Appendix I- Search criteria used
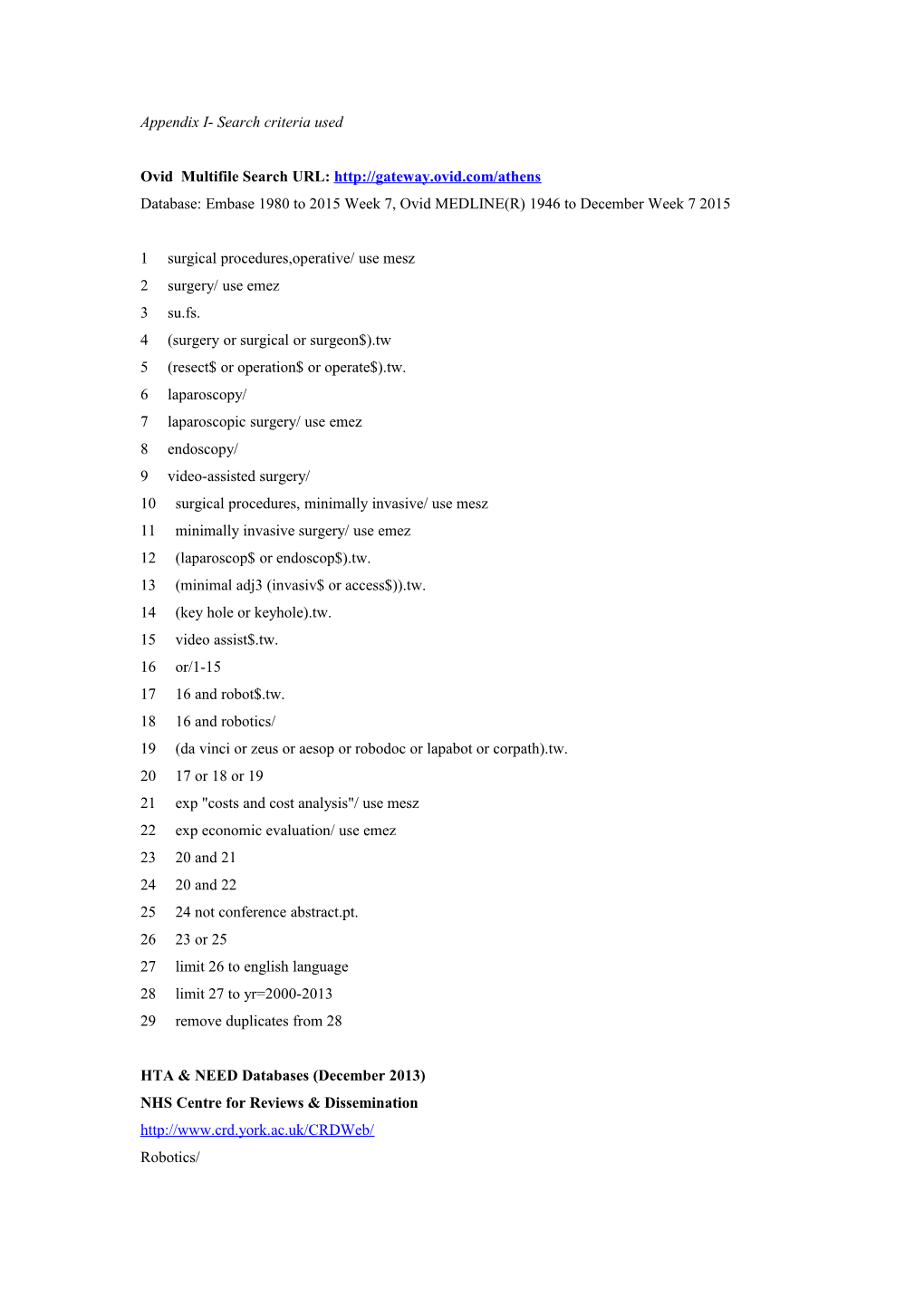
Ovid Multifile Search URL: http://gateway.ovid.com/athens Database: Embase 1980 to 2015 Week 7, Ovid MEDLINE(R) 1946 to December Week 7 2015
1 surgical procedures,operative/ use mesz 2 surgery/ use emez 3 su.fs. 4 (surgery or surgical or surgeon$).tw 5 (resect$ or operation$ or operate$).tw. 6 laparoscopy/ 7 laparoscopic surgery/ use emez 8 endoscopy/ 9 video-assisted surgery/ 10 surgical procedures, minimally invasive/ use mesz 11 minimally invasive surgery/ use emez 12 (laparoscop$ or endoscop$).tw. 13 (minimal adj3 (invasiv$ or access$)).tw. 14 (key hole or keyhole).tw. 15 video assist$.tw. 16 or/1-15 17 16 and robot$.tw. 18 16 and robotics/ 19 (da vinci or zeus or aesop or robodoc or lapabot or corpath).tw. 20 17 or 18 or 19 21 exp "costs and cost analysis"/ use mesz 22 exp economic evaluation/ use emez 23 20 and 21 24 20 and 22 25 24 not conference abstract.pt. 26 23 or 25 27 limit 26 to english language 28 limit 27 to yr=2000-2013 29 remove duplicates from 28
HTA & NEED Databases (December 2013) NHS Centre for Reviews & Dissemination http://www.crd.york.ac.uk/CRDWeb/ Robotics/ Appendix II- Adaptation of hierarchical levels suggested by Coyle and Lee[65] for the evaluation of the appropriateness of the data source used for key parameters Clinical effect size: 1. a. Meta-analysis of RCTs with direct comparison between comparator therapies, measuring final outcomes b. Single RCT with direct comparison between comparator therapies, measuring final outcomes c. Meta-analysis of RCTs with direct comparison between comparator therapies, measuring surrogate outcomes d. Meta-analysis of placebo-controlled RCTs with similar trial populations, measuring final outcomes for each individual therapy e. Single RCT with direct comparison between comparator therapies, measuring surrogate outcomes f. Single placebo-controlled RCTs with similar trial populations, measuring final outcomes for each individual therapy 2. a. Meta-analysis of placebo-controlled RCTs with similar trial populations, measuring a surrogate outcomes b. Single placebo-controlled RCTs with similar trial populations, measuring surrogate a outcomes for each individual therapy 3. Case–control or cohort studies 4. Non-analytic studies, for example, case reports, case series, Expert opinion 5. Expert opinion 6. Unclear/ not available Baseline clinical data 1. Case series or analysis of reliable administrative databases specifically conducted for the study covering patients solely from the jurisdiction of interest 2. Recent case series or analysis of reliable administrative databases covering patients solely from the jurisdiction of interest 3. Recent case series or analysis of reliable administrative databases covering patients solely from another jurisdiction 4. Old case series or analysis of reliable administrative databases. 5. Estimates from RCTs 6. Estimates from previously published economic analyses: unsourced 7. Unclear/ not available Resource Use 1. Prospective data collection or analysis of reliable administrative data from same jurisdiction for specific study 2. Recently published results of prospective data collection or recent analysis of reliable administrative data – same jurisdiction 3. Unsourced data from previous economic evaluations – same jurisdiction 4. Recently published results of prospective data collection or recent analysis of reliable administrative data – different jurisdiction 5. Unsourced data from previous economic evaluation – different jurisdiction 6. Expert opinion 7. Unclear/ not available Unit costs 1. Cost calculations based on reliable databases or data sources conducted for specific study – same jurisdiction 2. Recently published cost calculations based on reliable databases or data sources – same jurisdiction 3. Unsourced data from previous economic evaluation – same jurisdiction 4. Recently published cost calculations based on reliable databases or data sources – different jurisdiction 5. Unsourced data from previous economic evaluation - different jurisdiction 6. Expert opinion 7. Unclear/ not available
Utilities
1. Direct utility assessment for the specific study from a sample: a. of the general population b. with knowledge of the disease(s) of interest c. of patients with the disease(s) of interest 2. Indirect utility assessment from specific study from patient sample with disease(s) of interest: using tool validated for the patient population 3. Indirect utility assessment from a patient sample with disease(s) of interest; using a tool not validated for the patient population 4. Direct utility assessment from a previous study from a sample: a. of the general population b. with knowledge of the disease(s) of interest c. of patients with the disease(s) of interest 5. Indirect utility assessment from previous study from patient sample with disease(s) of interest: using tool validated for the patient population 6. Unsourced utility data from previous study – method of elicitation unknown 7. Patient preference values obtained from a visual analogue scale 8. Delphi panels, expert opinion 9. Unclear / not available Appendix III- Hierarchies of data sources for health economic analyses.
Quality of data used in health economic assessments for RAL surgery (according to the hierarchies adapted from Coyle&Lee and Cooper and colleagues)[65] Full-health economic evaluation studies – Quality Appraisal Clinical effect Baseline Resource use Costs Utilities size clinical data H 1 0 0 0 0 1 [12] i 2 2 [11, 16] 3 [11, 12, 6[11-16] 4 [11, 13, 14, 0 e 16] 16] r a 3 0 2 [14, 15] 0 0 3 [11, 13, 14] r 4 4 [12-15] 0 0 2 [12, 15] 0 c h 5 0 1 [13] 0 0 0 i 6 0 0 0 0 0 e s Not 0 0 0 0 2 (cost- o avialable minimisation) f [15, 16] e v i d e n c e
Cost-Analysis studies – Quality appraisal Clinical effect Baseline Resource use Costs Utilities size clinical data H 1 1 [39] 3 [25, 39, 2 [25, 39] 2 [25, 39] 1[39] i 52] e 2 1 [53] 32 [17, 18, 37 [18-24, 26- 39 [17-24, 26- 0 r 21-24, 26- 38, 40-52, 54- 38, 40-57] a 30, 32, 33, 57] r 36-38, 40- c 51, 54-57] h i 3 0 0 0 0 0 e 4 39 [17-38, 40- 1 [53] 1 [53] 0 0 s 52, 54-57] o f 5 0 5 [19, 20, 0 0 1 [25] e 31, 34, 35] v i 6 0 0 1 [17] 0 0 d Not 0 0 0 0 39 [17-24, 26- e avialable 36, 38, 40-52, n 54-57] c e Appendix IV- Cost of Robot assisted laparoscopic surgery compared to laparoscopy and/or open surgery in various diagnosis Author Count Disease Length of Cost (USD, 2014) per case Annual Initial Time (year of ry hospitalisat case cost horizon publicatio ion (days) assumpt of n) ion robot Urology Radical Yu et USA Bladder cancer Open:8 Open: NA Not Length cystectomy al[21] (stage not (7.8- 8.2) $26,291(IQR:25,169- includ of (2009) given) RAL: 8 27,414) ed hospital (7.2-8.8) RAL: $30,399 (IQR:27,062- ization (p=0.999) 33,737) (p=0.023) Lee et USA MIBC + Open: 8 Open: $22,146 – 27,262ŧ 361 Includ Length of al[30] Recurrent high RAL: 5.5 RAL: $22,082 -24,247 ŧ ed hospitalization (2010) grade NMIBC (p=0.75) Leow et al USA Bladder cancer Open: 11.8 Open: $26,681 NA Not 90 days [45] (stage not (11.5-12) RAL: $31,007 includ postope (2014) given) RAL: (p=0.08) ed rative 10.2(9.2- 11.3) (p=0.007) Radical Hohwu et Denm Prostate cancer NA Open: $4,956 (95% 110 Includ 1 year prostatecto al [12] ark (cT1-2) CI:4,260-5,550) ed my (2011) RAL: $10,737 (95% CI:9,596-11,552) $82,552 Incremental cost per successful operation (calculated from a societal perspective) Close et UK Prostate cancer 3.48 days $29,909 Incremental cost 200 Includ 10 years al [11] for RAL effectiveness ratio ed (2013) and RAL:$14,751 laparoscop Laparopscopy: $12,447 y
Conversion to open surgery additional 3 days
Complicati ons graded with Clavien Dindo: I: 1 additional day II: 2 additional days III: 3 additional days IV: 4 additional days V: Not applicable results in death Eldefrawy USA Prostate NA RAL: $24,330 NA Includ 10 years [17] Cancer (stage I- Open:$16,123 ed (2013) II) Scales et USA Prostate cancer Open: 2.5- Open:$9,887 336 Includ Length al [20] (stage not 3.2 RAL: $10,837 ed of given) RAL:1.3 hospital ization O`Malley Austr Prostate cancer Open>8 $1,828 incremental cost per 300 Includ Length and alia (stage not RAL~3 RAL compared to ed of Jordan given) Laparoscopy hospital [13] (Cost per procedure not ization (2006) given) Tomaszew USA Prostate cancer Open: 1.4 Open: $8,949±1,690 NA Includ Length ski [24] (stage not ±0.8 RAL: $14,430±2,049 ed of (2012) given) RAL:1.2±0. (p<0.05) hospital 6 ization (p>0.05) Bolenz et USA Prostate cancer Open: Open:$4,931(IQR:4,315- NA Not Length al. [26] (stage not 2.51±1.37 5,561) includ of (2009) given) Laparoscop Laparoscopy: $6,320 ed hospital y: (IQR:5,345-6,388) ization 1.76±0.83 RAL: $7,504 (IQR:6,797- RAL: 7,972) 1.56±1.53 (p<0.0001) (p<0.0001) Barbaro Italy Prostate cancer Open: Open:$ 7,097±2,134 NA Includ Length et al. [55] (stage not 8.1±4.9 RAL:$29,737±1,992 ed of (2009) given) RAL: 7±2.6 (p<0.0001) hospital (p=0.11) ization Hyams et USA Prostate cancer Open: 1.9 Open:$10,483 NA Not Length al. [33] (stage not (1-23) RAL:$14,676 includ of (2012) given) RAL: 1.7 (p<0.001) ed hospital (1-17) ization (p<0.001) Lotan et USA Prostate cancer Open: 2.5 Open: $6,741 300 Not Length al.[31] Laparoscop Laparoscopy:$7,332 includ of (2004) y: 1.3 RAL (no capital cost): ed hospital Robot: 1.2 $8,143 ization RAL: $8,836 Ho C et al Cana Prostate cancer 1.5 fewer $ 3,274(95% CI:-8,324- 130 Includ Length [15] da days than 12,400) )incremental cost ed of (2011) open per RAL compared to open hospital surgery ization 0.8 fewer $3,923(95% CI:-11,368- 130 Includ days than 18,014) incremental cost ed laparoscop per RAL compared to y Laparoscopy Ontario Cana Prostate 0.23 (0.02 Open: $11,104 NA Includ Length HTA da Cancer to 0.44) Laparoscopy: $11,476 ed of Committe lower for RAL: $13,641 hospital e [53] RAL vs ization (2010) Open + RT for (+) 0.38 (0.14 surgical to 0.91) margins lower for RAL vs. laparoscop y Flattery et Irelan Prostate cancer 1.5 $31,463(95% CI: 16,815- 200 Includ 10 years al [14] d (range:0.9- 72,286) Incremental cost ed (2011) 2.1) fewer effectiveness ratio days than ($/QALY) Open (Cost per procedure not given) 0.6 (range 0.1-1.2) fewer days than Laparoscop y
Yu et al,. USA Prostate cancer Open: Open: $10,567 (CI:8,123- NA Not Length [32] θ 2.4±4 12,947) includ of (2010) Laparoscop Laparoscopy:$10,991 ed hospital y:2±3.2 (CI:8,640-13,501) ization RAL:1.7±3. RAL: $11,778 (CI:8,860- 3 14,579) (p<0.001) (p=0.007) Hall et al. Austr Prostate cancer Open: 4.4 Open: $9,048 ($2,299- NA Not Length [54] alia (2-14) 22,808) includ of (2014) RAL: 1.2 RAL: $11,694 ($9,169- ed hospital (1-4) 16,303) ization
Simple & Yu et al,. USA Mixed group Open: Open: $13,679 (CI:10,023- NA Not Length Radical [32] 5.9±15.6 20,082) includ of Nephrectom (2010) Laparoscop Laparoscopy: $12,158 ed hospital y y:4.2±7.9 (CI:9,542-15,909) ization RAL:5.2±1 RAL:$15,146 (CI:12,068- 3.2 23,468) (p<0.001) (p<0.001) Partial Yu et al,. USA Renal tumour θ Open: Open: $12,882 (CI:9,972- NA Not Length nephrectom [32] 4.5±6.8 16,443) includ of y (2010) Laparoscop Laparoscopy: $13,519 ed hospital y:3.6±3.3 (CI:10,523-17,147) ization RAL:2.8±2. RAL:$17,141 (CI:11,114- 3 20,108) (p<0.001) (p=0.442) Mir et al. USA Renal tumour Open:5.9 Open: 300 Includ Length [34] Laparoscop $12,214(Rage:11,245- ed of (2010) y:3.2 14,384) hospital RAL:2.6 Laparoscopy: ization $11,021(Range: 9,131- 13,198) RAL:$12,786 (Range:10,948-14,434) Mano et USA Renal tumour Open: $3,240(range:-23,768- NA Includ 30 days al [50] 2.4±1.3 12,962) mean cost ed postope (2014) RAL: difference of RAL vs open rative 1.5±0.7 (p<0.001) (p<0.001) Castle et USA Renal tumour Open: 4 (3- RAL: $21,259 (18,404- 250 Includ 6 al.[37] (clinical stage 5) 23,331) ed months (2013) T1a) Laparoscop Open: $17,840 (15,461- ic radio- 20,334) frequency Laparoscopic radio- ablation: 1 frequency ablation: (1-2) $14,691 (12,580-17,560) Computer Computer tomography tomography guided radiofrequency guided guided ablation: $6,787 radiofreque (5,446-8,122) ncy guided ablation: 0 (0-1) RAL: 3 (3- 4) Pyeloplasty Yu et al,. USA UPJ Open:3±3 Open:$10,378 (CI:8,194- NA Not Length [32] obstruction θ Laparoscop 13,750) includ of (2010) y:2.2±1.2 Laparoscopy:$ 9,038 ed hospital RAL:2.2±1. (CI:8,282-12,645) ization 8 RAL:$12,895 (CI:9,167- (p=0.002) 18,248) (p=0.022) Seideman USA UPJ Laparoscop Laparoscopy: $9,502 300 Includ Length [35] obstruction y:1.9 RAL:$11,148 ed of (2011) RAL:1.5 hospital ization Varda et USA UPJ Open: 2 Open:$8,624 (7,673-9,576) NA Not 90 days al (2013) obstruction (2.5-3) Laparoscopy: $9,509 includ postope [48] Laparoscop (5,685-13,333) ed rative y: 2.3 (1.4- RAL: $12,909 (10,368- 3.2) 15,510) RAL: 2.1 (1.7-2.5) Gynecology Hysterecto Ontario Cana Uterine & RAL 2.05 Open: $8,177 NA Includ Length my HTA da Cervical (1.39-2.72) Laparoscopy: $8,976 ed of Committe Cancer lower than RAL: $10,800 hospital e [53] Open ization (2010) RAL 0.2(0.1-0.3) lower than Laparoscop y Wright et USA Cervical cancer More than Open: $10,280 NA Not Length al[22] (stage not 3 days Laparoscopy:$12,585 includ of (2011) given) Opem: 44% RAL: $10,877 ed hospital Laparoscop (p<0.0001) ization y: 11% RAL: 10% (p<0.0001)
Barnett et USA Endometrial Open: 4.4 Hospital perspective: 324 Includ Length al (2009) carcinoma (3.2-5.1) Open:$ 7,174 ed of [19] (stage not Laparoscop Laparoscopy: $7,640 hospital given) y: 1.2 (1.2- RAL: $9,560 ization 3) Societal perspective: RAL: 1 (1- Open:$13,898 2.3) Laparoscopy:$10,956 RAL:$12,415 Coronado Spain Endometrial Open: Open:$6,500±2,583 NA Includ Length et al[56] cancer (stage 8.1±4.8 Laparoscopy:$6,380±2,009 ed of (2011) not given) Laparoscop RAL:$7,011±3,291 hospital y: 4.6±4 (p=0.394) ization RAL: 3.5±3.4 (p=0.000 open compared to RAL and laparoscop y) Reynisson Swede Endometrial Open:7.3 Open: $13,613 400 Not Length et al[57] n cancer (Stage I- RAL:2.4 RAL: $15,399 includ of (2012) II) (Includes (p NS) ed hospital readmissio ization ns) Wright et USA Benign more than 2 Laparoscopy: NA Includ Length al. [29] gynecological days $7,139(IQR:5,555-9,270) ed of (2011) diseases Laparoscop RAL:$9,478 (IQR:7,254- hospital y: 24.9% 12,645) ization RAL:19.6% (p<0.001) (p<0.001) Wright et USA Endometrial More than Laparoscopy:$ 9,430 NA Includ Length al [23] carcinoma 2 days RAL: $11,131 ed of (2011) (stage not Laparoscop (p<0.01) hospital given) y: 11.4% ization RAL: 9.4% (p=0.23) Landeen USA Benign uterine Abdominal: Abdominal: $7,578±4,070 NA Includ Length et al, [36] diseases 2.7 ±1.4 (p<0.0001) ed of (2009) (p<0.0001) Vaginal: hospital Vaginal: $7,464±1,791(p<0.0001) ization 1.9±0.8 Laparoscopy:$ (p<0.0001) 7,464±3,292(p<0.0001) Laparoscop RAL: y: $8,800±1,920(p<0.0001) 1.8±1.5(p< 0.0001) RAL: 1.9±0.8 Pasic et USA Any disease Laparoscop Laparoscopy:$7,543±1,262 NA Not Length al. [28] requiring y: 1.4±0.2 RAL: $10,428 ±1,746 includ of (2009) hysterectomy RAL: (p<0.01) ed hospital 1.3±0.1 ization (p<0.01) Leitao Jr. USA Uterine Cancer Laparoscop Open:$25,832 ±10,922 Average Includ 6 et al. [44] y: 2 (1-15) Laparoscopy:$ 780 ed months (2014) RAL: 1 (0- 21,478±11,553 5) RAL: $24,788±11,348
Rosero et USA Benign Laparoscop Laparoscopy: $7,801 NA Not Length al [38] gynecological y: 1 (1-2) (6,039-10,243) includ of (2013) disease RAL 1 (1-2) RAL: $10,462 (7,594- ed hospital 13,660) ization
Woelk et USA Benign uterine Abdominal: RAL vs Abdominal: -$983 NA Not 6 weeks al.[49] diseases 3.4 ±2.3 (-3,063 to 1,099) includ postope (2014) RAL: ed rative 1.6±1.6 Vaginal: RAL vs vaginal: $2,437 1.9±0.8 ($1,051 to $3,824) RAL: 1.5 ±1.2 Dayaratn USA Benign NA Total vaginal: $8,284 NA Not Length a et al. gynecological (7,980-8,599) includ of [40] disease Laparoscopic assisted ed hospital (2013) vaginal hysterectomy: ization $10,554 (10,184-10,939) Total laparoscopic:$12,116 (10,603-13,844) RAL: $14,077 (12,643- 15,674) Teljeur et Irelan Uterine disease Model Weighted average of 100 Includ Length al. [16] d assumption Incremental cost of RAL (CI:75- ed of (2014) s: surgery vs mixed service 125) hospital Radical provision of open and ization hysterectom laparoscopy: $3,821 (CI: (patients y: 2,913 – 4,856) were Difference assumed RAL vs [Weighted average based to be of open: -3.4 on 4% radical, 70% simple equivale (-6.2to-0.5) total, 26% simple total with nt health Difference nodal staging) once RAL vs discharg laparoscop ed) y: -0.4(-1.7 to 1)
Simple total hysterectom y: Difference RAL vs open: -2 (- 2.6 to -1.4) Difference RAL vs laparoscop y: --0.3 (- 0.7to0.2)
Simple total hysterectom y with node staging: Difference RAL vs open: -3 (- 5.3 to -0.6) Difference RAL vs laparoscop y: -0.5(-1.8 to 0.8) Flattery et Irelan Uterine disease 2.6 $3,564 Incremental cost per 297 Includ 10 years al [14] d (range:2.2- RAL surgery compared to ed (2011) 2.9) fewer Open/laparoscopy days than (Cost per procedure not Open given)
0.4 (range 0.2-0.6) fewer days than Laparoscop y
Sacrocolop Anger etl USA Pelvic organ NA Laparoscopy: $12,369 300 Includ 6 weeks opexy al. (2014) prolapse (SD:4,129) ed postope [39] RAL: $21,240 (SD:3,386) rative Gastrointestinal Heller Shaligram USA Achalasia Open:4.4±5 Open: $10,275±10,599 NA Not 30 days myotomy et al .2 Laparoscopy: includ post- (2011) Laparoscop $7,441±8,278 ed dischar [18] y: 2.7±3.8 RAL: $9,869±5,781 ge RAL: (RAL vs open p= 0.65) 2.4±2.6 (RAL vs (RAL vs. Laparoscopy=0.0028) open: p=0.0001) (RAL vs Laparoscop y p=0.34) Antireflux Oewn et USA Esophageal Open: Open: $13,152 ±14,405 NA Not 30 days surgery al. (2014) reflux or 6.1±7.2 Laparoscopy: includ post- [46] Diaphragmatic Laparoscop $8,209±7,180 ed dischar hernia y: 2.8±3.6 RAL:$10,966±6,224 ge RAL: 3±3.5 Colectomy Tyler et USA Benign & Laparoscop Laparoscopy: $16,896 NA Not Length al. [27] Malign diseases y: 5.4 (5.3- (95% CI:15,775-16,362) includ of (2013) of the colon 5.5) RAL:$20,555 (95% ed hospital RAL: 5.5 CI:18,182-21,011) ization (5-5.9) (p,0.001) (p=0.664) Juo et al USA Benign & Open: 6 Median cost Laparoscopy: NA Not Length (2014) Malign diseases (vs. $12,790 (IQR: 7,035) includ of [42] of the colon Laparoscop RAL: $15,869 (IQR: 9,213) ed hospital y p<0.01) (p<0.001) ization Laparoscop y:4 (vs RAL p=0.008) RAL:4
Keller et USA Benign & Laparoscop Laparoscopy: $16,657 (CI: NA Not Length al. (2014) Malign diseases y: 5.8 (5.6- 16,287-17,038 ) includ of [43] of the colon 5.9) RAL: $20,261 (CI: 19,535- ed hospital RAL: 6.2 21,768) ization (5.9-6.6) Resection of Keller et USA Benign & Laparoscop Laparoscopy: $19,269 (CI: NA Not Length rectum al. (2014) Malign diseases y: 6.6 (6.1- 18,061-20,559) includ of [43] of the rectum 7.1) RAL: $24,531 (CI: 21,409- ed hospital RAL: 6.6 28,108) ization (5.6-7.8) Cholecystec Breitenste Switze Symptomatic Laparoscop Laparoscopy: $6,819±2174 300 Includ Length tomy in[52] rland cholecystolythia y:4.8±2.2 RAL: $8,705±1957 ed of (2007) sis RAL:4.5±1. (p<0.01) hospital 9 ization (p=0.4) Obesity Hagen et Switze Morbid obesity Open: 10.9 Open: $24,111 84 Includ Length operation al [51] rland (vs RAL Laparoscopy: $22,745 ed of (2011) p<0.0001) RAL: $20,298 hospital Laparoscop ization y: 11 (vs. RAL p=0.001) RAL:7.4 Cardiothoracic Thoracic Swanson USA Benign & Lobectomy NA Not surgery etl al [47] Malign diseases VATS: VATS: $21,096 includ Length (2014) of the lung 5.8±5 (SD:11,309) ed of RATS: RATS: $25,798 (SD: hospital 6±6.4 13,562) ization Wedge resection VATS: VATS: $17,103 5.3±5.2 (SD:10,681) RATS: RATS: $20,185 (SD:9,574) 5.2±5.1 Deen et al USA Stage I or II Open: 5.4 Open:$15,036 NA Includ Length (2013) Lung cancer VATS: 4.7 VATS:$13,829 ed of [43] Robot: 4.6 Robot:$17,011 hospital ization Cardiac Poston et USA CAD Open: Open:$17,983±3086 100 Includ Length al[25] 6.3±2 Robotic hybrid: ed of (2007) Robotic $26,005±3704 hospital hybrid:3.7± (p=0.001) ization 1.5 (p<0.001) ŧ: cost varies with urinary diversion type (ileal conduit, continent cutaneous diversion & orthotopic neobladder). Θ: Clinical diagnosis is not given in the study. These are the most logical diagnosis assumed. IQR: Interquartile range SD: Standard deviation VATS: Video assisted thoracic surgery CI: confidence interval CAD: Coronary artery disease NA: Not available
Appendix V – Appraisal of studies according to “Guidelines for authors and peer reviewers of economic submission to British Medical Journal”.
Study design. Yes No Not Not clear applicable 1. The research question is stated. 47 (100%) 2. The economic importance of the research 46 1 (2%) question is stated. (98%) 3. The viewpoint(s) of the analysis are clearly 17 13 17 (36%) stated and justified. (36%) (28%) 4. The rationale for choosing alternative 45 1 (2%) 1 (2%) programmes or interventions compared is (96%) stated. 5. The alternatives being compared are clearly 45 1 (2%) 1 (2%) described. (95%) 6. The form of economic evaluation used is 16 15 16 (34%) stated. (34%) (32%) 7. The choice of form of economic evaluation 12(26%) 19 16 (34%) is justified in relation to the questions (40%) addressed. Data collection. 8. The source(s) of effectiveness estimates 47 0 0 0 used are stated. (100%) 9. Details of the design and results of 38 0 9 (19%) 0 effectiveness study are given (if based on a (81%) single study). 10. Details of the methods of synthesis or meta- 8 (17%) 5 34 (72%) analysis of estimates are given (if based on (11%) a synthesis of a number of effectiveness studies). 11. The primary outcome measure(s) for the 31 4 (8%) 12 (26%) economic evaluation are clearly stated. (66%) 12. Methods to value benefits are stated. 8(17%) 2 (4%) 37 (79%) 0 13. Details of the subjects from whom 7 (15%) 0 39 (83%) 1 (2%) valuations were obtained were given. 14. Productivity changes (if included) are 3 (6%) 5 39 (83%) 0 reported separately. (11%) 15. The relevance of productivity changes to the 3 (6%) 3 (6%) 41 (87%) 0 study question is discussed. 16. Quantities of resource use are reported 39 7 1 (2%) separately from their unit costs. (83%) (15%) 17. Methods for the estimation of quantities and 46 1 (2%) 0 unit costs are described. (98%) 18. Currency and price data are recorded. 35 10 2 (4%) (74%) (21%) 19. Details of currency of price adjustments for 7 (15%) 39 1 (2%) inflation or currency conversion are given. (83%) 20. Details of any model used are given. 8 (17%) 0 36 (76%) 3( 6%) 21. The choice of model used and the key 8 (17%) 2 (4%) 37 (79%) 1 (2%) parameters on which it is based are justified. Analysis and interpretation of results 22. Time horizon of costs and benefits is stated. 13 31 0 3 (6%) (28%) (66%) 23. The discount rate(s) is stated. 5 (11%) 19 23 (49%) 0 (40%) 24. The choice of discount rate(s) is justified. 5 (11%) 0 42 (89%) 0 25. An explanation is given if costs and benefits 1 (2%) 1 (2%) 45 (95%) are not discounted. 26. Details of statistical tests and confidence 4 (9%) 1(2%) 42 (89%) intervals are given for stochastic data. 27. The approach to sensitivity analysis is 16 0 31 (66%) 0 given. (34%) 28. The choice of variables for sensitivity 8 (17%) 8 31 (66%) 0 analysis is justified. (17%) 29. The ranges over which the variables are 7 (15%) 9(19%) 31(66%) 0 varied are justified. 30. Relevant alternatives are compared. 16 1 (2%) 30 (64%) 0 (34%) 31. Incremental analysis is reported. 9 (19%) 8 30 (64%) 0 (17%) 32. Major outcomes are presented in a 45 2 (4%) disaggregated as well as aggregated form. (95%) 33. The answer to the study question is given. 47 0 (100%) 34. Conclusions follow from the data reported. 45 2(4%) (95%) 35. Conclusions are accompanied by the 44 3(6%) appropriate caveats. (94%)