Indicators for monitoring progress towards maternal and newborn survival
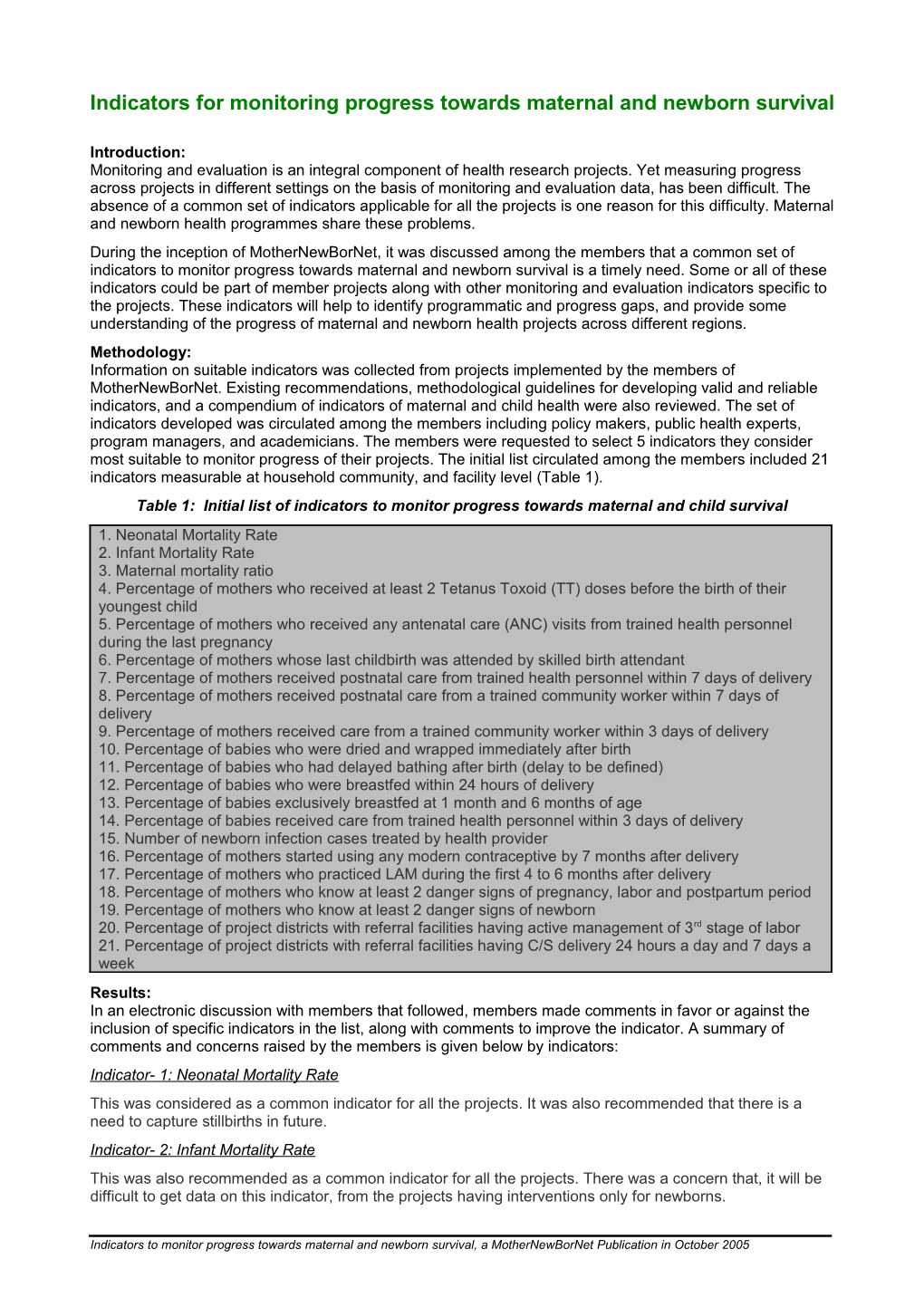
Introduction: Monitoring and evaluation is an integral component of health research projects. Yet measuring progress across projects in different settings on the basis of monitoring and evaluation data, has been difficult. The absence of a common set of indicators applicable for all the projects is one reason for this difficulty. Maternal and newborn health programmes share these problems. During the inception of MotherNewBorNet, it was discussed among the members that a common set of indicators to monitor progress towards maternal and newborn survival is a timely need. Some or all of these indicators could be part of member projects along with other monitoring and evaluation indicators specific to the projects. These indicators will help to identify programmatic and progress gaps, and provide some understanding of the progress of maternal and newborn health projects across different regions. Methodology: Information on suitable indicators was collected from projects implemented by the members of MotherNewBorNet. Existing recommendations, methodological guidelines for developing valid and reliable indicators, and a compendium of indicators of maternal and child health were also reviewed. The set of indicators developed was circulated among the members including policy makers, public health experts, program managers, and academicians. The members were requested to select 5 indicators they consider most suitable to monitor progress of their projects. The initial list circulated among the members included 21 indicators measurable at household community, and facility level (Table 1). Table 1: Initial list of indicators to monitor progress towards maternal and child survival 1. Neonatal Mortality Rate 2. Infant Mortality Rate 3. Maternal mortality ratio 4. Percentage of mothers who received at least 2 Tetanus Toxoid (TT) doses before the birth of their youngest child 5. Percentage of mothers who received any antenatal care (ANC) visits from trained health personnel during the last pregnancy 6. Percentage of mothers whose last childbirth was attended by skilled birth attendant 7. Percentage of mothers received postnatal care from trained health personnel within 7 days of delivery 8. Percentage of mothers received postnatal care from a trained community worker within 7 days of delivery 9. Percentage of mothers received care from a trained community worker within 3 days of delivery 10. Percentage of babies who were dried and wrapped immediately after birth 11. Percentage of babies who had delayed bathing after birth (delay to be defined) 12. Percentage of babies who were breastfed within 24 hours of delivery 13. Percentage of babies exclusively breastfed at 1 month and 6 months of age 14. Percentage of babies received care from trained health personnel within 3 days of delivery 15. Number of newborn infection cases treated by health provider 16. Percentage of mothers started using any modern contraceptive by 7 months after delivery 17. Percentage of mothers who practiced LAM during the first 4 to 6 months after delivery 18. Percentage of mothers who know at least 2 danger signs of pregnancy, labor and postpartum period 19. Percentage of mothers who know at least 2 danger signs of newborn 20. Percentage of project districts with referral facilities having active management of 3rd stage of labor 21. Percentage of project districts with referral facilities having C/S delivery 24 hours a day and 7 days a week Results: In an electronic discussion with members that followed, members made comments in favor or against the inclusion of specific indicators in the list, along with comments to improve the indicator. A summary of comments and concerns raised by the members is given below by indicators: Indicator- 1: Neonatal Mortality Rate This was considered as a common indicator for all the projects. It was also recommended that there is a need to capture stillbirths in future. Indicator- 2: Infant Mortality Rate This was also recommended as a common indicator for all the projects. There was a concern that, it will be difficult to get data on this indicator, from the projects having interventions only for newborns.
Indicators to monitor progress towards maternal and newborn survival, a MotherNewBorNet Publication in October 2005 Indicator-3: Maternal mortality ratio Maternal mortality is a very rare event in each setting, and population size is often too small to calculate the maternal mortality ratio. It was recommended that projects can collect data over the years on numbers of maternal deaths and could carry out verbal autopsies, which might provide useful programmatic information. Indicator-4: Percentage of mothers who received at least 2 TT doses before the birth of their youngest child It is difficult to interpret what numbers of TT doses mean, as some programs are mature and women have sufficient TT injections even prior to her last pregnancy. For example, if a woman does not have 2 TT shots in her last pregnancy, she may already be protected with 5 or more shots. There are also differences in strategies such as providing TT to women 15-49 vs. pregnant woman only and card verified TT doses vs. self-reported TT doses. Indicator-5: Percentage of mothers who received any ANC visits from trained health personnel during the last pregnancy There was no consensus on the cut off point for number of ANC visits. WHO recommended ANC indicator is 4 visits although the WHO Africa Bureau uses ANC 3 visits since 4 is too ambitious for them. ANC with 2 visits is probably too low given that the global ANC 2 visits coverage is already high (about 70%). Other relevant indicators were suggested on birth and newborn preparedness (e.g. percentage of deliveries conducted by using clean delivery materials; percentage of households with money for emergency care for mothers or newborns; percentage of households that have arranged transport for travel when emergency care for mother or newborn is needed). It was felt that an operational definition of trained health personnel applicable for all countries is needed. Indicator-6: Percentage of mothers whose last childbirth was attended by skilled birth attendant This was accepted as an important indicator, but an operational definition of skilled birth attendant was felt necessary. Indicator-7: Percentage of mothers received postnatal care from trained health personnel within 7 days of delivery ; Indicator-8: Percentage of mothers received postnatal care from a trained community worker within 7 days of delivery ; Indicator-9: Percentage of mothers received care from a trained community worker within 3 days of delivery It was felt that 7 days is too long, and clarification was sought whether postnatal referred to mother or baby or both. It was revealed that postpartum care within 3 days can be feasible in some projects. It was also suggested to phrase the indicator as ‘ postpartum care for mother and newborn by a trained health care provider’ and include all levels of health care personnel from community health worker (CHW) to facility based worker among trained health care provider. It was recommended that there is no reason to distinguish among levels of workers (trained health personnel and trained community worker) until the rate of PNC increases. It was also felt that there is a need to define what postpartum care in the community means. Examples from Measure-Evaluation document was cited. Measure-Evaluation document listed all indicators in the initial list (Table-1) except postpartum care within 3 days by trained health care worker (HCW) and newborn care within 3 days by trained HCW. Indicator-10: Percentage of babies who were dried and wrapped immediately after birth It was opined that this indicator is too vague. The word ‘wrapped’ has different meanings for example a baby can be wrapped against mother or wrapped in a blanket. It was suggested that delayed bathing for at least 6 hours can be used as a proxy because this indicator can be measured. Different ways of measuring drying and wrapping were tried in several countries but were not successful. There were a lot of unclear questions, exceptions and difficulty to apply. Examples from Measure-Evaluation document was again cited. Measure-Evaluation document have defined thermal protection with three criteria: (a) delayed bathing for at least 6 hours, (b) covering the head, and (c) drying and wrapping immediately after birth. It was suggested that the most important thing is drying and covering the baby to prevent heat loss. The modified indicator recommended was ‘percentage of babies dried and wrapped in dry sheet immediately after birth’. Indicator-11: Percentage of babies who had delayed bathing after birth It was discussed that there were two components involved in this indicator (a) delaying the bath at birth and (b) the duration of the delay. Delaying the birth: It was revealed that there is lack of evidence that delay in bathing improves newborn health especially when the babies are normal weight and full term. A cold-water bath is unanimously not good but there are studies showing that a warm water bath may not be harmful. Bathing is needed if a baby is born to an HIV positive mother and if there is excessive blood, maternal stools, and frank infected liquor.
Indicators to monitor progress towards maternal and newborn survival, a MotherNewBorNet Publication in October 2005 There are potential benefits of antiseptic ‘baths’ or sponging in poor hygienic condition. There is a paucity of evidence about the benefits or harmful effects of just wiping the baby or actually using wet swabs or sponge. It is not always helpful to assume that families will use cold water and therefore suggest, ‘do not bathe. Babies who get wet by sponging can also get hypothermic if not properly attended. Moreover, bathing has various connotations– cold vs. warm water bathing, cleaning vs. scrubbing, sponging vs. bathing etc. Duration of bathing delay: Among the programmes, the periods of delay in bathing vary from 6 hours to overnight to 24 hours and even longer. It was opined that the main issue is ‘maintenance of the baby's body temperature in the ideal temperature range at all times’. It is necessary for health care workers and mothers to realize that they will have to keep babies pleasantly warm without getting chilled or overheated and verify that the baby is maintaining his/her temperature all the time. But it is impossible to translate this whole process into a simple understandable, doable term that can be readily understood and evaluated by all health workers and family members. Concern was raised that use of ‘percentage of babies who had delayed bathing for at least 24 hours’ as a core indicator, will leave other relevant issues unaddressed. Findings from formative research in Pakistan showed that in rural settings a majority of deliveries are conducted at home. Immediately after birth, the newborn is placed on cold mud floor without drying and wrapping. This is because the attending TBA is busy delivering the placenta. If a relative is present, the baby is handed over to her. She takes the baby and gives a bath considering vernix to be dirty. During the bath she rubs skin of the baby rather aggressively to take off blood and vernix. As a result the baby is not put to mother’s breast immediately after delivery. A mixture of several such behaviors may lead to hypothermia. It was opined that programs should be encouraged to identify behaviors that may lead to hypothermia in a particular setting. An indicator should not focus on one particular behavior. As far as maintaining the right temperature according to the season is the main goal, these particular behaviors should be linked with drying the baby after delivery, warming and wrapping the baby and putting it closer to mother’s breast. If families delay bathing beyond 24 hours, but do not dry and wrap the newborn immediately and properly damage is done. From the perspective of thermal control, immediate drying and wrapping (again before even the cord is cut) should be a focus of the program. Considering the fact that hypothermia may vary among different settings and cultures and the need to focus on a positive action that the birth attendant or family can practice universally, this was regarded as an important proxy indicator. It was also suggested that delay needed to be defined. Two cut offs for delay were recommended: a. more than 6 hours and b. more than 24 hours. Indicator-12: Percentage of babies who were breastfed within 24 hours of delivery There was no consensus on the timing of initiation of breastfeeding. Breastfeeding within 1 hour, 3 hours, and 24 hours was discussed. It was also discussed that initiation of breastfeeding within 1 hour will be difficult for mothers who had caesarian section delivery. It was also suggested that colostrum feeding should be included along with breastfeeding within 1 hour. Moreover, initiation of breastfeeding ‘immediately’, especially before the delivery of placenta would be more important. Indicator-13a: Percentage of babies exclusively breastfed at 1 month Indicator 13b: Percentage of babies exclusively breastfed at 6 month It was revealed that Demographic and health Survey (DHS) indicator is ‘breastfeeding exclusively at 4 months’. Analusis done by DHS is normally on the basis of small sub-samples, not really big enough for significant results. If this indicator is included, data on exclusive breastfeeding for initial 6 months of age should be taken. This indicator is not suitable for countries where HIV prevalence is high. For the purpose of monitoring newborn care at community level early and exclusive breastfeeding indicators are good core as well as tracer indicators in low HIV prevalence settings. Indicator-14: Percentage of babies received care from trained health personnel within 3 days of delivery This was regarded as an important indicator. There was some debate on 3 days vs. 7 days. It was suggested that newborn care within 3 days might be very restrictive and hard to achieve in newborn programs that are new. Postpartum care for newborns also needs to be further defined. Indicator-15: Number of newborn infection cases treated by health provider This was not regarded as a suitable indicator to be used by all maternal and newborn health projects. This indicator is useful only if the project aims to treat newborn infections. Also, there are a lot of newborn infections, and indicators for each of the newborn infections are necessary for this purpose. Indicator-16: Percentage of mothers started using any modern contraceptive by 7 months after delivery This was also regarded as an important indicator. Other related indicators suggested are: - Percentage of ANC or PP visits in which FP is counseled, delivered or referred - Percentage of couples who know 2 benefits of spacing pregnancies at least two years apart - Percentage of couples who know 2 benefits of limiting births for high parity/> 35 years women - Percentage of women using family planning (modern methods) six months postpartum
Indicators to monitor progress towards maternal and newborn survival, a MotherNewBorNet Publication in October 2005 - Percentage of women using contraception 6 months postpartum - Percentage of women using contraception 12 months postpartum - Percentage of women using contraception 6 weeks postpartum if not practicing LAM - Percentage of mothers who practiced LAM during the first 4 to 6 months postpartum Indicator-17: Percentage of mothers who practiced LAM during the first 4 to 6 months after delivery This indicator was considered as redundant, when compared with indicator 16. Indicator-18: Percentage of mothers who knows at least 2 danger signs of pregnancy, labor and postpartum period There was confusion in terms of 2 in each period i.e. 6 in total or 2 each - separated into 3 indicators. It was suggested that if they are all combined looking at women who knew at least 2 signs, usual term is knowledge of 'maternal danger signs.' Otherwise it is wise to split maternal danger signs for a. pregnancy, b. delivery and c. postpartum periods and split newborn danger signs for a. immediate and b. postnatal period. Indicator-19: Percentage of mothers who knows at least 2 danger signs of newborn It was regarded as an important knowledge level indicator considering the fact that some programme is yet to focus on danger signs of newborn. Indicator-20. Percentage of project districts with referral facilities having active management of 3rd stage of labor Indicator- 21: Percentage of project districts with referral facilities having C/S delivery 24 hours a day and 7 days a week These indicators were considered to be inapplicable for wide use as some projects may be confined in a small area within 1 district. Conclusion and recommendation After this debate and discussion, the following list of indicators were proposed for the maternal and newborn health projects (Table-2): Table 2: Recommended Indicators for community-based maternal and newborn programs Service Indicators: 1. Percentage of pregnant mothers who received antenatal care (at least three times) by a trained Health Care Worker (HCW)* during the last pregnancy 2. Percentage of mothers whose last childbirth was attended by a skilled birth attendant 3. Percentage of mothers who received tetanus toxoid vaccine in their last pregnancy 4. Percentage of mothers who received care within three days postpartum, by a trained HCW 5. Percentage of newborn who received care within three days after birth, by a trained HCW 6. Percentage of births in facilities that received active management of the third stage of labor to prevent postpartum hemorrhage Knowledge indicator: 7. Percentage of mothers who know at least two maternal danger signs 8. Percentage of mothers who know at least two newborn danger signs Behavior indicator: 9. Percentage of births with new or sterile blade or equipment for cutting the cord 10. Percentage of babies who were breastfed within 1 hour after delivery 11. Percentage of babies who had been dried and wrapped immediately after birth 12. Percentage of women using family planning (any modern methods) at six weeks postpartum 13. Percentage of caretakers seeking care from skilled care providers for sick newborns Impact indicator: 14. Neonatal mortality rate
* HCW includes skilled birth attendants and trained community health workers This article was developed through active participation of members of MotherNewBorNet. For further information, please contact: MotherNewborNet, Public Health Sciences Division, ICDDR,B, Mohakhali, Dhaka, Bangladesh http://www.icddrb.org/activity/?typeOfActivity=MotherNewB E-mail: [email protected]
MotherNewBorNet (Facilitating Translation of Research into Action) http://www.icddrb.org/activity/?typeOfActivity=MotherNewB
Indicators to monitor progress towards maternal and newborn survival, a MotherNewBorNet Publication in October 2005