Male Reproductive System
All living things, including humans, reproduce; it's one of the things that set us apart from nonliving matter. And because all living things eventually die, new creatures of the same kind must constantly be born to perpetuate a particular species. Interestingly, although the reproductive system is essential to keeping a species alive, unlike other body systems, it is not essential to keeping an individual being alive.
In the reproductive process, two kinds of sex cells, or gametes, are involved. The male gamete, or sperm, and the female gamete, the egg or ovum, meet in the female's reproductive system to create a new individual.
How Is the Male Reproductive System Important for Living? The male reproductive system is essential to the perpetuation of life: the female is dependent on the male for fertilization of her egg, even though it is she who carries the offspring through pregnancy and childbirth.
Testosterone, the hormone that allows boys to become mature men, is produced by the male reproductive system. Without it, men wouldn't be able to make sperm, and reproduction would be impossible.
Basic Anatomy Most species have male and female organisms. Each sex has its own unique reproductive system. They are different in shape and structure, but both produce, nourish, and transport either the egg or sperm.
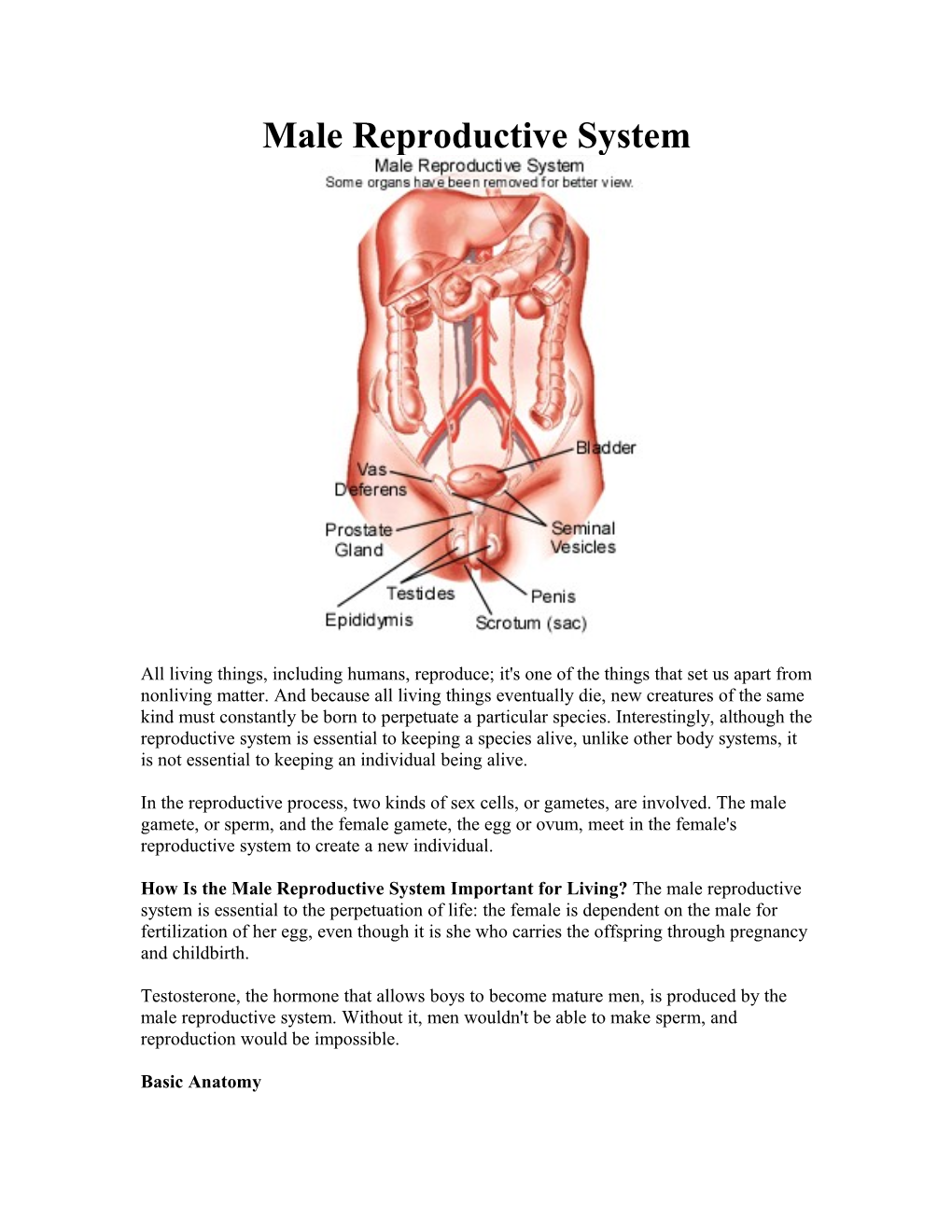
Unlike its female counterpart, whose sex organs are inside the body, the male reproductive system includes sex organs, or genitals, that are situated both inside and outside the body. These are the testicles; duct system, including the epididymis and vas deferens; accessory glands; and penis. The two testicles, or testes, produce and store the tiny sperm cells. The counterpart of the ovaries in the female, the testicles are oval shaped and grow to be about 1 inch long. The testicles also produce hormones, including testosterone, which stimulates the production of sperm and facilitates male maturation.
The duct system includes the epididymis and the vas deferens, a muscular tube that passes upward alongside the testes and transports the sperm-containing fluid called semen. Each epididymis is a set of coiled tubes that lies against the testes, connecting them with the vas deferens. With the testes, they hang in a pouchlike structure behind the penis called the scrotum.
The accessory glands, including the seminal vesicles and the prostate gland, provide fluids that lubricate the duct system and nourish the sperm. The seminal vesicles are saclike structures attached to the vas deferens to the side of the bladder. The prostate gland, which produces some of the components of semen, surrounds the ejaculatory ducts at the base of the urethra, just below the bladder. The urethra carries the semen through the penis, a cylindrical structure located between the legs, to the outside. The urethra also discharges urine, which is filtered in the kidneys and stored in the bladder.
Normal PhysiologyThe male sex organs work together to produce semen and to release the sperm into the reproductive system of the female during sexual intercourse. They also produce and secrete sex hormones.
During puberty, sex hormones help a male to develop into a sexually mature man. At this time, usually between the ages of 9 and 14, the pituitary gland secretes hormones that stimulate the testicles to produce testosterone, which is responsible for bringing about a series of sexual changes. These changes may occur at different rates but generally follow a set sequence.
The first stage of sexual maturation involves the growth of the scrotum and testes. Next, the penis becomes longer, and the seminal vesicles and prostate gland grow. Hair begins to appear in the pubic area, and about 2 years later, it grows on the face and underarms. The voice deepens, and males may experience their first ejaculation. Most males will also undergo a growth spurt during adolescence, reaching their adult height and weight. The onset of sexual maturation may be delayed or brought on earlier by certain genetic abnormalities or illnesses. An adult male produces several million sperm cells every day. Sperm develop in the testicles within a system of tubes called seminiferous tubules. When a male baby is born, his tubules contain simple round cells, but during puberty testosterone and other hormones cause these cells to divide and change until they are thin, with a head and short tail, like tadpoles. The head contains genetic material (genes). The sperm use their tails to propel themselves into the epididymis, where they complete their development.
The sperm then move to the vas deferens, or sperm duct. The seminal vesicles and prostate gland produce a whitish fluid called seminal fluid, which mixes with sperm to form semen as a result of sexual stimulation. The penis, which usually hangs limp, becomes hard when a male is sexually excited. Tissues in the penis fill with blood and it becomes stiff and erect. When the erect penis is stimulated, muscles around the reproductive organs contract and force the semen through the duct system and urethra. Semen is expelled from the body through the urethra inside the penis. This process is called ejaculation. Each milliliter of semen contains about 100 million sperm.
The rigidity of the erect penis aids its insertion into the female's vagina during sexual intercourse. When the male ejaculates, semen is deposited into the female's vagina. The sperm make their way up to the uterus with help from uterine contractions. If a mature egg is in one of the fallopian tubes, a single sperm may penetrate it, and fertilization or conception occurs.
The cell is now a zygote, containing its full quota of 46 chromosomes, half from the egg, and half from the sperm. The cell divides again and again as it grows in the female's uterus. The genetic material from the male and female has combined to create a new individual.
Diseases, Disorders, Conditions, and DysfunctionsSome of the more common diseases and conditions affecting the male reproductive system include the following:
Disorders of the Scrotal ContentsConditions affecting the scrotal contents may involve the testicles, epididymis, or the scrotum itself.
Testicular Disorders
* Testicular trauma. Even the slightest injury to the testicles can cause severe pain, bruising, or swelling. Most testicular injuries occur when the testicles are struck, hit, kicked, or crushed, usually during sports. To protect their testicles from trauma, boys and men should always wear athletic cups during contact sports. * Testicular torsion. This testicular problem occurs most frequently in males between the ages of 12 and 18. Within the scrotum, the testicles are secured by a structure called the spermatic cord. When the testicle twists on this cord, the blood supply to the testicle is cut off. Torsion might occur as the result of trauma to the testicles, strenuous activity, or for no apparent reason at all. In the United States, testicular torsion occurs in one out of 4,000 males younger than 25. * Undescended testicles. A male baby may be born with his testicles not having descended into the scrotum. The testes form in the abdominal cavity in the early stages of fetal development, and then descend in the month before birth. If the testicles do not drop by themselves, surgery can bring them down. * Testicular cancer. Although rare, this is one of the most common cancers in men younger than 40. It occurs when cells in the testicle divide and form a tumor. If detected early, the cure rate is excellent. Lance Armstrong, champion U.S. cyclist, survived testicular cancer that was not detected early and had spread to his abdomen, lungs, and brain. Teens should be encouraged to perform self-examinations, because early detection of testicular cancer can be life-saving. * Epididymitis is inflammation of the epididymis, the coiled tubes that connect the testes with the vas deferens. It is usually caused by infection or by the sexually transmitted disease chlamydia, and results in pain and swelling at the back of one testicle. * Hydrocele. A hydrocele - fluid in the membranes surrounding the testes - may be present at birth or may develop later in life. Hydroceles may cause swelling of the testicle but are generally painless. If a large amount of fluid is present, a doctor may need to draw it out with a needle. * Inguinal hernias. When a portion of the intestines pushes through the abdominal wall and into the groin or scrotum, it is known as an inguinal hernia. The hernia is apparent as a bulge or swelling in the groin area. It can be corrected with surgery.
Penile Disorders Disorders affecting the penis include the following:
* Hypospadias, a birth defect in which the opening of the urethra is in the wrong place, such as the underside of the penis. Surgery can correct it. * Phimosis, a tightening of the foreskin of the penis, which is common in newborns and young children and usually resolves without treatment. If it interferes with urination, circumcision may be recommended. * Ambiguous genitalia, a very rare condition in which a child is born with genitals that aren't clearly male or female. In most boys born with this disorder, the penis may be very small or nonexistent but testicular tissue is present. In a small number of cases, the child may have both testicular and ovarian tissue. * Micropenis, another rare disorder where the penis, although normally formed, falls well below the average size, as determined by standard measurements.
CircumcisionAlthough circumcision is not a penile disorder or dysfunction, it is something that parents of newborn boys may find themselves thinking a lot about. Usually performed during the first few days of life, circumcision is a procedure in which the foreskin is surgically removed, exposing the end of the penis. Parents who choose circumcision often do so based on religious beliefs, concerns about hygiene, or cultural or social reasons.
Sterility/InfertilityIf a male is sterile, either his body doesn't produce sperm at all or it doesn't produce enough sperm. This may occur as a result of abnormalities of the reproductive organs, inflammation in the genitals, alcoholism, or diseases.