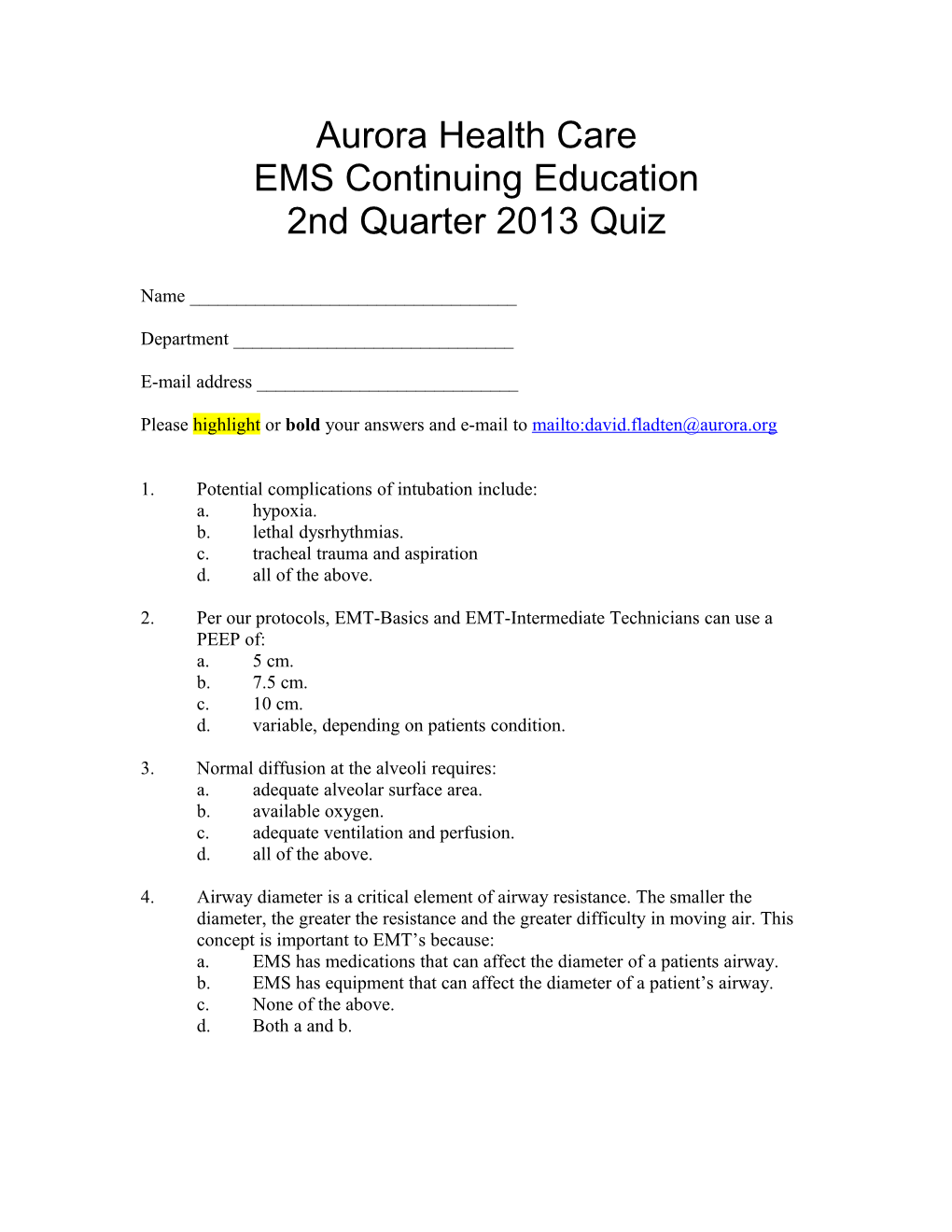
Aurora Health Care EMS Continuing Education 2nd Quarter 2013 Quiz
Name ______
Department ______
E-mail address ______
Please highlight or bold your answers and e-mail to mailto:[email protected]
1. Potential complications of intubation include: a. hypoxia. b. lethal dysrhythmias. c. tracheal trauma and aspiration d. all of the above.
2. Per our protocols, EMT-Basics and EMT-Intermediate Technicians can use a PEEP of: a. 5 cm. b. 7.5 cm. c. 10 cm. d. variable, depending on patients condition.
3. Normal diffusion at the alveoli requires: a. adequate alveolar surface area. b. available oxygen. c. adequate ventilation and perfusion. d. all of the above.
4. Airway diameter is a critical element of airway resistance. The smaller the diameter, the greater the resistance and the greater difficulty in moving air. This concept is important to EMT’s because: a. EMS has medications that can affect the diameter of a patients airway. b. EMS has equipment that can affect the diameter of a patient’s airway. c. None of the above. d. Both a and b. 5. Increased work of breathing is an important sign of respiratory distress. EMT’s must look for signs and symptoms of increased work of breathing in their patient assessment. Signs of increased work of breathing include: a. tripod positioning by the patient. b. use of accessory muscles. c. presence of retractions. d. all of the above.
6. Pulmonary edema due to an underlying cardiac problem is usually related to: a. failing right atrium. b. failing right ventricle. c. failing left atrium. d. failing left ventricle.
7. CPAP is effective for patients with pulmonary edema because it: a. reinflates collapsed alveoli. b. increases oxygen availability at the alveolar membrane. c. forces fluid out of the interstitial space and back into blood vessels. d. all of the above.
8. CPAP is effective for patients suffering from COPD exacerbation because it: a. reinflates collapsed alveoli. b. can “pop” open bronchioles obstructed by mucus secretions. c. aids in getting nebulized medications where they need to be in order to be effective. d. all of the above.
9. CPAP works by: a. decreasing inspiratory and expiratory pressures to below atmospheric pressures. b. decreasing inspiratory pressures below atmospheric pressure and raising expiratory pressures to above atmospheric pressures. c. increasing inspiratory pressure above atmospheric pressure and applying PEEP during expiration. d. none of the above.
10. Hypercarbia is a condition in which there is an increase in CO2 levels in the blood. This frequently results from inadequate elimination of CO2 from the lungs. This is important to EMS because: a. a primary cause is respiratory depression and hypoventilation. b. EMS has no method to detect CO2 levels. c. the primary cause is hyperventilation. d. CPAP will have no effect on this condition. 11. CPAP is appropriate for patients who: a. are in mild, moderate or severe respiratory distress. b. are not breathing. c. have an altered mental status or are unresponsive. d. are vomiting as it will protect their airway.
12. Once CPAP has been attached to the patient, nebulized medications or sublingual medications such as nitroglycerine can still be administered. a. true. b. false.
13. Pneumothorax is a complication risk associated with application of CPAP. This is a concern for EMS as undetected, the pneumothorax can quickly develop into a tension pneumothorax. Based upon that risk, CPAP : a. is appropriate for a patient with chest trauma and suspected pneumothorax. b. should be considered for chest trauma patients as long as lung sounds are auscultated. c. should ONLY be applied after a COMPLETE respiratory assessment is performed even if a pneumothorax is suspected. d. should NEVER be applied to a patient with a suspected pneumothorax regardless of whether it is from a medical or traumatic condition.
14. CPAP is appropriate for patients who have respiratory distress due to: a. asthma or COPD. b. pneumonia. c. pulmonary edema. d. all of the above.
Per our protocols, please select appropriate indications for the use of CPAP. Place an X next to an appropriate indication.
_____ Patient awake _____ Patient with an altered mental status _____ Systolic blood pressure greater than 100 mm Hg _____ Unresponsive patient _____ Apnea _____ Patient over 12 years of age and able to fit mask _____ Respiratory rate greater than 25 _____ Increased work of breathing _____ sPO2 less than 94% and not relieved by other interventions _____ Patient able to maintain patent (open) airway _____ Poor respiratory drive _____ Mild to severe respiratory distress