RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES BANGALORE
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
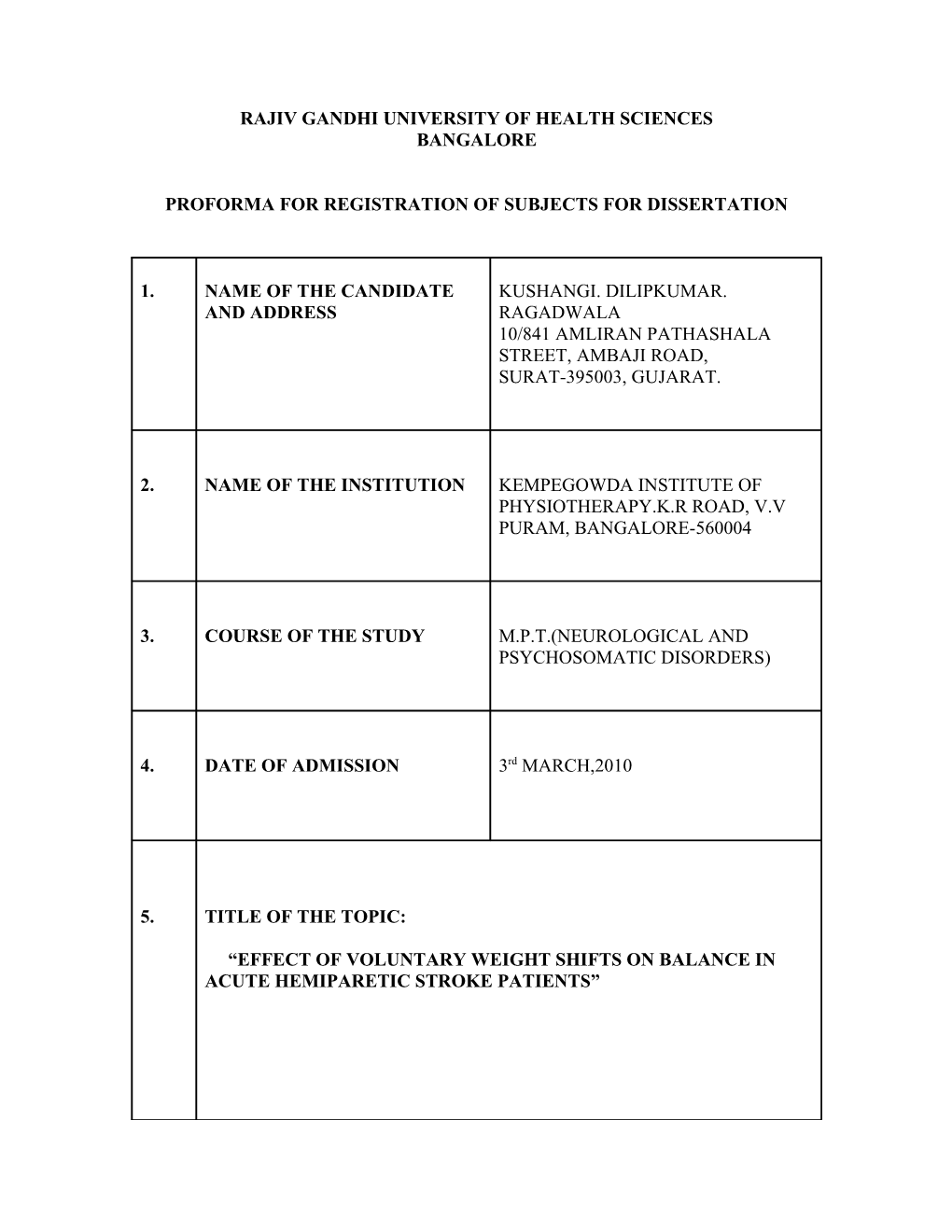
1. NAME OF THE CANDIDATE KUSHANGI. DILIPKUMAR. AND ADDRESS RAGADWALA 10/841 AMLIRAN PATHASHALA STREET, AMBAJI ROAD, SURAT-395003, GUJARAT.
2. NAME OF THE INSTITUTION KEMPEGOWDA INSTITUTE OF PHYSIOTHERAPY.K.R ROAD, V.V PURAM, BANGALORE-560004
3. COURSE OF THE STUDY M.P.T.(NEUROLOGICAL AND PSYCHOSOMATIC DISORDERS)
4. DATE OF ADMISSION 3rd MARCH,2010
5. TITLE OF THE TOPIC:
“EFFECT OF VOLUNTARY WEIGHT SHIFTS ON BALANCE IN ACUTE HEMIPARETIC STROKE PATIENTS” 6. BRIEF RESUME OF THE INTENDED WORK
6.1 NEED FOR THE STUDY:
Like all the developing countries, Stroke is fast emerging as a major public health problem in India.[1,2] Stroke is one of the most common neurological disorders leading to chronic disability.[3] Stroke is an acute onset neurological dysfunction due to an abnormality in cerebral circulation with resultant signs and symptoms that correspond to involvement of focal areas of the brain.[4] Hemiparesis is the most frequent neurological deficit after Stroke.[5] Risk factors: hypertension, cardiovascular disease, diabetes mellitus, increased serum cholesterol levels, obesity, heavy alcohol consumption, cocaine use, cigarette smoking.[4,6] Stroke is the 3rd commonest cause of mortality and the 4th leading cause of disease burden.[7,8] In 2005, Stroke accounted for nearly 5.7 million deaths and 16 million cases of first ever Strokes worldwide.[7,8] Countries with large populations [like India, China, Brazil, Russia ] contribute for greater number of deaths and disability due to Stroke.[8,9,10,11] The Indian Council of Medical Research (ICMR) estimates indicated that amongst the non-communicable disease, Stroke contributes for 41% of deaths and 72% of disability adjusted life years.[8,12] Stroke incidence in India has been registering an upward trend in the last few decades, while the incidence of Stroke in western countries has declined or plateaued.[2,13] Average life expectancy for Indians is lower than American, European, and Japanese populations, which exclude the population at higher risk, thereby bringing the prevalence rate.[2] A recent Indian study has suggested that squatting during toilet use, common throughout India, raise B.P and could be an important triggering factor for Stroke.[2,14] Stroke is expected to assume epidemic proportions in India in the coming years and will strain its already limited health care infrastructure.[2] Public education, strict control of risk factors at primary care level is the most appropriate strategy for India to meet the growing challenge of Stroke.[2] Clinically, acute Stroke patient presents as arms hangs by the side- humerus internally rotated, elbow extended, forearm pronated; trunk is weak, the ribs flare, and posture is impaired with a convex lateral curve seen on the affected side; in Standing, client has problems recruiting strength on the affected leg.; the pelvis lists downward and the hip and knee flex; as the client learns to walk, either the knee flexes or the patient compensates and locks the knee in extension. [4] Sequential stages of recovery: - evolution of the recovery process from onset to community life is in three stages: 1.Acute [5-45 days] [15], 2.Active [rehabilitation], 3. Adaptation to personal environment.[4] Balance is complex process involving the reception and integration of sensory input, planning, and execution of movements, to achieve a goal requiring upright posture. [3] It is the ability to control COG over BOS in a given environment. Hemi paretic Stroke patients frequently present balance abnormalities.[5] Following acute Stroke, the ability to move outside the base of support in sitting, balance in standing and move from sitting to standing and back again is critical to independence.[16]
There are three systems in body that works coordinately to control balance: 1. Visual, 2. Vestibular, 3. Somatosensory. A Stroke can affect balance because of an injury to one of the systems that controls balance, damage to system connecting loops to the brain, injury to brain.[17] The main objective for hemi paretic patient is the rehabilitation of their impaired ability to accept and bear body weight on the involved lower extremity. [18] Major requirements for good balance are an accurate sense of being balanced, the ability of muscle, particularly of the lower limb, to produce force rapidly and at the appropriate time and muscles which are extensible i.e not stiff or short.[19] Physiotherapist challenges balance there by retraining receptors to respond to information. The brain relearns how to interpret the information and forms new movement plans for adjusting balance.[17] Studies have shown that when leaning their body as far as possible in a specific direction without adjusting foot position, Stroke patients have difficulties in all planes but mostly in direction of their paretic leg.[20] When shifting from two-legged to one-legged stance or when stepping on stairs of various heights, Stroke patients show the greatest difficulties with transferring weight toward their paretic leg.[20] Step Test has high test-retest reliability 0-94 for performance with normal leg. It assesses an individual’s ability to place one foot onto 7.5 cm high step and then back down to the floor repeatedly as fast as possible. The step is placed 5cm in front of the individual’s feet. the test is scored by recording the number of steps completed in the 15 seconds period for each leg.[21] Berg Balance Scale is recommended assessment of balance for post stroke rehabilitation-14 balance items graded on 5-point scale ranging from 0-4; 0- patient inability to perform the task; 4- independence.[22] Voluntary Weight Shifts i.e. emphasis is on performing tasks which require voluntary movements of the body mass in sitting and standing.[19] Balance control is necessary in daily life as: during performance of self-initiated action and when predicting destabilization and taking avoiding action and when walking a reactive response as a last resort in an attempt avoid a fall.[19] Sitting balance training is done by making patient to sit on a chair (without back rest and arm rest) and then reaching tasks are given in different directions. Standing balance training is done by making the patient stand with feet few centimeters apart and then reach outs in different directions are given to load the paretic extremities. [19]
PURPOSE OF THE STUDY:
This study is related to know the effectiveness of Voluntary Weight Shifts on Balance in Acute Hemi paretic Stroke patients.
HYPOTHESIS:
Null Hypothesis: There will be no significant effect of Voluntary Weight Shifts on Balance in Acute Hemi paretic Stroke patients.
Alternate Hypothesis: There will be significant effect of Voluntary Weight Shifts on Balance in Acute Hemi paretic Stroke patients.
6.2 REVIEW OF LITERATURE:
Snehal Bhupendra Shah, et al. [2006] Stroke is an acute onset neurological dysfunction due to an abnormality in cerebral circulation with resultant signs and symptoms that correspond to involvement of focal areas of the brain.[3]
Subhash Kaul [2007] Stroke is expected to assume epidemic proportions in India in the coming years and will strain its already limited health care infrastructure.[2]
Subhash Kaul [2007] The last few decades have seen a rise in the incidence and prevalence of Stroke in India, attributable to increasing life span, urbanization, and better survival, and the rates are now matching western figures. [2]
D. Nagaraja, et al. [2009] Despite limitations of resource constraints, the present study has shown that population based stroke surveillance is possible and feasible and needs to develop specific mechanisms to overcome challenges in India.[8]
Snehal Bhupendra Shah, et al. [2006] Balance is defined as a complex process involving the reception and integration of sensory inputs, planning and execution of movements, to achieve a goal requiring upright posture.[3]
Department of Rehabilitation Services; The Ohio State University Medical Center [2002] Balance is controlled by several systems of body working together sending signals and getting signals from brain; after Stroke brain relearns interpretation and execution of information to formulate movement.[17]
Clarissa Barros de Oliveira, PT, et al. [2008] Hemi paretic Stroke patients frequently present balance abnormalities and therapeutic approaches depends on appropriate balance evaluation thus their study have different tools for balance assessment have validated.[12]
Vicki Stemmons Mercer, et al. [2009] The Step Test, performed with the non-paretic limb as the stepping limb, demonstrates convergent validity as a measure of paretic–lower extremity loading in individuals recovering from Stroke.[21] Berg K, et al. [1989] Berg balance scale is valid measuring tool for balance. Both inter rater and intra rater reliability is high(r=.0.95). [22] Julie Sanford, et al. [1993] The overall reliability of Fugl-Meyer assessment was high; this instrument has good construct validity and high reliability[r=0.99] for determining motor function and balance. [23]
Ruth Dickstein, et al. [1994] In their study pointed out the larger sways manifested in voluntary weight shifts as compared to automatic weight shifts.[18] Mirjam de Haart, MD, et al. [2005] Even severe Stroke patients who are selected for inpatient rehabilitation to retrain gross motor skills can substantially improve their weight-shifting capacity in the frontal plane during a 12-week training period of individualized physiotherapy, in terms of both speed and precision.[20]
TE Howe, et al. [2005] Sway value during static standing and time to return from reaching in sitting indicated a significant improvement in postural control over time.[16]
Laufer Y, et al. [2000] Raising foot on a step appears to be an appropriate strategy for weight shifting as it is impaired in both paretic and non- paretic limb of stroke.[24]
Wilson, et al. [1987] The Behavioral Inattention Test, initially called as Rivermead Behavioral Inattention Test, is a short screening battery of tests to assess the presence and the extent of visual neglect on a sample of everyday problems faced by patients with visual inattention.[25]
Diller, et al. [1974] The Single Letter Cancellation Test (SLCT) is used to evaluate the presence and severity of visual scanning deficits, and is used to evaluate unilateral spatial neglect (USN) in the near extra personal space.[26]
Schubert and Spatt [2001] The Line Bisection Test is a test is a quick measure to detect the presence of unilateral spatial neglect (USN).[27]
6.3 OBJECTIVE OF THE STUDY:
To assess the effect of voluntary weight shifts on paretic limb in acute hemi paretic stroke patients. To assess the effect of voluntary weight shifts on sitting balance. To assess the effect of voluntary weight shifts on standing balance. To assess the effect of voluntary weight shifts in improving functional ability.
7. MATERIALS AND METHODS:
7.1 SOURCE OF DATA: Out Patient Department of General Medicine in Kempegowda Institute of Medical Science Hospital and Research Center, Bangalore. Out Patient Department of Physiotherapy in Kempegowda Institute of Medical Science Hospital and Research Center, Bangalore. Out Patient Department of Neurology-Neurosurgery in Kempegowda Institute of Medical Science Hospital and Research Center, Bangalore.
7.2 METHODS OF COLLECTION OF DATA:
(a) Study Design: A Single Group Interventional Study.
Sample size: 30
Materials Used: chair(without arm rest and back rest) high table cargo box stool target objects e.g.- glass, pen, piles of books measuring tape Step of height 7.5 centimeter.
(b) Inclusion Criteria: Patient with hemispheric intra cerebral infarction. Age 45-60 years Post stroke within 45days. Both male and female. Either right-sided or left-sided hemiparesis A score of less than or equal to 7 on Balance scale of the Fugl- Meyer assessment.
(c) Exclusion Criteria: Cerebellar stroke, vertebra basilar artery insufficiency. Patient with history of orthopedic, vestibular, and other neurological conditions. Patient with perceptual and cognitive deficits like hemi spatial neglect; attention and memory deficits. Patient having lower extremity deformity. Patient with terminal illness or medically unstable. Severe cardiovascular disease.
7.3 Does the study require any Investigations or Interventions to be conducted on Patients or other Humans or Animals? If so , Please describe briefly: Yes, an intervention on patients is required.
Methodology: Assess the patient for inclusion and exclusion criteria. Explain the patient about the treatment procedure. Patient informed consent will be taken
Evaluation of perception and cognition: it is done using Behavioral Inattention Test. [25] 1. Letter cancellation test- The test consists of one 8.5"x11" sheet of paper containing 6 lines with 52 letters per line. The stimulus letter H is presented 104 times. The page is placed at the patient's midline. The patient is told to put a line through each H that is found on the page. The time taken to complete the test is recorded. The score is calculated by subtracting the number of omissions (H's that were not crossed out) from the possible perfect score of 104 (0 to 53 on the left and 0 to 51 on the right). Higher scores indicate better performance. Omissions of 4 or more have been found to be pathological.[26] 2. Line bisection test- Patients are asked to place a mark with a pencil (with their preferred or unaffected hand) through the center of a series of 18 horizontal lines on an 11x 8.5-inch page. Usually, a displacement of the bisection mark towards the side of the brain lesion is interpreted as a symptom of neglect. The test is scored by measuring the deviation of the bisection from the true center of the line. A deviation of more than 6 mm from the midpoint indicates USN. Omission of two or more lines on one half of the page indicates USN(Unilateral Spatial Neglect).[27] Fugl-Meyer scoring for balance for inclusion criteria- this is an impairment based test with items organized by sequential recovery stages. A 3-point ordinal scale is used to measure impairments of volitional movement with grades ranging from 0[item cannot be performed] to 2[item can be fully performed]. This instrument requires an estimated 30-40 min to administer. The balance section with maximum score of 14 was used. The patient with the score of less than or equal to 7 on this scale are recruited.[6] Evaluation of Step Test-it assesses an individual’s ability to place one foot onto a 7.5cm high step and then back down to the floor repeatedly as fast as possible. The step is placed 5cm in front of the patient’s feet. The test is scored by recording the number of steps completed in the 15 seconds period for each leg. The test is performed first with the non-paretic foot and then with the paretic foot placed on and off. Step test scores for stepping with the non-paretic leg were analyzed.[8] Evaluation of Berg Balance Scale-it has 14 items graded on 5-point scale ranging from 0-4; 0-patient inability to perform the task; 4-independence.[22] Patients referred are evaluated pre-training using Step test and Berg balance scale then they are trained using voluntary weight shifts Explain the procedure Give clear instructions to the patient.
Sitting balance exercises-patient is made to sit on a chair without arm rest and back rest, hands on lap, feet and knees approx. 15 centimeters apart, feet on floor. 1) Turning head and trunk to look over the shoulder, returning to mid position and repeating to other side. 2) Looking up at the ceiling and returning to upright. 3) Reach to touch the objects [beyond arm’s length] with paretic hand: forward [flexing at the hips]; sideways [both sides]; backward; then returning to mid-position. Initially objects to be picked up from stool then progression is made by picking from the floor [use of one hand-both hands]. Very weak patients can practice reaching action with arms resting on a high table. Progression of exercise is made by reaching with non-paretic arm across the body to load the paretic foot. Standing balance exercises-patient made to stand with feet few cms apart. 1) Look up at ceiling and return to upright 2) Turn head and body mass and look behind and return to mid position, repeat to other side. 3) Reaching to touch or pick objects forward, sideways (both sides), backward. Initially object placed at arm level then gradually level of object is decreased. Reaching with one hand or both the hand is done. Reaching is given beyond arm’s length. Progressively reaching is made to practice across the body. 4) Single leg support- stepping forward with non-paretic limb to place foot on a step, practice reaching tasks. 5) Standing and picking up objects from floor in forward direction and placing it on the table beside. Stepping exercises- Stepping to markers on the floor. Stepping onto high step.[19]
After training, the patients are evaluated for Balance using Step test and Berg balance scale.
Frequency: Thirty-forty five minutes per session[20] Five days per week[3] Four weeks training[16]
Duration of the Study: 12 months
Statistical Analysis: Student’s PAIRED-t test. Any other suitable test will be applied at the time of data analysis.
7.4 Has Ethical Clearance been obtained from your Institution in case of 7.3? Yes. 8. LIST OF REFERENCES :
1) Poungvarin N. Stroke in the developing countries. Lancet 1998; 352:19-22.
2) Subhash Kaul. Stroke in India: Are We Different from the World? Pak J Neurol Sci 2007 ; 2(3):158-64 .
3) Snehal Bhupendra Shah, Smita Jayavant. Study of Balance training in ambulatory Hemiplegics. The Indian Journal of Occupational Therapy April - July 2006; 38: 1.
4) Darcy A. Umphred, Susan P. Ryerson. Chapter 27, Hemiplegia. Neurological Rehabilitation, 5th edition. Elsevier 2007; 858,863,877.
5) Clarissa Barros de Oliveira, Ítalo Roberto Torres de Medeiros, Norberto Anizio Ferreira Frota, Mário Edvin Greters, Adriana B Conforto. Balance control in Hemiparetic Stroke patients: Main tools for Evaluation. Journal of Rehabilitation Research and Development 2008; 45: no. 8: 1215-26.
6) Susan B O’sullivan, Thomas J Schmitz. Chapter 18, Stroke. Physical Rehabilitation, 5th edition. Jaypee brothers 2007; 707,735, 774.
7) Strong K, Mathers C, Bonita R. Preventing stroke: saves lives around the world. Lancet Neurol 2007; 6:182-7.
8) D. Nagaraja, G. Gururaj, N. Girish, Samhita Panda, A.K. Roy, G.R.K. Sarma, R. Srinivasa. Feasibility study of stroke surveillance: Data from Bangalore, India. Indian J Med Res October 2009; 130: 396-403.
9) Feigin VL. Stroke in developing countries: Can the epidemic be stopped and outcomes improved. Lancet Neurol 2007; 6:94-97.
10) World Health Organization. The economic impact of Chronic Diseases in preventing chronic diseases: a Vital Investment. World Health Organization Geneva 2005.
11) Liu M, Wu B, Wang W, Lee L, Zhang S, Kong L. Stroke in China: Epidemiology, Prevention and Management Strategies. Lancet Neurol 2007; 8: 456-64.
12) Indian Council for Medical Research. Stroke in: Assessment of the burden of Non-communicable diseases: Final project report, New Delhi. Indian Council of Medical Research 2004: 18-22.
13) Garraway WM, Whisnant JP, Drury I. The Continuing Decline in the Incidence of Stroke. Mayo Clinical Practice 1983; 58: 520-23. 14) Feldmann E, Daneault N, Kwan E, Ho KJ, Pessin MS, Langenberg P, Caplan LR. Chinese-white differences in the distribution of Occlusive Cerebrovascular Disease. Neurology 1990; 40: 1541-42.
15) Baldhomero Ranjo II. Mental Practice Improves Balance in Acute Stroke Patients: A Series of Single-System Studies. http://afrdis.mmsu.edu.ph/researchinfo.php?code=382.
16) TE Howe, I Taylor, H Jones. Lateral weight transference exercises following Acute Stroke: a preliminary study of clinical effectiveness. Clinical Rehabilitation 2005; 19: 45-53.
17) Department of Rehabilitation Services. The Ohio State University Medical Center; Balance Changes after a Stroke 2002.
18) Ruth Dickstein, et al. Automatic and Voluntary Lateral Weight Shifts in Rehabilitation of Hemiparetic patients. Clinical Rehabilitation May 1994; 8: 91-99.
19) Janet H Carr, Roberta B Shepherd. Chapter-2, BALANCE. Stroke Rehabilitation, 5th edition. An imprint of Elsevier 2003; 33-75.
20) Mirjam de Haart, Alexander C. Geurts, Mylène C. Dault, Bart Nienhuis, Jacques Duysens. Restoration of Weight-Shifting Capacity in Patients with Post-acute Stroke: A Rehabilitation Cohort Study. Archives Physical Medicine Rehabilitation 2005; 86: 755-62.
21) Vicki Stemmons Mercer, Janet Kues Freburger, Shuo-Hsiu Chang, Jama L. Purser. Measurement of Paretic–Lower-Extremity Loading and Weight Transfer after Stroke. American Physical Therapy Association 2009; 89: No. 7:653-64.
22) Berg K, Wood-Dauphinee S, Williams JI, Maki, B. Measuring balance in the elderly: Validation of an instrument. Physiotherapy. Canada 1989; 41: 304- 11.
23) Julie Sanford, Julie Moreland, Laurie R Swanson, Paul W Stratford and Carolyn Gowland. Reliability of the Fugl-Meyer Assessment for Testing Motor Performance in Patients Following Stroke. Physical Therapy July 1993; 73: no. 7: 447-54.
24) Laufer Y, Dickstein R, Resnik S, Marcovitz E. Weight-bearing shifts of hemi paretic and healthy adults upon stepping on stairs of various heights. Clinical Rehabilitation 2000; 14: 125-29.
25) Sabrina Figueiredo, et.al. The Behavioral Inattention Test. http://www.medicine.mcgill.ca/strokengine-assess/module_bit_intro-en.html 26) Lisa Zeltzer, MSc OT, Anita Menon, MSc. The Single Letter Cancellation Test. http://www.medicine.mcgill.ca/strokengine-assess/module_slct_indepth en.html.
27) Lisa Zeltzer, MSc OT, Anita Menon, MSc. The Line Bisection Test. http://www.medicine.mcgill.ca/strokengineassess/module_lbt_indepth- en.html.
28) http://www.ncbi.nlm.nih.gov/pubmed/10763788.
9. Signature of the Candidate: 10. Remarks of the Guide:
11. Names and Designation of:
11.1 Guide: PREM KUMAR.B.N ASSISTANT PROFESSOR
11.2 Signature:
11.3 Co-guide: Dr. VEDAVATHI PROFESSOR
11.4 Signature:
11.5 Head of the Department: PROF. R.BALASARVANAN
11.6 Signature :
12.1 Remarks of the Chairman & Principal: 12.
12.2 Signature: