – transport to nearest hospital is recommended that medical command be contacted • Condition absent– assess for: II. Trauma Arrest • Condition present: – begin CPR Revised 2002 -49- – transport to nearest hospital • Condition absent– assess for: III. Multi-system Trauma With: – unstable V.S. – hemodynamic compromise (shock symptoms) – respiratory compromise (RR < 10 or > 28) – altered mental status or LOC > 5 minutes • Condition present: – begin routine trauma care – transport to trauma center – if > 15 min. to trauma center, launch helicopter • Condition absent– assess for: IV. Anatomic Injury – penetrating injury head, neck, torso, groin – 2° / 3° burns > 15% BSA, or any burn involving face, airway, hands, feet, or genitalia – partial or complete paralysis of new onset – flail chest / major blunt chest injury – > 2 long bone fractures – suspected open or depressed skull fracture – suspected unstable pelvis or pelvic fracture – partial or full amputation proximal to digits • Condition present: – begin routine trauma care – transport to trauma center – if > 15 min. to trauma center, launch helicopter • Condition absent– assess for: V. Increased Risk For Severe Injury – ejection from vehicle – death of occupant in same vehicle – auto crash w/ significant intrusion into passenger compartment – significant fall from a height – bent steering column – significant auto-pedestrian impact – significant motorcycle, ATV, horse, or bicycle incident – major chronic illness (respiratory, cardiac, etc.) – high risk medical condition (on anticoagulants like coumadin, etc.) – pregnancy > 20 week gestation • Condition present: – begin routine trauma care – if pt < 18 y/o, transport to trauma center – if medical command not available, transport to trauma center – if decision made for trauma center and if > 15 min. to trauma center, launch helicopter • Condition absent– assess for: Routine Trauma Care (Pediatrics) – Cont. Altered Mental Status – Unknown Origin
Determine Major Trauma Criteria (see previous page) Definition: GCS < 15. See below. STANDING ORDERS : STANDING ORDERS : ______|______| | ALL • Routine pediatric medical care (p. 41). Assure airway patency and administer high flow O2 – hypoxia is a common cause of Criteria Present Criteria Absent decreased LOC in children. • Consider possibility of head trauma, child abuse. Trauma procedures prn. Refer to Head Trauma protocol (p. 64). • Spinal immobilization • Perform secondary survey • Thorough scene assessment for possibility of poisoning, etc. • IV NS, at KVO or: • Stabilize patient prn Obtain history and consider other medical cause (meningitis, • Fluid Challenge protocol (p. 48) • IV NS prn at KVO. etc.) • Consider second IV line • Expedite transport to closest • Rapid transport • EKG monitoring appropriate facility • Assess blood glucose. (EMT-D’s can perform fingerstick • Transport to trauma center or • Contact medical control ASAP glucose testing only if the corps has prior off-line approval by its contact Medical Control if patient medical director. Glucose may be administered without will not arrive at trauma center checking BG if EMT is not cleared for fingerstick testing.) within one hour from time of injury ______|______| |
FOR TRAUMATIC ARREST OR OBSTRUCTED AIRWAY, TRANSPORT Glucose < 60 Glucose > 60 TO CLOSEST EMERGENCY FACILITY. CC / P CC / P AS NEEDED, see also protocols for: • Establish vascular access • Naloxone (Narcan) 0.1 mg/kg IM • D25 2-4 ml/kg IV/IO push or ET. Repeat as needed. Cardiac Arrest (p. 55) • If unable to place IV, or IO not Pediatric Chest Trauma (p. 62) available, glucagon Pediatric Head Trauma (p. 64) 0.1 mg/kg IM (up to 1 mg)
* PEDIATRIC HYPOTENSION – To rapidly determine hypotensive status in pediatric patients, lower limits of systolic BP are:
Age < 1 mos: Systolic BP < 60 Age 1 mos – 1 y/o: Systolic BP < 70 Age > 1 y/o: Systolic BP < 70 + (2 x age)
Revised 2002 -50- Analgesia (Pain Control) Revised 2002 -51-
STANDING ORDERS:
ALL • Routine pediatric medical care (p. 41)
• Identify and treat cause of the underlying cause of pain when possible
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC/P • Morphine sulfate 0.1 mg/kg IV, IO, IM or SQ q5 min to desired analgesic response (max dose 5 mg). • May repeat as ordered by Medical Control • If hypotension, respiratory depression or stupor develop after morphine, administer Naloxone (Narcan) 0.1 mg/kg (up to 2.0 mg) IV, IO or IM.
Revised 2002 -52- Anaphylactic Shock / Allergic Reaction
STANDING ORDERS :
ALL • Routine pediatric medical care (p. 41) • Airway management and oxygenation with high-flow oxygen • If patient has own epinephrine auto-injector, all EMTs may assist the patient, or parent, in administering the auto-injector. • If agency has been approved to carry an epinephrine auto- injector, see epinephrine auto-injector protocol (p. 85) • Rapid transport.
I / CC / P • If hypotensive*, establish vascular access with NS and Fluid Challenge protocol (p. 48). See Pediatric Hypotension Chart / Formula (p. 42)
CC / P • Epinephrine 1:1,000 0.01 mg/kg IM or SQ (up to 0.3 mg), if hypotensive. • Diphenhydramine (Benadryl) 1-2 mg/kg (up to 50 mg) IM or IV/IO (all patients). • Nebulized albuterol, if wheezing present. Albuterol dosage as follows: – < 1 y/o: 1.25 mg – > 1 y/o 2.5 mg
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P • Repeat epinephrine 1:1,000 0.01 mg/kg IM or SQ prn, if still hypotensive.
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • If patient remains hypotensive, contact Medical Control for possible use of epinephrine 1:10,000 IV at dosage to be determined by Medical Control.
* PEDIATRIC HYPOTENSION – To rapidly determine hypotensive status in pediatric patients, the lower limit of normal systolic BP’s are as follows:
Age < 1 mos: Systolic BP < 60 Age 1 mos – 1 y/o: Systolic BP < 70 Age > 1 y/o: Systolic BP < 70 + (2 x age)
Revised 2002 -53- Burns – Thermal
STANDING ORDERS :
ALL • ASSURE SCENE SAFETY • Remove constricting clothing and jewelry. • High flow O2 (10-15 lpm) if airway burn / inhalation injury suspected. • Do not rupture blisters or apply any ointment or medication to burns. • Cover burns with sterile gauze soaked in saline*. Avoid ice or cold compresses • Maintain body temperature (keep patient covered) • Consider transport to a Burn Unit (see Trauma protocols p. 49)
I / CC / P • If 2° burns cover > 15 % BSA, start IV of NS at 10 ml/kg/hr.
CC / P • Analgesia protocol (p. 52)
* If burns > 15% BSA, remove compresses after 5 minutes and dress with dry sterile dressings.
Burns – Electrical
STANDING ORDERS :
ALL • Determine current source. Remove patient after current shut off. USE CAUTION! • Cover entrance and exit burns with dry sterile dressing.
I / CC / P • Start IV NS at KVO rate.
CC / P • Monitor EKG ASAP and treat arrhythmias as appropriate. • Analgesia protocol (p. 52)
Burns – Chemical
STANDING ORDERS :
ALL • Remove clothing, jewelry, etc. and flush skin with large quantities of water. • Flush eyes with NS, if appropriate.
CC / P • Analgesia protocol (p. 52) Revised 2002 -54- Cardiac Arrest – General
The following applies in all pediatric cardiac arrest situations.
Pediatric cardiac arrest is usually the end result of unchecked hypoxia or shock. It rarely results from a primary cardiac event, except in the presence of congenital defects. The treatment plan must keep this in mind.
STANDING ORDERS:
ALL • Routine pediatric medical care (p. 41), CPR and airway management up to level of training. • CPR to be continued at all times except during defibrillation and/or interruptions < 30 sec for patient transfer. • Initiate early transport. • Utilize ALS or initiate rapid transport to ALS (hospital or mobile). • Advise receiving hospital ASAP.
EMT-D / I • Automatic / semi-automatic defibrillator not to be used for pediatrics under 80 lbs. If weight > 80 lbs (approx 40 kg), refer to adult arrest protocols.
EMT-I • For IV access use NS. NOT TO DELAY TRANSPORT.
CC / P • For vascular access use NS. • Initiate immediate intubation and CPR, and ventilate with 100% oxygen. Use “quick look” paddles to determine rhythm and connect cardiac monitor ASAP. With Pediatric patients, unlike adults, intubation should take first priority.
Revised 2002 -55- Cardiac Arrest – Asystole
Also see Cardiac Arrest (pediatric) – General protocol (p. 55)
STANDING ORDERS:
CC / P • Continue CPR. • Assure adequate airway and oxygenation. Hyperventilate with 100 % O2 • Establish vascular access using NS. If able to place ETT, may give initial epinephrine by ET route. • Assess blood glucose. • Administer epinephrine, dosage as follows: INITIAL DOSE: Epinephrine 0.01 mg/kg 1:10,000 IV/IO OR Epinephrine 0.1 mg/kg 1:1,000 ET SUBSEQUENT DOSES: Epinephrine 0.1 mg/kg 1:1,000 IV/IO/ET q5 min • Begin transport as soon as possible. Reassess airway and ventilation.
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P SUBSEQUENT DOSES: • Epinephine may be increased up to 0.2 mg/kg IV/IO q 3-5 minutes. • Transcutaneous external pacemaker, if available. If child weighs: > 15 kg – use adult leads < 15 kg – use pediatric leads
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • May consider Sodium bicarbonate 8.4 % solution 1 mEq/kg IV/IO if: • Known pre-existing non-respiratory acidosis • Known pre-existing hyperkalemia • Drug overdose (especially tricyclic antidepressant) • Long arrest interval (> 10-15 min) and patient is intubated
( use 4.2% Sodium bicarbonate solution for infants < 3 months)
Revised 2002 -56- CARDIAC ARREST – VF/Pulseless VT Cardiac Arrest – PEA Also see Cardiac Arrest (pediatric) – General protocol (p. 55)
STANDING ORDERS: Also see Cardiac Arrest (pediatric) – General protocol (p. 41)
CC / P • Continue CPR. STANDING ORDERS: • Assure adequate airway and oxygenation. Hyperventilate with 100 % O2 CC / P • Assure adequate airway and oxygenation. Hyperventilate with • Defibrillate up to 3 times prn (2 j/kg, 4 j/kg, 4 j/kg) 100 % O2 • Establish vascular access using NS. If able to place ETT, may • Establish vascular access using NS. give initial epinephrine by ET route. • Administer epinephrine, dosage as follows: • Administer epinephrine, dosage as follows: INITIAL DOSE: INITIAL DOSE: Epinephrine 0.01 mg/kg 1:10,000 IV/IO OR Epinephrine 0.01 mg/kg 1:10,000 IV/IO OR Epinephrine 0.1 mg/kg 1:1,000 ET Epinephrine 0.1 mg/kg 1:1,000 ET SUBSEQUENT DOSES: SUBSEQUENT DOSES: Epinephrine 0.1 mg/kg 1:1,000 IV/IO/ET Epinephrine 0.1 mg/kg 1:1,000 IV/IO/ET • Assess and treat cause of PEA (hypoxia, hypovolemia, • Defibrillate 4 j/kg hypoglycemia, hypothermia, cardiac tamponade, acidosis, • Lidocaine 1 mg/kg IV/IO or ET tension pneumothorax.) • OR amiodarone 5 mg/kg bolus IV/IO • Begin transport ASAP. Reassess airway and ventilation. • Defibrillate 4 j/kg • Contact medical control for further orders. • Repeat lidocaine 1 mg/kg IV/IO or ET • Defibrillate 4 j/kg ON-LINE MEDICAL CONTROL ( standin g order if communication failure): • Begin transport ASAP. Reassess airway and ventilation. • Contact medical control for further orders. CC / P SUBSEQUENT DOSES: • Epinephrine doses up to 0.2 mg/kg IV/IO may be effective. ON-LINE MEDICAL CONTROL ( standin g order if communication failure): Repeat q 3-5 minutes throughout arrest.
CC / P SUBSEQUENT DOSES: • Epinephrine may be increased up to 0.2 mg/kg IV/IO q 3-5 min. • OR Consider amiodarone, 5 mg/kg bolus IV/IO
• Defibrillate 4 j/kg, 30-60 sec after each med administration • Use anterior-posterior placement of paddles if body area is small
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • Consider Sodium bicarbonate 8.4 % solution 1 mEq/kg IV/IO if: • Known pre-existing non-respiratory acidosis • Known pre-existing hyperkalemia • Drug overdose (especially tricyclic antidepressant) • Long arrest interval (> 10-15 min) and patient is intubated
(use 4.2% Sodium bicarbonate solution for infants < 3 months) Revised 2002 -57- Revised 2002 -58- Cardiac – Bradycardia Cardiac – SVT
STANDING ORDERS : STANDING ORDERS: ALL • BRADYCARDIA IS ALMOST ALWAYS THE RESULT OF HYPOXIA IN PEDIATRIC PATIENTS. ASSURE AIRWAY ALL • SVT rate usually >200 in infants and children. PATENCY, ADMINISTER HIGH FLOW O2, AND ASSIST VENTILATIONS. • Routine pediatric medical care (p. 41). • Routine pediatric medical care (p. 41). • Administer high flow O2 and assure airway patency. • For newborns, refer to Neonatal Resuscitation protocol (p. 69) • Rapid transport. CC / P • Assess hemodynamic status / stability of patient • Administer chest compressions if, despite ventilation and • Wide complex SVT is very uncommon in the pediatric patient. oxygenation, pulse remains < 60 and there is evidence of: Wide complex tachyarrhythmias should be treated as VT. – Poor perfusion (slow capillary refill, altered mental status) – Hypotension ______|______– Respiratory difficulty | |
I / CC / P • If evidence of poor perfusion, Fluid Challenge protocol (p. 48), Unstable* Stable if signs of CHF are absent. ON-LINE MEDICAL CONTROL: • Valsalva maneuver ON-LINE MEDICAL CONTROL ( standin g order if communication failure): • If IV access already available, ABSOLUTE ON-LINE: CC / P • If continued pulse < 80 and evidence of poor perfusion, adenosine 0.1 mg/kg rapid IVP. administer epinephrine 1:10,000 0.01 mg/kg IV/IO OR May repeat in 1-2 min. at 0.2 • If IV access already available, epinephrine 1:1,000 0.1 mg/kg ET. Repeat at same dose q3-5 mg/kg. (Maximum single dose is adenosine 0.1 mg/kg rapid IVP. minutes. 12 mg) May repeat in 1-2 min. at 0.2 • If continued pulse < 80 and evidence of poor perfusion following • Sync cardioversion 0.5 j/kg mg/kg. (Maximum single dose is epinephrine, medical control may order atropine 0.02 mg/kg • Sync cardioversion 1 j/kg 12 mg) IV/IO OR 0.04 mg/kg ET. May repeat once in 5 minutes. • Sync cardioversion 2j/kg • Transcutaneous external pacemaker, if available. If child • Sync cardioversion 4 j/kg weighs: • Further therapy per medical > 15 kg – use adult leads control < 15 kg – use pediatric leads
* "Unstable" is defined as one or more of the following: – Hypotension * PEDIATRIC HYPOTENSION – To rapidly determine hypotensive status in – Chest pain pediatric patients, the lower limits of systolic BP’s are: – Signs of CHF – Poor peripheral pulses Age < 1 mos: Systolic BP < 60 – Capillary refill > 2 seconds in warm extremity Age 1 mos – 1 y/o: Systolic BP < 70 – Cool, mottled, cyanotic distal extremities Age > 1 y/o: Systolic BP < 70 + (2 x age)
Revised 2002 -59- Revised 2002 -60- Cardiac – VT Chest Trauma
If there is no pulse, refer to the Cardiac Arrest – VF/Pulseless VT protocol (p. 57)
STANDING ORDERS : Includes pneumothorax, tension pneumothorax, penetrating chest injuries, rib fractures, and flail chest. ALL • Routine pediatric medical care (p. 41) • Administer high flow O2. STANDING ORDERS : • In the absence of congenital heart defects, ventricular dysrhythmias in pediatrics are frequently due to electrolyte ALL • Routine pediatric trauma care (pp. 49, 50) deficiencies or hypoxia. • Stabilize and do not remove penetrating objects • Use occlusive dressing to seal open wounds CC / P • Assess hemodynamic status / stability of patient • Stabilize flail segments with bulky dressings • Rapid transport ______|______| | ABSOLUTE ON-LINE MEDICAL CONTROL: Unstable* Stable CC / P • If signs / symptoms of tension pneumothorax present, perform ON-LINE MEDICAL CONTROL: • Attempt IV NS needle thoracostomy • Sync cardioversion 0.5 j/kg • Contact medical control • Sync cardioversion 1 j/kg • Sync cardioversion 2j/kg • Sync cardioversion 4 j/kg • Lidocaine 1 mg/kg IV/IO; reattempt cardioversion at 4 j/kg
Use pediatric paddles (if available) for children ≤ 10 kg. Use adult paddles for children > 10 kg. If no pediatric paddles available, use anterior - posterior placement of adult paddles.
* "Unstable" is defined as one or more of the following: – Hypotension – Chest pain – Signs of CHF – Poor peripheral pulses – Capillary refill > 2 seconds in warm extremity – Cool, mottled, cyanotic distal extremities
Revised 2002 -61- Revised 2002 -62- Diabetic Emergencies
STANDING ORDERS :
ALL • Routine pediatric medical care (p. 41) • Assess signs, symptoms and medical history • If patient appears hypoglycemic, administer glucose gel under tongue while protecting airway. If patient is conscious they may eat any form of available sugar, such as non-diet soda, candy, orange juice, or granular sugar • Administer glucose gel if you are unsure if patient is hypoglycemic • A reasonable attempt should be made to assess blood glucose prior to giving glucose. (EMT-D’s can perform fingerstick glucose testing only if the corps has prior off-line approval by its medical director. Glucose may be administered without checking BG if EMT is not cleared for fingerstick testing.)
______|______| |
Glucose < 60 Glucose > 300
CC / P I / CC / P • Establish vascular access • Consider Fluid Challenge (p. 48), • D25 2-4 ml/kg IV/IO slow push if patient shows evidence of shock over 2 min • Reassess blood glucose • Repeat D25 prn • If not able to establish access, administer glucagon 0.1 mg/kg IM (up to 1 mg)
If level of consciousness does not improve in the hypoglycemic patient following administration of D25, proceed with Altered Mental Status protocol (p. 51).
Revised 2002 -63- Head Trauma
STANDING ORDERS:
ALL • Administer high flow O2 and assure airway patency • If respirations slow / shallow, assist with 100 % O2 • If spontaneous respirations absent: • Begin immediate ventilation with 100 % O2 • Hyperventilate patient with appropriate size ambu bag • Airway management up to level of training (I, CC, P only: intubation preferred with appropriate spinal precautions) • Refer to Cardiac Arrest protocols prn • All patients to receive spinal immobilization as appropriate • Monitor vital signs and level of consciousness • Refer to Seizure protocol (p. 72) prn • Consider possibility of other trauma. Refer to Trauma protocols (pp. 49, 50) prn • Consider possible child abuse
I / CC / P • If hypotensive (p. 42), establish IV NS and provide fluid bolus as per Fluid Challenge protocol (p. 48). • Ventilate at 15 to 20 breaths/minute if patient undergoes rapid decompensation in mental status suggesting herniation syndrome. • Contact medical control
* PEDIATRIC HYPOTENSION – To rapidly determine hypotensive status in pediatric patients:
Age < 1 mos: Systolic BP < 60 Age 1 mos – 1 y/o: Systolic BP < 70 Age > 1 y/o: Systolic BP < 70 + (2 x age) Revised 2002 -64- Hyperthermia – Heat Exhaustion / Heat Stroke
STANDING ORDERS :
ALL • Routine pediatric medical care (p. 41) • Cool patient using whatever means immediately available – If temp < 41° C (mild hyperthermia), lukewarm towels – If temp > 41° C (severe hyperthermia), cold towels with crushed ice available • If patient has seized or is seizing, see Pediatric Seizure protocol (p. 72)
I / CC / P • IV NS at KVO • If dehydration / shock present, Fluid Challenge protocol (p. 48)
Also proceed with Altered Mental Status protocol (p. 51), if there is a decreased level of consciousness.
Revised 2002 -65- Hypotension / Shock
Defined as inadequate tissue perfusion as evidenced by one or more of the following: • Poor peripheral pulses • Delayed capillary refill • Altered mental status • Cool, cyanotic distal extremities • Tachycardia in conjunction with any of the above
DECREASED BLOOD PRESSURE IS A VERY LATE SIGN OF SHOCK IN PEDIATRIC PATIENTS. THE PRESENCE OF HYPOTENSION SUGGESTS SEVERE AND DECOMPENSATED SHOCK. LOOK CAREFULLY FOR THE EARLY SIGNS OF SHOCK, PER ABOVE.
STANDING ORDERS:
ALL • Routine pediatric medical (p. 41) or trauma (pp. 49, 50) care as appropriate • Consider other treatable causes – hypoglycemia, hypoxia, anaphylaxis
I / CC / P • Fluid Challenge protocol (p. 48), if signs / symptoms of CHF absent
ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • If no improvement and no history consistent with fluid loss, Dopamine 5-10 µg/kg/min IV/IO drip
* PEDIATRIC HYPOTENSION – To rapidly determine hypotensive status in pediatric patients:
Age < 1 mos: Systolic BP < 60 Age 1 mos – 1 y/o: Systolic BP < 70 Age > 1 y/o: Systolic BP < 70 + (2 x age)
Revised 2002 -66- Hypothermia
STANDING ORDERS :
ALL • PARTICULARLY WITH NEONATES AND INFANTS, HYPOTHERMIA CAN BE RAPID IN ONSET. The environment should be warm enough for the baby. Wrap newborns in blanket and use ambulance heater. Ambulance temperature should be higher than normal room temperature. Warming of newborns is an imperative part of neonatal resuscitation. • Routine pediatric medical care (p. 41) • Remove wet clothing, protect patient from environment • Avoid rough handling • Rewarming of severely hypothermic patient best carried out in hospital • Rapid transport
In the event of hypothermic cardiac arrest, medical control should be contacted prior to any medication administration.
Proceed with Altered Mental Status protocol (p. 51) if there is a decreased level of consciousness.
Revised 2002 -67- Near Drowning
STANDING ORDERS :
ALL • Routine pediatric medical (p. 41) or trauma (pp. 49, 50) care as appropriate. • Assure airway patency and administer high flow O2 • Refer to Cardiac Arrest protocols prn • Spinal precautions as appropriate • Treat hypothermia prn • Transport ALL patients regardless of presence or absence of symptoms (development of life-threatening symptoms may be delayed). • Unless in cardiac arrest, transport on side. There is a high risk of vomiting and aspiration.
For pediatric downing victims, if there is any question about the appropriateness of beginning resuscitation efforts, begin CPR and contact medical control for advice on how to proceed.
Revised 2002 -68- Neonatal Resuscitation Revised 2002 -69-
Resuscitation of the newborn rarely requires invasive procedures. The EMT must be most concerned with providing adequate oxygenation, airway patency, and warmth. Signs of inadequate oxygenation include: quiet, not crying; diffuse, dark cyanosis over entire body (some cyanosis may be present initially but baby should "pink up" rapidly); apnea or gasping respirations; pulse rate < 100 / min; flaccid, not moving extremities.
STANDING ORDERS : ALL • Suction mouth and nose as soon as head is visible. Do not put bulb syringe into throat. *** (CC / P: IF THICK MECONIUM IS PRESENT, ET INTUBATION SHOULD BE PERFORMED ASAP AND THE TRACHEA SUCTIONED). • Keep baby at level of vagina until umbilical cord is cut. Cord should be clamped and cut 30-45 seconds after birth. • Dry baby, warm with blankets, provide tactile stimulation. • IF RESPIRATIONS < 20 OR SIGNS OF INADEQUATE OXYGENATION ARE PRESENT, ADMINISTER 100% O2 AND SUCTION THE AIRWAY • IF NO IMPROVEMENT, VENTILATE WITH 100 % O2 USING 450-ML BVM AT A RATE OF 40-60 / MIN • Assess heart rate ______|______| | | < 60 bpm 60 – 100 bpm > 100 bpm STANDING ORDERS : STANDING ORDERS : STANDING ORDERS : ALL ALL ALL • BEGIN CHEST • BVM VENTILATION • MAINTAIN COMPRESSIONS AND WITH 100 % O2 OXYGENATION WITH VENTILATION HIGH FLOW O BVM • BEGIN RAPID 2 WITH O 100% 2 TRANSPORT • BEGIN RAPID • BEGIN RAPID TRANSPORT TRANSPORT
I / CC / P • Contact Medical Control • Establish IV / ET access
ON-LINE MEDICAL CONTROL: CC / P • Epinephrine 1:10,000 0.01 mg/kg ET. May be repeated q3-5 min., if required. Once adequate respirations and pulse rate are established, continue monitoring the infant and provide supplemental oxygen as needed using tent of aluminum foil. Keep infant warm at all times. (CHECK BLOOD GLUCOSE IF TIME PERMITS) Poisoning / Overdose
STANDING ORDERS:
ALL • ASSURE SCENE SAFETY Revised 2002 -70- • Remove patient from source and attempt to identify poison • Remove topical poisons from skin or eye • remove contaminated clothing • brush away particulate matter • irrigate with large amount of saline or tap water, unless contraindicated
• Assess Modified Glasgow Coma Scale (p. i)
-- GCS < 15, refer to Altered Mental Status protocol (p. 51)
– GCS = 15, routine pediatric care (p. 41) and assess for shock
______|______| |
Shock absent Shock present
• CONTACT MEDICAL CONTROL • Refer to Hypotension / Shock • Save all emesis, if possible; bring protocol (p. 66) it, poison and / or poison container(s) to hospital
ABSOLUTE ON-LINE:
• Consider Ipecac / water as follows: • Age 1-5 y/o: ipecac syrup 15 ml PO followed by 1 large glass of water or other clear liquid • Age > 5 y/o: ipecac syrup 30 ml PO followed by 2 large glasses of water or other clear liquid • Sorbitol-free activated charcoal 1-2 g/kg PO Respiratory Distress Seizures
Secondary to foreign body, croup, epiglottitis, asthma, bronchiolitis, pneumonia, etc.
STANDING ORDERS : STANDING ORDERS :
ALL • Routine pediatric care (p. 41). Ensure airway patency and ALL • Routine pediatric medical care (p. 41) adequate oxygenation – administer high flow oxygen • Assure airway patency and administer high flow O2 • If possibility of epiglottitis (hoarseness, stridor, choking, • If status epilepticus, begin rapid transport. ( Status epilepticus is drooling), AIRWAY NOT TO BE STIMULATED OR defined as one continuous seizure for > 20 minutes, or repetitive EXAMINED. Do not lie patient down. seizures without regaining of consciousness for > 20 minutes.) • Consider possible foreign body obstruction – refer to Airway • Consider febrile seizures – if fever present, remove clothing Obstruction protocol (p. 46). • Consider possible toxic ingestion • If patient is between one and sixteen years of age and is • Consider possible head injury – refer to Head Trauma protocol experiencing an exacerbation of his/her previously diagnosed (p. 64) prn asthma, see nebulized albuterol protocol. (p. 86) • Avoid unnecessarily agitating child. Transport with parent and I / CC / P • IV of NS at KVO allow parent to hold if possible. • Rapid transport. CC / P • Assess blood glucose and refer to Diabetic Emergencies protocol (p. 63), if hypoglycemia present. I / CC / P • IV will agitate child and should be deferred unless immediately necessary for medication administration or fluid challenge – refer to Fluid Challenge protocol (p. 48). ABSOLUTE ON-LINE MEDICAL CONTROL:
CC / P • If wheezing present, administer albuterol by nebulizer, dosage CC / P • If seizures continue, Lorazepam 0.1 mg/kg slow IV. May be as follows: repeated in 5-10 minutes, if seizures continue. – < 1 y/o: 1.25 mg • OR Diazepam 0.05-0.3 mg/kg IV/IO/ET, which may also be – > 1 y/o: 2.5 mg repeated q 15 min. May give under pressure with BVM, if necessary.
ON-LINE MEDICAL CONTROL ( standin g order if communication failure):
CC / P • Medical control may suggest epinephrine 1:1,000 at 0.01 mg/kg (up to 0.3 mg) IM or SQ as alternative to albuterol.
Revised 2002 -71- Revised 2002 -72- Special Protocols Initiation / Termination of Resuscitation
INITIATION OF RESUSCITATION
All providers, regardless of level of certification, are required to initiate cardiopulmonary resuscitation (CPR) in any victim who is apneic, pulseless, and/or demonstrating signs of inadequate perfusion, unless the criteria described below are a factor.
WITHHOLDING RESUSCITATION
Resuscitation should be withheld in the following circumstances: • Inter-facility transfer and sending facility has provided a written order not to resuscitate the patient. • When presented with a non-hospital DNR Order on the standard Department of Health form. • When the standard DNR bracelet is found on the patient’s body. • In cases of obvious death such as decapitation, or similarly mortal injuries, or where rigor mortis, tissue decomposition, or extreme lividity is present. • Frozen state. • Incineration. .
NOTE: A health care proxy, or a living will, is not sufficient for withholding or terminating CPR. Normal treatment protocols should be followed and the receiving hospital should be notified of the existence of the proxy or living will.
TERMINATION OF RESUSCITATION
Once CPR is initiated, it must be continued until one of the following occurs: • Effective spontaneous circulation has been restored, • Resuscitation efforts have been transferred to another appropriately trained individual who continues CPR and other Basic Support measures, • A physician assumes responsibility for the patient in an Emergency Department, or on-scene if the appropriate card has been signed (see p. 80). • Care of the patient is transferred to hospital staff assigned responsibilities for emergency care, • Valid non-hospital DNR is discovered. • The rescuer is exhausted and physically unable to continue resuscitation. • A medical control physician (on-scene, or by radio, telephone, or other means) orders the in-field termination of resuscitation, per the following procedure:
Revised 2002 -75- Termination of Resuscitation Procedure
STANDING ORDERS:
CRITERIA
Patients must meet all of the following requirements for in-field termination of resuscitation: • Adult (>18 y/o) patient who is non-traumatic, non-hypothermic, and does not have a reversible cause of arrest. • ECG is asystolic, or has a pulseless idioventricular rhythm with a rate <10 beats per minute, • There has been no return of a perfusing cardiac rhythm at any time during the resuscitation, • Patient’s cardiac arrest did not occur in a public place, • Full ACLS guidelines have been followed for at least 25 minutes, including successful intubation, IV access, adequate CPR, and appropriate pharmacologic therapy. • Issues of family notification have been addressed with medical control or other appropriate individuals, such as law enforcement.
PROCEDURE
• Follow ACLS guidelines for at least 25 minutes. • Assure all the above criteria have been met. • Obtain on-line authorization from Medical Control to terminate resuscitative efforts. • Request Law Enforcement Officer/Coroner to scene.
Transport to the hospital should be initiated if any of the above criteria are not met, or if the family or the patient’s private physician (if contacted) disagree with the termination of efforts at the scene.
Revised 2002 -76- On-scene Helicopter Utilization Guidelines Mass Casualty Incident (MCI) ALS Policies
A mass casualty incident is any situation that requires more service or services than STANDING ORDERS: may be immediately available. When faced with an MCI, coordination of efforts becomes vital. Several different circumstances may exist at an MCI or disaster that Air Medical Services should be considered for the following: will tax the skills of the advanced technicians. For this reason, several parameters 1) Patients who meet the vital signs or injury criteria for trauma care when have been set to augment the activities of the technicians. Those areas not covered ground transport time is greater than 20 minutes to a trauma center. are assumed to be handled per the protocols within this document without deviation. 2) A multiple casualty incident 3) A remote / wilderness area, difficult terrain, or any other time when a ground ORDER OF RESPONSIBILITY: ambulance is unable to access the patient in a reasonable time frame. 4) Any unstable patient when ground transport to the nearest hospital is greater The highest-level AEMT of the first-toned agency on the scene becomes the than 20 minutes ALS/Scene Coordinator and will coordinate the activities of all other EMS personnel arriving at the scene. He / she is also responsible for maintaining accurate records of A request for Air Medical Service standby or flight should be made by on-scene these activities. Technicians should be familiar with their County’s MCI plan and emergency services personnel. adhere to those principals.
POLICIES TO BE IN EFFECT DURING AN MCI/DISASTER ONLY:
1) Patients requiring cardiac monitoring, IV fluid, or the administration of Air medical service en route can only be canceled medications will be treated per the Finger Lakes ALS protocols unless otherwise by the highest level currently certified EMT on stipulated here. 2) If a patient is being administered IV fluids without medications, that patient may scene. be transported by a BLS crew 3) A medical control physician may authorize, however, a patient who has been administered medication to be transported with a Basic EMT in attendance along with a list of medications and dosages given Patient transport should NOT be delayed 4) An AEMT, when treating more than one patient, should treat those patients in close proximity to each other so that he may monitor each patient. Patients awaiting a helicopter. Begin transport and should be brought to a holding or staging area where they may receive treatment 5) Whenever possible, the ALS/Scene Coordinator should be an EMT-CC or rendezvous with the helicopter en route whenever EMT-P. possible.
Revised 2002 -77- Revised 2002 -78- Medical Control
A Medical Control Base Station provides on-line medical control and serves as a resource to EMT’s engaged in treatment activities. To receive medical control, the EMT must ask to speak to the emergency physician. Ideally, medical control should be obtained from the facility that will receive the patient. In cases where the receiving hospital is elsewhere, the medical control physician should attempt to communicate patient care information to the receiving hospital. When on-line medical control is not needed, the EMT still must notify the receiving facility as soon as possible of the patient’s condition and their time of arrival. For on-line medical control, cellular phones should be utilized whenever possible. UHF biotelemetry radio is an alternative. The following hospitals are recognized by FLREMSC as Medical Control Base Stations. HOSPITAL DISP 1° FREQ TELEPHONE CODE VHF Arnot-Ogden 071 155.340 ED 607-737-4194 Auburn Memorial 053 155.355† ED 315-255-7011 Cayuga Med. Ctr. 541 155.340* ED 607-274-4411 ED 607-274-4514 Clifton Springs 341 155.340 ED 315-462-1451 CP 315-462-7816 FF Thompson 342 155.175 ED 585-396-6600 CP 585-394-3511 Geneva General 343 155.340 ED 315-787-4500 CP 315-789-4795 Highland 272 155.340 ED 585-461-6880 ViaHealth of Wayne 583 155.340 ED 315-483-7524 Myers Campus or 6939 CP 315-483-8902 ViaHealth of Wayne 584 155.340 ED 315-332-2267 Newark-Wayne Campus 315-332-1957 Noyes Memorial 251 155.340 ED 585-335-6001 Park Ridge 275 155.340 ED 585-723-7070 Rochester General 276 155.340 ED 585-338-2300 MC 585-338-3367 Schuyler County 481 155.400 ED 607-535-7121 155.340 (x222 or 279) Soldiers & Sailors 612 155.340 Main 315-531-2000 Strong Memorial 278 155.340 ED 585-275-4551 MC 585-271-2769 Upstate (Univ.) 336 155.340* ED 315-464-5700 * must call fire control † do not need to use tones CP = radio/phone line MC= medical control
Revised 2002 -79- On-Scene Medical Personnel
In the event that a physician, registered nurse, or physician's assistant comes to the scene and wants to assist, the following procedure(s) should be utilized:
Physician 1. The EMT should present the information card shown below to the physician:
Finger Lakes Regional Emergency Medical Services Council, Inc. (FLREMSC) ON-SCENE PHYSICIAN INFORMATION
Thank you for your offer of assistance. Please be advised that we are certified by the NYS Department of Health and are working under Medical Control from physicians at a Resource Hospital. We are not permitted to relinquish Medical Control to a physician on the scene without approval from Medical Control at the Resource Hospital.
You may assist the EMS provider, but if you wish to take charge of this patient’s medical care, you must: 1. Be currently licensed in New York State as a physician 2. Request to speak with the Resource Hospital physician 3. Assume all responsibility for this patient 4. Accompany this patient to the hospital 5. Document your interventions and orders on the PCR 6. I agree to the above stipulations _____ (initials)
per Frank Edwards, MD, Chair, Finger Lakes Regional Emergency Medical Advisory Committee
2. The on-scene physician should be put in touch with a Medical Control Base Station by radio (or telephone, if appropriate) to consult with the Medical Control physician. If communications with a Medical Control cannot be accomplished, then the EMT is to adhere to these protocols and take NO medical orders from the on-scene physician. 3. The Medical Control physician may: • Refuse to release the patient, in which case the EMT will proceed as per usual under the direction of the Medical Control. • Release the patient to the on-scene physician. If so, the on-scene physician must: • Produce his / her valid NYS Certificate of practice medicine. • Write orders for the EMT (only to the level at which the EMT is trained). • Sign for his actions on the patient management form. • Accompany the patient to the hospital. • In the event that a physician gives an order which is contrary to these protocols, or the EMT's training, or which clearly and certainly, in the opinion of the EMT, will be detrimental to the patient's care, the EMT must respectfully question the order, then decline the order. • If the on-scene physician initials the information card, it should be attached to the agency copy of the PCR. Non-physician medical personnel may assist with patient care under the direction of the ALS technician, but may not be in charge of, or assume responsibility for, patient care. Patient Refusals / AMA Revised 2002 -80-
ALL • Always talk with patient and attempt to convince him / her of the need for treatment / transport • Talk with family and friends in an attempt to convince patient of the need for treatment / transport • Offer to call Medical Control and have patient speak with physician • If patient still refuses treatment / transport: – Assess LOC: • Patient is alert and oriented x3 with GCS = 15 – Rule out the following conditions: • Attempted / threatened suicide • Minor refusing care • Parent refusing when potentially serious illness or child abuse exists – NO – if none of the above apply, patient can refuse treatment / transport • Educate patient and family • Have patient sign AMA on PCR – YES – if the above apply, contact medical control. Elicit assistance from law enforcement agency, if necessary. • Patient not alert, not oriented, GCS < 15 – Patient cannot refuse transport – Contact medical control – Elicit assistance from law enforcement agency, if necessary
• Under no circumstances should field personnel allow themselves to be placed in danger. If this potential exists, go to a safe area and call for assistance.
Revised 2002 -81- Phone / Radio Failure
STANDING ORDERS :
ALL
Situations may occur where communications with medical control cannot be established due to one or more of the following reasons:
• The crew is not within UHF / cellular range due to distance from radio tower, terrain, or radio dead spots • The crew is not within their home cellular service area • The radio or cellphone is malfunctioning, making communications impossible • No telephones are available at the scene • No physician is available at the Medical Control Base Station
In the event of this situation, all protocols listed in this document become standing orders for use by the EMT-I, CC, or P as appropriate WITH THE EXCEPTION OF ORDERS IDENTIFIED AS “ABSOLUTE ON-LINE MEDICAL CONTROL.”
Orders identified as “absolute on-line medical control” in this document are ABSOLUTE ON-LINE PROCEDURES and may only be done by direct verbal order from a base station physician. They may not be done by protocol or standing orders.
Absolute on-line procedures are summarized below:
1. Administration of the following medications: Calcium gluconate Dopamine Morphine sulfate Epinephrine drip Sodium bicarbonate Diltiazem Flumazenil Verapamil
2. Induction of vomiting with ipecac syrup and / or administration of activated charcoal
In the event that a protocol work-up is performed, thorough documentation is required describing the type of communication problem which occurred, the number of attempts made and base stations attempted. The ALS Chief of the provider service is responsible for submitting the run record from the work-up to the system QA coordinator for review.
Revised 2002 -82- Transportation Destination Policy Statement
This policy should serve as a guideline for use by EMT’s in determining the receiving facility for their patient(s). In order of importance, the following elements should be taken into consideration.
1. Whenever appropriate, patients should be transported to the facility of their choice. In the case of the incompetent patient, the family’s choice should be respected. This applies only to STABLE patients whose condition does NOT REQUIRE a specific destination (i.e. New York State Trauma Protocols).
2. Decisions to transport the patient to another facility should (in order of importance) be based on:
a. The urgent clinical need of the patient to be seen immediately by a physician in the nearest emergency department (i.e. CODES, unmaintainable airway, etc.).
b. Protocol-specific destination for patients with certain conditions (i.e. trauma center for patients with specific types of trauma).
c. The decision of an EMT-CC or EMT-P, in conjunction with direct on-line medical control, that transport to another facility is more appropriate to the patient's treatment plan .
It is the intent of the Finger Lakes Regional Emergency Medical Services Council to endorse the action of any EMT based on the above guidelines.
Revised 2002 -83- Universal Precautions
Universal precautions should be used for all patient contacts if the health care provider may be exposed to blood and certain other body fluids that appear to be contaminated with blood. Universal precautions assume that all patients are carriers of infectious, contagious diseases.
General Recommendations
• Gloves should be worn when handling blood, body fluids, mucous membranes, non-intact skin, and body tissues. New gloves should be worn for each patient contact. Hands must be washed after glove removal and between patient contacts.
• If a splash of blood or body fluid is possible, a full face shield or goggles and face mask should be used.
• If emergency ventilatory support is necessary, a resuscitation mask should be used.
• Do not recap needles. Promptly place disposable sharps in a designated puncture-resistant container.
• Place all soiled linen in a clear, plastic bag before sending it to the laundry.
• Use a solution of 1 part household bleach to 10 parts water to clean equipment, clean up spills, and decontaminate walls and other objects soiled with blood and body fluids.
• If your skin has a break, cut, abrasion, or dermatitis, use gloves and avoid contact with blood and body fluids.
• Be vaccinated against Hepatitis B
Since there is no reliable, immediate means to identify infected patients, it is recommended that prehospital care providers be equally cautious when caring for ALL patients.
Revised 2002 -84- Epinephrine Auto-Injector Administration by EMT-D/I
Anaphylaxis can be a potentially life-threatening situation most often associated with a history of exposure to an inciting agent/allergen (bee sting or other insect venom, medication/drugs, or foods such as peanuts, seafood, etc.) and physical reactions ranging from mild skin rashes to catastrophic multi-system failure and/or death. The presence of respiratory distress (upper airway obstruction, lower airway disease/severe bronchospasm) and/or cardiovascular collapse/hypotensive shock characterize the clinical findings that authorize and require treatment according to this protocol.
• Request advanced life support intercept. DO NOT delay transport to the hospital. • Determine that the patient’s history includes a history of anaphylaxis, severe allergic reactions, and/or recent exposure to an allergen or inciting agent. • Administer high concentration oxygen • Assess the cardiac and respiratory status of the patient. • If both the cardiac and respiratory status of the patient are normal, transport the patient, reassessing the patient’s condition frequently during the transport. • If either the cardiac or respiratory status of the patient is abnormal, proceed as follows: • If the patient is having severe respiratory distress or shock and has been prescribed an epinephrine auto-injector, assist the patient in administering the epinephrine. If the patient’s auto-injector is not available or is expired, and the EMS agency carries an epinephrine auto-injector, administer the epinephrine as authorized by the agency’s medical director. • If the patient has not been prescribed an epinephrine auto-injector or has already received a dose and is still having symptoms, begin transport and contact Medical Control for authorization to administer epinephrine or an additional dose of epinephrine, if available. • Refer immediately to the appropriate Respiratory Arrest, Respiratory Distress, Obstructed Airway, or Shock protocol. • If cardiac arrest occurs, perform CPR according to AHA/ARC standards. • Contact Medical Control for Age<5 years. • Record all patient care information, including the patient’s medical history and all treatment, provided on a Prehospital Care Report (PCR).
Revised 2002 -85- Nebulized Albuterol (for Exacerbation of Previously Diagnosed Asthma)
EMT-D / I
For patients between one (1) and sixty-five (65) years of age, who are experiencing an exacerbation of their previously diagnosed asthma:
• Assess the airway. • Administer oxygen. • Monitor breathing.
NOTE: If patient exhibits signs of imminent respiratory failure, refer to Adult Respiratory Distress/Failure protocol or Pediatric Respiratory Distress/Failure protocol (as applicable).
• Do not permit physical activity. • Place the patient in a Fowler’s or Semi-Fowler’s position. • Assess the following prior to administration of the first nebulized treatment: • Vital signs • Patient’s ability to speak in complete sentences • Accessory muscle use • Wheezing • Patient self-assessment of severity (BORG scale)* NOTE: For patients with a history of angina, myocardial infarction, arrhythmia, or congestive heart failure, Medical Control MUST be contacted prior to initiating next step.
• Administer Albuterol Sulfate 0.083%, one (1) unit dose (3 ml) via nebulizer at a flow rate that will deliver the solution in 5 to 15 minutes. Do not delay transport to complete medication administration. • Begin transport.
NOTE: For patients in significant respiratory distress, call for Advanced Life Support (ALS) assistance. Do not delay transport. Plan an ALS intercept and/or initiate rapid transport to the nearest hospital if necessary.
• Upon completion of medication administration, reassess the patient. If patient is in severe respiratory distress, a second dose may be administered during transport. Transfer patient care to an ALS Provider or a receiving hospital.
NOTE: Medical Control must be contacted for any patient refusing medical assistance or transport.
*Ask patient to rate severity of difficulty breathing from 1 – 10, 10 being highest.
Revised 2002 -86- Surgical Airway
Although paramedics may perform needle cricothyroidotomy with jet insufflation under absolute on-line medical control as a last-ditch airway control measure, the creation by paramedics of an open cricothyroidotomy (intubation of the trachea through the cricothyroid membrane by other than a needle technique) is not yet covered by a routine protocol in the Finger Lakes EMS region. Paramedic level corps who desire to perform open cricothyroidotomies must submit a special application for evaluation and approval by the Finger Lakes REMAC.
This application should contain a detailed protocol, along with evidence of sufficient training for each member of the corps who would be performing the technique. The application would require approval and active involvement of the service medical director, and would need to contain evidence of a comprehensive quality assurance and refresher training program. It would be an absolute on-line medical control procedure.
Revised 2002 -87- FORMULARY
Medication Trade Name Page(s) Activated charcoal none 82 Adenosine Adenocard 21, 22, 44, 60 Albuterol Proventil, Ventolin vi, 11, 25, 36, 44, 53, 71, 86 Amiodarone Cordarone 17, 22, 44, 57 Atropine same 15, 18, 19, 44, 59 Calcium gluconate none 38, 82
D25 same 51, 63
D50 same 9, 26, 37 Diazepam Valium 12, 19, 21, 22, 27, 28, 37, 44, 72 Diltiazem Cardizem 21, 82 Diphenhydramine Benadryl 11, 12, 44, 53 Dopamine Intropin 19, 25, 31, 44, 66, 82 Epinephrine Adrenalin vi, 11, 15, 17, 18, 19, 36, 44, 53, 56, 57, 58, 59, 69, 71, 82, 85 Etomidate Amidate 28 Flumazenil Romazicon 19, 22, 82 Furosemide Lasix 25 Glucagon none 9, 26, 44, 51, 63 Glucose gel none 26, 63 Haloperidol Haldol 12 Ipecac same 35, 44, 70, 82 Ipratropium Atrovent 36 Lidocaine Xylocaine 17, 20, 22, 27, 28, 44, 57, 61 Lorazepam Ativan 12, 19, 21, 22, 27, 28, 37, 44, 72 Magnesium sulfate same 17, 38 Morphine sulfate none 10, 19, 21, 22, 23, 25, 44, 52, 82 Nalbuphine Nubain 10, 23, 25 Naloxone Narcan 9, 10, 19, 21, 22, 23, 25, 35, 44, 51, 52 Nitroglycerin (NTG) Nitrostat, Tridi, Nitro- 23, 25 paste Normal saline (NS) none 4, 8, 11, 13, 14, 26, 27, 28, 29, 30, 32, 34, 37, 38, 44, 47, 48, 50, 53, 54, 55, 56, 57, 58, 61, 64, 65, 70, 72 Procainamide Pronestyl 17 Promethazine Phenergan 23, 29 Sodium bicarbonate none 15, 17, 18, 44, 56, 57, 82 Sorbitol-free activated same 39, 70 charcoal Succinylcholine Anectine 28 Thiamine Betalin 9 Vasopressin Pitressin 17 Verapamil Isoptin, Calan 21, 82
Revised 2002 -89-