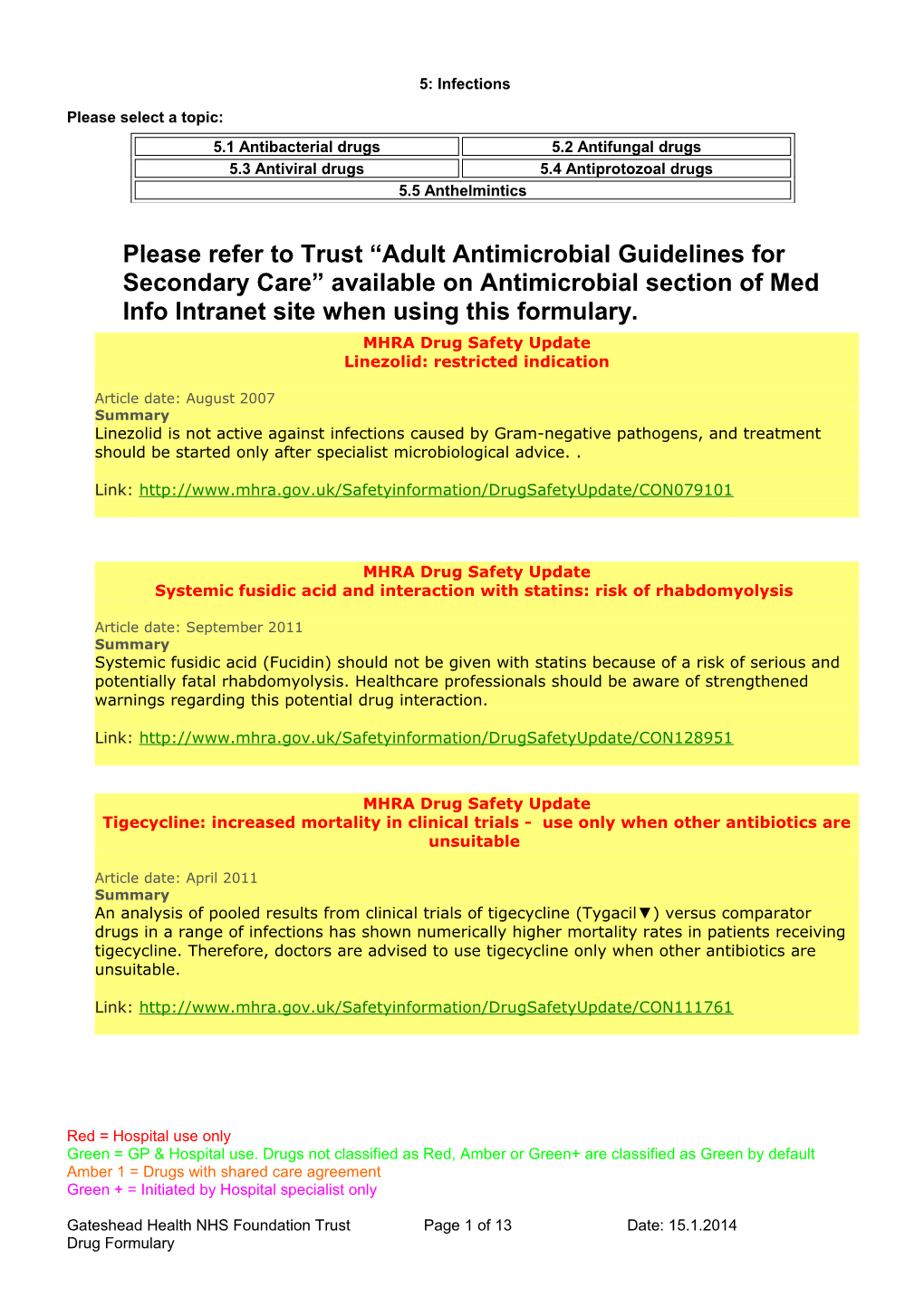
5: Infections
Please select a topic: 5.1 Antibacterial drugs 5.2 Antifungal drugs 5.3 Antiviral drugs 5.4 Antiprotozoal drugs 5.5 Anthelmintics
Please refer to Trust “Adult Antimicrobial Guidelines for Secondary Care” available on Antimicrobial section of Med Info Intranet site when using this formulary. MHRA Drug Safety Update Linezolid: restricted indication
Article date: August 2007 Summary Linezolid is not active against infections caused by Gram-negative pathogens, and treatment should be started only after specialist microbiological advice. .
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON079101
MHRA Drug Safety Update Systemic fusidic acid and interaction with statins: risk of rhabdomyolysis
Article date: September 2011 Summary Systemic fusidic acid (Fucidin) should not be given with statins because of a risk of serious and potentially fatal rhabdomyolysis. Healthcare professionals should be aware of strengthened warnings regarding this potential drug interaction.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON128951
MHRA Drug Safety Update Tigecycline: increased mortality in clinical trials - use only when other antibiotics are unsuitable
Article date: April 2011 Summary An analysis of pooled results from clinical trials of tigecycline (Tygacil▼) versus comparator drugs in a range of infections has shown numerically higher mortality rates in patients receiving tigecycline. Therefore, doctors are advised to use tigecycline only when other antibiotics are unsuitable.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON111761
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 1 of 13 Date: 15.1.2014 Drug Formulary MHRA Drug Safety Update Daptomycin: risk of eosinophilic pneumonia
Article date: February 2011 Summary There have been rare but potentially serious reports of eosinophilic pneumonia associated with daptomycin (Cubicin▼). If eosinophilic pneumonia is suspected, daptomycin should be discontinued immediately and if appropriate the patient treated with corticosteroids. Daptomycin should not be readministered to patients who have experienced eosinophilic pneumonia with this drug.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON108678
MHRA Drug Safety Update Moxifloxacin: use in pelvic inflammatory disease only when other antibacterials are inappropriate or ineffective- use only when other antibiotics are unsuitable
Article date: January 2011 Summary Because of evidence of an increased risk of life-threatening liver reactions and other serious risks (such as QT interval prolongation), oral moxifloxacin (Avelox ▼, a fluoroquinolone antibiotic) should be used only when it is considered inappropriate to use antibacterial agents that are commonly recommended for the initial treatment of the infections below or when these have failed.This restriction now applies to treatment of mild to moderate pelvic inflammatory disease as well as treatment of acute bacterial sinusitis, acute exacerbations of chronic bronchitis, and community acquired pneumonia (except severe cases).Consideration should be given to official guidance on the appropriate use of antibacterial agents.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON105760
MHRA Drug Safety Update Carbapenems: concomitant use with valproic acid not recommended
Article date: May 2010 Summary A clinically significant interaction between carbapenems and valproic acid results in reduced valproate plasma concentrations with potential for inadequate seizure control. Concomitant use of these agents is not recommended, and healthcare professionals should consider alternative antibacterial therapy.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON085143
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 2 of 13 Date: 15.1.2014 Drug Formulary MHRA Drug Safety Update Ceftriaxone: incompatibility with calcium containing solutions – updated advice
Article date: October 2009 Summary Ceftriaxone should not be given simultaneously with calcium-containing solutions (other than total parenteral nutrition solutions) for intravenous administration because of a risk of calcium precipitation. Ceftriaxone is contraindicated in newborns up to age 28 days who need intravenous treatment with any calcium-containing solution. Calcium and ceftriaxone may be infused sequentially in patients aged 28 days or older provided that either a) the infusion line is rinsed or flushed between solutions, or b) the infusions are given via different infusion lines at different sites.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON087671
MHRA Drug Safety Update Moxifloxacin: restricted use
Article date: August 2008 Summary Oral moxifloxacin (Avelox ▼, a fluoroquinolone antibiotic) is now restricted for use only when other medicines cannot be prescribed, or have failed, for treatment of acute bacterial sinusitis, acute exacerbation of chronic bronchitis, or community-acquired pneumonia. This restriction is based on evidence of an increased risk of life-threatening liver reactions and other serious risks associated with moxifloxacin. Please prescribe oral moxifloxacin according to this updated information, while also considering official guidance on appropriate use of antibiotics and prevalence of resistance.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON087781
MHRA Drug Safety Update Nitrofurantoin: reminder on precautions for use, especially renal impairment in (elderly) patients
Article date: August 2013 Summary Use of nitrofurantoin for urinary tract infections is contraindicated in patients with <60 mL/min creatinine clearance. Healthcare professionals should be aware of a patient’s current renal function when prescribing, especially for elderly patients.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON3000402
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 3 of 13 Date: 15.1.2014 Drug Formulary MHRA Drug Safety Update Oral ketoconazole: do not prescribe or use for fungal infections – risk of liver injury outweighs benefits
Article date: August 2013 Summary Doctors should no longer prescribe oral ketoconazole for fungal infections, and should review patients’ treatment options because of a risk of liver injury. The European Medicines Agency’s Committee on Medicinal Products for Human Use (CHMP) concluded that although liver injury such as hepatitis is a known side effect of antifungal medicines, the incidence and the seriousness are higher with oral ketoconazole than with other antifungals.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON300403
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 4 of 13 Date: 15.1.2014 Drug Formulary 5.1 Antibacterial drugs Penicillins Benzylpenicillin 600mg injection
Co-flumampicil 125/125 suspension
Co-flumampicil 250/250 injection
Phenoxymethylpenicillin 250mg tablets
Phenoxymethylpenicillin 125mg/5ml, 250mg/5ml syrup
Flucloxacillin 250mg, 500mg injection
Flucloxacillin 250mg, 500mg capsules
Flucloxacillin 125mg/5ml, 250mg/5ml syrup
Amoxycillin 250mg, 500mg, 1g injection
Amoxycillin 250mg, 500mg capsules
Amoxycillin 125mg/5ml, 250mg/5ml syrup
Amoxycillin 3g sachet
Co-amoxiclav 1.2g injection
Co-amoxiclav 250/125 tablets and 500/125 tablets
Co-amoxiclav 125/31, 250/62 suspension
Co-amoxiclav 400/57 (Augmentin Duo) suspension - Paediatric use in cystic fibrosis ONLY
Cephalosporins, cephamycins and other beta-lactams Cefotaxime 1g injection – ALERT ANTIMICROBIAL – consult microbiology
Ceftazidime 500mg,1g, 2g injection– ALERT ANTIMICROBIAL – consult microbiology
Cefuroxime 250mg and 750mg injection
Cefalexin 250mg, 500mg capsules
Cefalexin 125mg/5ml, 250mg/5ml syrup
Ceftriaxone 250mg, 1g and 2g injection– ALERT ANTIMICROBIAL – consult microbiology
Aztreonam 1g, 2g injection– ALERT ANTIMICROBIAL – consult microbiology
Meropenem 500mg, 1g injection– ALERT ANTIMICROBIAL – consult microbiology
Ertapenem 1g injection– ALERT ANTIMICROBIAL – consult microbiology
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 5 of 13 Date: 15.1.2014 Drug Formulary Tetracyclines Tetracycline 250mg tablets
Demeclocycline 150mg capsules
Doxycycline 50mg, 100mg capsules, 100mg disp. tablets
Aminoglycosides Gentamicin 20mg/2ml, 80mg/2ml injection– ALERT ANTIMICROBIAL – consult microbiology
Neomycin 500mg tablets
Macrolides Erythromycin 250mg, 500mg tablets
Erythromycin 1g injection
Erythromycin 125mg/5ml, 250mg/5ml syrup
Azithromycin 250mg capsules
Azithromycin 200mg/5ml suspension
Clarithromycin 500mg injection
Clarithromycin 250mg tablets
Clarithromycin 125mg/5ml, 250mg/5ml suspension
Other antibiotics Benzathine benzylpenicillin 1.8g (2.4 million unit) injection
Chloramphenicol 1g injection– ALERT ANTIMICROBIAL – consult microbiology
Chloramphenicol 250mg capsules– ALERT ANTIMICROBIAL – consult microbiology
Ciprofloxacin 200mg ,400mg injection– ALERT ANTIMICROBIAL – consult microbiology
Ciprofloxacin 250mg tablets– ALERT ANTIMICROBIAL – consult microbiology
Ciprofloxacin 250mg/5ml suspension– ALERT ANTIMICROBIAL – consult microbiology
Clindamycin 150mg capsules– ALERT ANTIMICROBIAL – consult microbiology
Clindamycin 600mg/4ml injection– ALERT ANTIMICROBIAL – consult microbiology
Clindamycin 75mg/5ml suspension– ALERT ANTIMICROBIAL – consult microbiology
Colistin 1 million unit per vial– ALERT ANTIMICROBIAL – consult microbiology
Co-trimoxazole 240mg/5ml and 480mg/5ml suspension
Co-trimoxazole 400/80 tablets
Co-trimoxazole 480mg/5ml injection– ALERT ANTIMICROBIAL – consult microbiology
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 6 of 13 Date: 15.1.2014 Drug Formulary Daptomycin 350mg and 500mg injection – ALERT ANTIMICROBIAL – consult microbiology
Fidaxomicin 200mg tablets – ALERT ANTIMICROBIAL – consult microbiology
Fosfomycin 3g sachet – ALERT ANTIMICROBIAL – consult microbiology
Linezolid 100mg/5ml suspension– ALERT ANTIMICROBIAL – consult microbiology
Linezolid 600mg tablets– ALERT ANTIMICROBIAL – consult microbiology
Linezolid 600mg/300ml infusion– ALERT ANTIMICROBIAL – consult microbiology
Metronidazole 200mg, 400mg tablets
Metronidazole 200mg/5ml suspension
Metronidazole 500mg in 100ml infusion
Metronidazole 500mg, 1g suppositories
Moxifloxacin 400mg tablets– ALERT ANTIMICROBIAL – consult microbiology
Nitrofurantoin 25mg/5ml suspension
Nitrofurantoin 50mg, 100mg capsules
Nitrofurantoin 50mg,100mg tablets
Piperacillin 4g/Tazobactam 500mg injection – ALERT ANTIMICROBIAL – consult microbiology
Pivmecillinam 200mg tablets
Rifaximin 550mg tablets – for use in hepatic encephalopathy by consultant gastroenterologist only
Sodium fusidate 250mg tablets
Sodium fusidate 250mg/5ml suspension
Sodium fusidate 500mg intravenous infusion
Teicoplanin 200mg and 400mg injection– ALERT ANTIMICROBIAL – consult microbiology
Tigecycline 50mg injection – ALERT ANTIMICROBIAL – consult microbiology
Trimethoprim 200mg tablets
Trimethoprim 50mg/5ml suspension
Vancomycin 125mg capsules– ALERT ANTIMICROBIAL – consult microbiology
Vancomycin 500mg injection– ALERT ANTIMICROBIAL – consult microbiology
Prescribing notes
The following advice from the Antimicrobial Management Committee can be found under of the Antimicrobials section of the Trust Medicines Info Intranet site: . Adult Antimicrobial Guidelines for Secondary Care . Guidance No 1: IV to Oral Switch . Guidelines on Colomycin Administration by Nebuliser
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 7 of 13 Date: 15.1.2014 Drug Formulary . Body Mass Index Ready Reckoner . Adult Once Daily Gentamicin Guidelines . Management of Patients with Fever and Neutropenia
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 8 of 13 Date: 15.1.2014 Drug Formulary Antituberculosis drugs Ethambutol 100mg, 400mg tablets
Isoniazid 50mg, 100mg tablets
Isoniazid 50mg/5ml elixir
Pyrazinamide 500mg tablets
Rifampicin 150mg, 300mg capsules
Rifampicin 100mg/5ml syrup
Rifampicin 600mg injection
Rifinah 150 tablets (Rifampicin 150mg, isoniazid 100mg)
Rifinah 300 tablets (Rifampicin 300mg, isoniazid 150mg)
Rifater (Rifampicin 120mg, isoniazid 50mg, pyrazinamide 300mg)
Prescribing notes
Consult BNF for recommended treatment regimens and dosing from the Joint Tuberculosis Committee of the British Thoracic Society guidelines for the treatment of tuberculosis in the UK.
Streptomycin should not be given in pregnancy.
Isoniazid, rifampicin and pyrazinamide are associated with liver toxicity so hepatic function should be checked before treatment with these drugs. Further checks are only necessary if the patient develops fever, malaise, vomiting, jaundice or unexplained deterioration during treatment.
Visual acuity should be tested before ethambutol is used The earliest features of ocular toxicity are subjective and patients should be advised to discontinue therapy immediately if they develop deterioration in vision and promptly seek further advice.
Renal function should be checked before treatment with antituberculous drugs and appropriate dosage adjustments made. Streptomycin or ethambutol should preferably be avoided in patients with renal impairment, but if used, the dose should be reduced and the plasma-drug concentration monitored.
Rifampicin induces hepatic enzymes which accelerate the metabolism of several drugs including oestrogens, corticosteroids, phenytoin, sulphonylureas, and anticoagulants. (N.B. the effectiveness of hormonal contraceptives is reduced and alternative family planning advice should be offered)
Monthly tablet counts and urine examination (rifampicin imparts an orange-red coloration) may be useful indicators of compliance with treatment.
Drug-resistant tuberculosis should be treated by a specialist physician.
Antileprotic drugs Dapsone 50mg tablets
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 9 of 13 Date: 15.1.2014 Drug Formulary 5.2 Antifungal drugs
Anidulafungin 100mg injection – ALERT ANTIMICROBIAL – consult microbiology
Caspofungin 50mg and 70mg injection – ALERT ANTIMICROBIAL – consult microbiology
Fluconazole 50mg, 150mg, 200mg capsules
Fluconazole 200mg/100ml injection
Fluconazole 50mg/5ml suspension
Griseofulvin 125mg, 500mg tablets
Itraconazole 100mg capsules
Itraconazole 50mg/5ml SF liquid
Nystatin 100,000 units/ml suspension
Posaconazole 200mg/5ml suspension – ALERT ANTIMICROBIAL – consult microbiology
Terbinafine 250mg tablets
Voriconazole 200mg injection – ALERT ANTIMICROBIAL – consult microbiology
Voriconazole 200mg tablets – ALERT ANTIMICROBIAL – consult microbiology
Voriconazole 200mg/5ml suspension – ALERT ANTIMICROBIAL – consult microbiology
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 10 of 13 Date: 15.1.2014 Drug Formulary 5.3 Antiviral drugs
Aciclovir 200mg, 400mg tablets
Aciclovir 200mg/5ml suspension
Aciclovir 250mg, 500mg injection – ALERT ANTIMICROBIAL – consult microbiology
Palivizumab 50mg, 100mg injection
Oseltamivir 30mg, 45mg and 75mg capsules
Oseltamivir 30mg/5ml suspension
Boceprevir 200mg capsules
Telaprevir 375mg tablets
Ribavirin 200mg, 400mg tablets (Copegus®)
Peginterferon alfa-2a 135microgram/0.5ml, 180microgram/0.5ml injection (Pegasys®)
Prescribing notes – Human Immunodeficiency Virus
Seek specialist advice from the Department Of Infectious Diseases and Tropical Medicine at Newcastle General Hospital.
Antiretroviral therapy following an inoculation injury (post-exposure prophylaxis or PEP) if indicated should be commenced if possible within 2 hours and at the latest 48 hours after injury. In the event of an inoculation injury follow the Trust Policy and contact Occupational Health Service.
Prescribing notes - Influenza
Annual vaccination is essential for all those in 'at-risk' groups.
For otherwise healthy adults the use of antivirals is not recommended.
Antiviral drugs may be prescribed for the prophylaxis and treatment of influenza in 'at-risk' groups when influenza A or influenza B is circulating in the community on the advice of the Department of Health.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 11 of 13 Date: 15.1.2014 Drug Formulary 5.4 Antiprotozoal drugs
Tinidazole 500mg tablets Treatment of Giardiasis
Chloroquine 200mg tablets
Quinine dihydrochloride 300mg/ml injection – ALERT ANTIMICROBIAL – consult microbiology
Quinine sulphate 200mg, 300mg tablets
Prescribing notes
Treatment of malaria
Seek specialist advice from the Department Of Infectious Diseases and Tropical Medicine at Newcastle General Hospital.
Quinine is very toxic in overdose in such cases immediate advice should be sought from UK National Poisons Information Service.
IV administration of Quinine requires monitoring of blood glucose, electrolytes and ECG.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 12 of 13 Date: 15.1.2014 Drug Formulary 5.5 Anthelmintics Drugs for threadworms Mebendazole 100mg tablets
Mebendazole 100mg/5ml suspension
Pripsen sachets
Prescribing notes Threadworms Anthelmintics should be used in combination with hygienic measures to break the cycle of auto-infection. All members of the family should be treated.
One dose of mebendazole is usually sufficient for treatment of threadworms.
Mebendazole is not licensed for children under 2 years; piperazine salts are less effective but licensed for this age group.
Mebendazole and piperazine are available over-the-counter.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green+ are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 13 of 13 Date: 15.1.2014 Drug Formulary