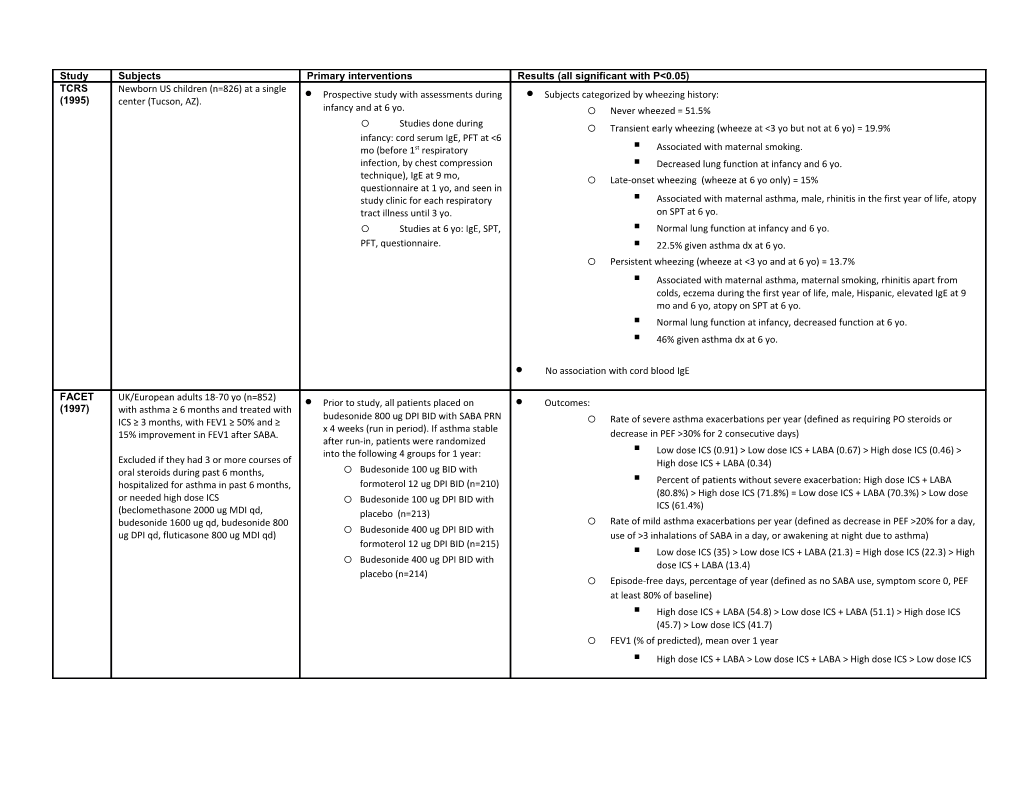
Study Subjects Primary interventions Results (all significant with P<0.05) TCRS Newborn US children (n=826) at a single Prospective study with assessments during Subjects categorized by wheezing history: (1995) center (Tucson, AZ). infancy and at 6 yo. o Never wheezed = 51.5% o Studies done during o Transient early wheezing (wheeze at <3 yo but not at 6 yo) = 19.9% infancy: cord serum IgE, PFT at <6 mo (before 1st respiratory . Associated with maternal smoking. infection, by chest compression . Decreased lung function at infancy and 6 yo. technique), IgE at 9 mo, o Late-onset wheezing (wheeze at 6 yo only) = 15% questionnaire at 1 yo, and seen in study clinic for each respiratory . Associated with maternal asthma, male, rhinitis in the first year of life, atopy tract illness until 3 yo. on SPT at 6 yo. o Studies at 6 yo: IgE, SPT, . Normal lung function at infancy and 6 yo. PFT, questionnaire. . 22.5% given asthma dx at 6 yo. o Persistent wheezing (wheeze at <3 yo and at 6 yo) = 13.7% . Associated with maternal asthma, maternal smoking, rhinitis apart from colds, eczema during the first year of life, male, Hispanic, elevated IgE at 9 mo and 6 yo, atopy on SPT at 6 yo. . Normal lung function at infancy, decreased function at 6 yo. . 46% given asthma dx at 6 yo.
No association with cord blood IgE
FACET UK/European adults 18-70 yo (n=852) Prior to study, all patients placed on Outcomes: (1997) with asthma ≥ 6 months and treated with budesonide 800 ug DPI BID with SABA PRN ICS ≥ 3 months, with FEV1 ≥ 50% and ≥ o Rate of severe asthma exacerbations per year (defined as requiring PO steroids or x 4 weeks (run in period). If asthma stable 15% improvement in FEV1 after SABA. decrease in PEF >30% for 2 consecutive days) after run-in, patients were randomized into the following 4 groups for 1 year: . Low dose ICS (0.91) > Low dose ICS + LABA (0.67) > High dose ICS (0.46) > Excluded if they had 3 or more courses of High dose ICS + LABA (0.34) oral steroids during past 6 months, o Budesonide 100 ug BID with hospitalized for asthma in past 6 months, formoterol 12 ug DPI BID (n=210) . Percent of patients without severe exacerbation: High dose ICS + LABA (80.8%) > High dose ICS (71.8%) = Low dose ICS + LABA (70.3%) > Low dose or needed high dose ICS Budesonide 100 ug DPI BID with o ICS (61.4%) (beclomethasone 2000 ug MDI qd, placebo (n=213) budesonide 1600 ug qd, budesonide 800 o Rate of mild asthma exacerbations per year (defined as decrease in PEF >20% for a day, Budesonide 400 ug DPI BID with ug DPI qd, fluticasone 800 ug MDI qd) o use of >3 inhalations of SABA in a day, or awakening at night due to asthma) formoterol 12 ug DPI BID (n=215) . Low dose ICS (35) > Low dose ICS + LABA (21.3) = High dose ICS (22.3) > High Budesonide 400 ug DPI BID with o dose ICS + LABA (13.4) placebo (n=214) o Episode-free days, percentage of year (defined as no SABA use, symptom score 0, PEF at least 80% of baseline) . High dose ICS + LABA (54.8) > Low dose ICS + LABA (51.1) > High dose ICS (45.7) > Low dose ICS (41.7) o FEV1 (% of predicted), mean over 1 year . High dose ICS + LABA > Low dose ICS + LABA > High dose ICS > Low dose ICS CAMP US children 5-12 yo (n=1024) with mild- Budesonide DPI 200 μg BID (n=311) vs. No difference between budesonide and placebo in: (2000) moderate asthma (defined by the nedocromil 8 mg BID (n=312) vs. placebo, presence of sx ≥2X/wk, or by use of a o FEV1 for 4.3 years (average). SABA ≥2X/wk, or the use of daily o likelihood to discontinue study meds medication for asthma), and PC20 ≤ 12.5 bone density, fractures, cataract mg/ml. Allowed albuterol prn, oral prednisone for o exacerbations, addition of o depression questionnaire beclomethasone dip. 168 μg BID for poor control (with replacement or adding more Budesonide group with: meds allowed if still poorly controlled), tapering off meds for remission. o decreased AHR (via methacholine challenge) o shorter height and height percentile (~1 cm and 4%) Placebo grouped received o lower daily sx score, more episode-free days beclomethasone or other asthma less albuterol use, less additional controller med use controller meds for 20% of study days. o o less prednisone use o increased likelihood to taper study meds o fewer urgent care visits, fewer hospitalizations vs. placebo
SMART US subjects ≥12 yo with asthma (as Salmeterol 42 μg MDI BID added to GlaxoSmithKline terminated the study early due to preliminary findings in AAs and difficulties in (2006) judged by study physician) and current medications (n=13,176) vs. enrollment (but predefined criteria for study termination were not met at the interim analysis). currently receiving prescription placebo (n=13,179) added to current asthma medication. medications, for ~6.5 months (28 weeks). Primary endpoint: occurrence of respiratory-related (includes asthma-related) deaths or respiratory- Excluded if ever used LABA, Contacted by phone Q4 weeks to assess related life-threatening experiences, defined as intubation and mechanical ventilation. pregnancy, significant systemic study endpoints. o No difference between salmeterol and placebo for total population. disease, or current use of beta- o AA/salmeterol subgroup with statistically significant relative risk (4) for primary blocker. endpoint vs. AA/placebo o No difference between phase 1 and phase 2 for total population. Multicenter (over 6000 sites). AA/salmeterol/no ICS subgroup with statistically significant RR (5.6) for primary Recruitment in 2 phases (~3 years o each): phase 1 via media advertising, endpoint vs. AA/placebo/ICS phase 2 directly by study investigators. Secondary endpoints: o Total pop/salmeterol with statistically significant RR for the following: combined Baseline ICS use by 47% overall (49% asthma-related death or life-threatening experience (1.7), respiratory-related death in Caucasians and 38% in African (2.1), asthma-related death (4.3) Americans). Data for asthma history o Caucasian subgroup with no difference between salmeterol and placebo. and current nocturnal symptoms indicate greater disease severity at o AA/salmeterol subgroup with statistically significant RR for the following: combined baseline in the AA subgroup vs. asthma-related death or life threatening experience (4.9), combined all-cause death or Caucasian. life-threatening experience (2.1). o By phase of trial: . Total pop/salmeterol with statistically significant RR (1.8) for combined asthma-related deaths or life-threatening experiences during phase 1; No difference in secondary endpoints during phase 2. o By baseline ICS use: . Total pop/salmeterol/no ICS with statistically significant RR (2.39) for combined asthma-related death or life-threatening experience. . Caucasian subgroup with no difference between ICS and no ICS. . AA/salmeterol/no ICS subgroup with statistically significant RR (10.4) for combined asthma-related death or life-threatening experience.
PACT US children 6-13 yo (n=285) with mild- Fluticasone 100 μg DPI BID (n=86) vs. Primary outcome: percent of asthma control days during study (defined as a day w/o albuterol, oral (2007) moderate persistent asthma (via “combination” fluticasone/salmeterol steroids, additional controller medication, day/night sx, unscheduled PCP/ER visits, hospitalizations, reported sx, SABA use, or peak flow <80% 100/50 μg DPI QAM + salmeterol 50 μg DPI school absence due to asthma) calculated), FEV1 ≥ 80%, PC20 ≤ 12.5 QHS (n=81) vs. montelukast 5 mg PO QHS mg/ml. o Fluticasone (64.2 %) = combination (59.6 %) > montelukast (52.5 %) (n=83), for 48 weeks (11 months).
Excluded if history of life threatening Secondary outcomes (change vs. baseline): asthma, >4 courses oral steroids or 2 hospitalizations in past year. o Change in FEV1: Fluticasone (+6.3 %) = combination (+3.6 %) > montelukast (-0.58 %) o Decrease in eNO: Fluticasone (-59.1 %) > combination (-22.9 %) > montelukast (-18.9 %) o AHR via methacholine challenge: Fluticasone > combination = montelukast o Proportion of subjects not requiring oral steroids during study: Fluticasone (~60%) = combination (~48%) > montelukast (~42%) o Growth: no difference between treatments
LOCSS US patients ≥6 yo (n=500) with asthma 6 week run-in period with fluticasone 100 Primary outcome: (2007) was acceptably controlled after 4 to 6 μg DPI BID (run-in period). If asthma weeks of open-label treatment with o Time to treatment failure, defined as: ER/hospital vist, need for systemic corticosteroids stable, randomized to following groups: fluticasone propionate (Flovent Diskus, or open-label ICS use, fall in pre-SABA FEV1 to more than 20% below baseline value; continue fluticasone 100 μg DPI BID GlaxoSmithKline) decrease in AM PEFR >35% below baseline value on 2 consecutive days; use of ≥10 (n=169), fluticasone 100 μg + salmeterol puffs/day of SABA for 2 consecutive days (excluding exercise premed); refusal of the 50 μg DPI QHS (n=165), or montelukast 5- Inclusion criteria for enrollment in the patient to continue because of lack of satisfaction with treatment; or judgment by a 10 mg PO QHS (n=166) for 16 weeks. run-in period: age ≥6 yo, and FEV1≥60% physician that the patient should stop treatment for reasons of safety. predicted before SABA, and ≥12% . fluticasone (20.2%) = fluticasone + salmeterol (20.4%) > montelukast (30.3%) improvement in FEV1 post-SABA, or methacholine PC20 ≤8 mg. Secondary outcomes: Inclusion criteria after the run-in period: adequate adherence, a pre-SABA FEV1 ≥ o FEV1 %predicted (pre-SABA): 80% predicted, Asthma Control . fluticasone + salmeterol (91.8%) = fluticasone (91.1%) > montelukast (88.8%) Questionnaire score of <1.5 (0-6 scale, o Morning PEFR %predicted: lower is better); <16 puffs of SABA per week during final 2 weeks of the run-in . fluticasone + salmeterol (99%) > fluticasone (96.2%) = montelukast (94.7%) period (excluding exercise o Asthma symptom free days: premedication); no hospitalization, urgent medical care (for asthma), oral . fluticasone (85.8%) = fluticasone + salmeterol (82.7%) = montelukast (78.7%) corticosteroid use, or use of additional o Days with use of SABA asthma medication during the run-in . fluticasone (18.2%) = fluticasone + salmeterol (17.1%) = montelukast (22.9%) period; and an absence of febrile illness within the previous 24 hours. BADGE US children/teens 6-17 yo (n=165) with 48 week / 3 period (16 weeks each) Primary outcome: R mild-moderate asthma (as defined by crossover trial. During each 16 week (2010) NAEPP), FEV1 ≥ 60%, and FEV1 increase ≥ o Response to each of the 3 step-up therapies was judged on the basis of: period, subjects received the following 12% after SABA or PC20 ≤ 12.5 mg/ml. 2- step-up therapies: increase fluticasone to . Total amount oral steroids required 8 weeks prior to the treatment period, 250 μg DPI BID, or switch to their asthma was poorly controlled on . Asthma control days (during latter 12 weeks of each 16 week period). ACD fluticasone/salmeterol 100/50 μg DPI BID, fluticasone 100 μg DPI BID. defined as day with w/o albuterol, day/night sx, unscheduled visit to health or add montelukast 5-10 mg PO QD (to care provider, or peak flow <80% of best) fluticasone 100 μg DPI BID). . Change in FEV1 . A treatment considered to be better if needed at least 180 mg less oral Allowed albuterol prn, oral prednisone for steroids; if not, better if more asthma control days; if not, better if FEV1 exacerbations. improved at least 5%. If no difference in any parameter, treatments considered to be same. o 98% of patients had a differential response, with most responding to LABA step-up best. Probability of best response: add LABA > increase ICS = add LTRA. o Although LABA step-up most likely to provide the best response overall, some children had a best response to increased ICS or LTRA step-up.
Analysis of predictors of differential response: o Response affected by: . Asthma control test >19, more likely to have best response to LABA. . Race - Hispanic and whites most likely to have a best response to LABA, least to ICS. AA patients equally likely to have a best response to LABA or ICS and least to LTRA. . Eczema status – without eczema more likely to have best response to LABA. o Response not affected by: AHR (PC20 >1.5 vs <1.5 mg/mL), FeNO (>10 vs <10 ppb), 2 receptor genotype (Arg/Arg vs Arg/Gly vs Gly/Gly), age, sex, sensitization to perennial allergens, baseline FEV1 (>90% vs <90%), bronchodilator reversibility (>10% vs <10% FEV1), previous use or nonuse of a controller med, baseline number of asthma control days, and number of recent asthma exacerbations (0 vs ≥1).
TALC US adults ≥18 yo with asthma confirmed Prospective 3-way, double-blind, triple Primary end point: morning PEF (2010) by bronchodilator reversibility or BHR, crossover trial (n=210) FEV1 ≥ 40% of predicted value, and o tiotropium = salmeterol > double ICS nonsmoking status (<10 pack-years). Patients were treated for a 14-wk period with: Secondary end points: Enrolled in TALC study if after 4 week o Beclomethasone 80 μg HFA MDI BID + o Evening PEF run-in period with beclomethasone 80 μg tiotropium bromide DPI 18 μg QAM, or HFA MDI BID (all other asthma . tiotropium > salmeterol > double ICS medications stopped) patients with FEV1 o Beclomethasone 160 μg HFA MDI BID, o FEV1 (pre-bronchodilator) <70% predicted or if during final 2 weeks or of run-in period they had sx ≥6 days/wk o Beclomethasone 80 μg HFA MDI BID + . tiotropium > salmeterol = double ICS or used SABA ≥6 days/wk or were salmeterol 50 μg DPI BID o Asthma-control days (day without symptoms and without use of SABA) awakened by asthma ≥2 nights/wk. Between each 14 wk period, there was a 2 . tiotropium = salmeterol > double ICS wk washout period with beclomethasone o Asthma exacerbations with PO or IV steroids 80 μg HFA MDI BID. . double ICS (13) > tiotropium (7) > salmeterol (5) o Unscheduled visits for asthma symptoms . double ICS (6) > tiotropium (2) = salmeterol (2)
PEDIATRIC ASTHMA PREVENTION STUDIES Study Subjects Primary interventions Conclusions (all significant with P<0.5) ETAC UK children 1-2 yo with active AD for at Placebo (n=275) vs. cetirizine 0.25 mg/kg Primary end point: time to the onset of asthma (defined as 3 episodes separated by at least 7 days, either (2002) least 1 month. PO BID (n=274) for 18 month treatment of nocturnal cough with sleep disturbance lasting for at least 3 consecutive nights, wheezing, or a period, then observation for 18 months. combination of the 2) Excluded if wheezing episodes after 6 mo old, persistent nocturnal coughing, o No significant difference between placebo and cetirizine groups in probability of chronic pulmonary disease or other developing asthma after 36 mo. Median time to asthma onset was 27.1 mo for placebo During the study, choice of treatment for severe disorder likely to interfere with and 26.5 months for cetirizine. the study drug or observation of any conditions manifested by the children was left to the clinical . Analysis of subgroups with elevated grass pollen sIgE (>0.35): elevated outcome, regular antihistamine use, oral GP/placebo >> others cromoglycate use, or systemic steroids in investigators/other physicians managing the previous few weeks before the children. . Analysis of subgroups with elevated dust mite sIgE (>0.35): elevated recruitment. DM/placebo > elevated DM/cetirizine > negative DM/cetirizine > negative DM/placebo . Increased relative risk for developing asthma associated with elevated IgE to egg (RR 1.4), grass pollen (1.7), DM (1.6), cat dander (1.5), but not milk (1.1)
No difference in eczema improvement between groups. Overall trend toward improvement in eczema during the course of study in all treatment groups with all patterns of sensitivity.
No significant difference between groups in adverse effects, including EKG (RR, QT).
PAT European children 6-14 yo with AR to Subcutaneous IT to birch and/or grass Development of asthma defined as recurrence of ≥2 out of 3 sx (cough, wheeze, SOB) within the previous (2002) birch and/or grass (with positive SPT ≥3 (maintenance doses: 12 μg Bet v 1, 20 μg 12 mo, with sx that are not triggered only by infections and clinically respond to SABA; not dependent on mm and conjunctival challenge). Phl p 5, started before allergy season) the amount of reversibility with SABA. (n=79) vs. no immunotherapy (n=72), for Excluded if positive SPT to any allergen 3 years, then observed for 2 years. other than grass and/or birch, previous After 3 years: SCIT treatment, or asthma with need of o 24% developed asthma in IT group, 44% in controls. 5/6 centers concordant with similar Both groups were allowed to take daily medication. Study performed at 6 results. centers. symptomatic medication, limited to loratadine, nasal levocabastine o AHR incrementally decreased each year in IT group, no change in controls. (antihistamine), ocular sodium o IT group with improved symptom scores for conjunctivitis after 1st year and rhinitis after cromoglycate, and nasal budesonide. In 2nd year vs. control. case of asthmatic symptoms, SABA and ICS could be given. After 5 years (3 years IT + 2 years observation): Methacholine challenge done before o 20% with asthma in IT group, 76% in controls (4 subjects lost to follow-up in each allergy season (baseline), during season, group). and each winter for 3 years, and again at 5 years. o No significant difference in AHR between groups. AHR decreased in both groups vs. baseline. o IT group with stable improved symptom scores for conjunctivitis and rhinitis vs. control, (similar to scores after 1st 3 years).
PEAK US children 2.4-3.6 yo (n=285) with Fluticasone 88 μg BID via At end of 2 year treatment period: (2006) positive asthma predictive index aerochamber/mask (n=143) vs. placebo (frequent wheezing with one of the o Fluticasone group with (n=142) for 2 years, then observation off following: AD, AR, parent with asthma; study medication for 1 year. . more symptom free days (93% of treatment period v. 88%) OR 2 of the following: food allergy, wheezing unrelated to colds, . less prednisolone use for exacerbations eosinophilia). Allowed albuterol prn, oral prednisolone . less singulair or additional fluticasone added for poor control for exacerbations, additional controller . longer time to 2nd course of prednisolone or addition of controller med meds for poor control (e.g. more fluiticasone, montelukast). . decreased airway resistance measured via impulse oscillometry . shorter height (-1.1 cm), with slower growth velocity during 1st year Additional controller meds used in 13% (fluticasone) and 21% (montelukast) of o No difference between groups in placebo group during 2 year treatment period. . albuterol use . time to 1st prednisolone course . unscheduled physician visits and hospitalizations . growth velocity during 2nd year
At end of 3rd year (2 year treatment + 1 year observation period): o Fluticasone group with . less additional fluticasone added for poor control (only during 1st 3 months of observation period) . shorter height (-0.7 cm) at end of 3rd year, with increased “catch-up” growth velocity during 3rd year
o No difference between groups in . symptom-free days . albuterol, montelukast, prednisolone use . unscheduled physician visits and hospitalizations . airway resistance via impulse oscillometry o Children with a positive response to fluticasone treatment were more likely (OR 2.32) to have increase in symptoms during observation period.