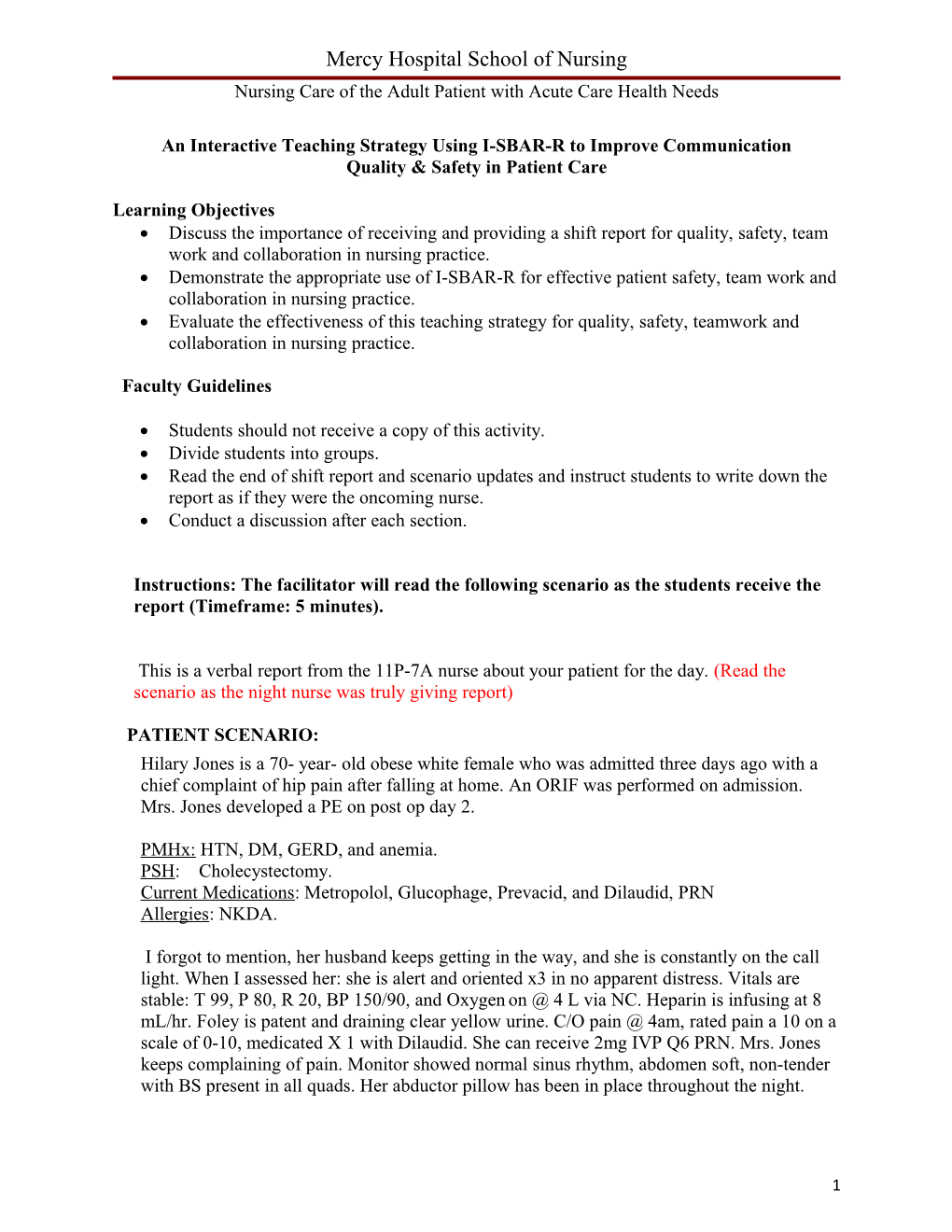
Mercy Hospital School of Nursing Nursing Care of the Adult Patient with Acute Care Health Needs
An Interactive Teaching Strategy Using I-SBAR-R to Improve Communication Quality & Safety in Patient Care
Learning Objectives Discuss the importance of receiving and providing a shift report for quality, safety, team work and collaboration in nursing practice. Demonstrate the appropriate use of I-SBAR-R for effective patient safety, team work and collaboration in nursing practice. Evaluate the effectiveness of this teaching strategy for quality, safety, teamwork and collaboration in nursing practice.
Faculty Guidelines
Students should not receive a copy of this activity. Divide students into groups. Read the end of shift report and scenario updates and instruct students to write down the report as if they were the oncoming nurse. Conduct a discussion after each section.
Instructions: The facilitator will read the following scenario as the students receive the report (Timeframe: 5 minutes).
This is a verbal report from the 11P-7A nurse about your patient for the day. (Read the scenario as the night nurse was truly giving report)
PATIENT SCENARIO: Hilary Jones is a 70- year- old obese white female who was admitted three days ago with a chief complaint of hip pain after falling at home. An ORIF was performed on admission. Mrs. Jones developed a PE on post op day 2.
PMHx: HTN, DM, GERD, and anemia. PSH: Cholecystectomy. Current Medications: Metropolol, Glucophage, Prevacid, and Dilaudid, PRN Allergies: NKDA.
I forgot to mention, her husband keeps getting in the way, and she is constantly on the call light. When I assessed her: she is alert and oriented x3 in no apparent distress. Vitals are stable: T 99, P 80, R 20, BP 150/90, and Oxygen on @ 4 L via NC. Heparin is infusing at 8 mL/hr. Foley is patent and draining clear yellow urine. C/O pain @ 4am, rated pain a 10 on a scale of 0-10, medicated X 1 with Dilaudid. She can receive 2mg IVP Q6 PRN. Mrs. Jones keeps complaining of pain. Monitor showed normal sinus rhythm, abdomen soft, non-tender with BS present in all quads. Her abductor pillow has been in place throughout the night.
1 Mercy Hospital School of Nursing Nursing Care of the Adult Patient with Acute Care Health Needs
SECTION I:
Instructions: The facilitator should ask the following questions followed by a student discussion. (Timeframe: 15 minutes)
1. What important data was omitted from the night shift nurse in the report? What other information should have been provided by the night nurse to give quality and safe patient care?
a. Heparin: What dose? Only 8mL/hr was reported by the RN When was last PTT drawn What are the trends of PTTs (stable on that dose or need of adjusting). When is next PTT due? b. Pain: Complete a pain assessment? What other techniques could be used to relieve pain? Complete a pain reassessment? c. Pulse Ox: What is her saturation? Patient is on oxygen. d. Breathing: Need more data on breathing – breath sounds e. Neurovascular Are pulses palpable in extremity? Is circulation adequate? Is the patient moving the extremity? f. Foley: Quantity? Adequate amounts? g. Abdomen: Last bowel movement h. Surgical Site: Dressing information? Staples, drainage, etc. i. Labs: What other labs need to be in report (CBC, H&H, PT, BGM) Is patient on Coumadin? j. Code Status Is there a code status? k. Nutrition: Type of diet and fluid intake l. IV Fluids Does she have IV fluids?
2 Mercy Hospital School of Nursing Nursing Care of the Adult Patient with Acute Care Health Needs
2. What was inappropriate about the night RN’s report?
Comments about patient and the husband Perhaps there was a reason the patient was on the call light all night. Perhaps she was afraid? What did the nurse do when she saw the patient? Was she therapeutic? Could she have just sat with the patient, offered support, held her hand, answered her questions?
3. What can you do to change behaviors like this on your nursing units?
Do not feed into negative behaviors Try to redirect the RN to continue with the important information: Change the subject. Be a role model. Learn to give excellent, concise, non-biased, factual, professional report.
Section II:
Instructions: The facilitator will read the following scenario as the students write down the updates followed by a discussion of the two questions below. (Timeframe: 20 minutes).
It is 8:00 AM, the night nurse has left, and you enter the patient’s room – as she has pressed the call light again. After you wash your hands and introduce yourself, Mrs. Jones exclaims that she has “been in pain all night with her hip.”, and further states, “What is wrong with this place?” “Why do I have to suffer with this constant pain?”
1. What would be your immediate actions as the RN?
Acknowledge patient’s comment and provide a therapeutic response Complete a full pain assessment and obtain vital signs Complete a wound assessment to ensure nothing is wrong. Call health care provider for a change in pain medication order because current order is not helping with pain.
3 Mercy Hospital School of Nursing Nursing Care of the Adult Patient with Acute Care Health Needs
2. Write the information that you would provide to the health care provider, in the ISBAR format) based on the information you were just given (Give the groups five minutes to complete and then have them read the report) (Students verbally present their I-SBAR- R to group)
Introduction: “Hello, my name is ______, I am the RN from 14 Tower and I am caring for Hilary Jones in room 16
Situation: Mrs. Jones has been complaining of pain throughout the night. She was medicated at 4 am with 2 mg of Dilaudid for hip pain 10/10, and one hour later her pain was still at 8/10. The current order is Dilaudid 2 mg IV every 6 hours PRN for pain.
Background : Mrs. Jones 70- year- old, white female status post ORIF of the right hip three day ago, status post fall at home. She developed a PE on post op day two. She is on a Heparin infusion. She has NKDA.
Assessment: Her VS are ______(stable) & wound is _____. Mrs. Jones rates her pain a 10/10 with a sharp quality. She is refusing to go to physical therapy. Pedal pulses are palpable (Students provide VS and wound assessment data – gives students opportunity to critically think about VS and learning to describe a wound – (normal versus abnormal)
Recommendation: Could the Dilaudid dose and/ or time frames be changed? Every 4 hours?
MD Order: Please increase Dilaudid dose to 4 mg IV every 4 hours, PRN pain
Read back: Dilaudid dose to 4 mg IV every 4 hours, PRN pain
Facilitator provides the following instruction The physician increased the Dilaudid dose to 4 mg IVP Q4 hours PRN pain.
4 Mercy Hospital School of Nursing Nursing Care of the Adult Patient with Acute Care Health Needs
PATIENT SCENARIO CONTINUES: (Faculty to read)
It is 10:00 AM. You administered Mrs. Jones the new Dilaudid dose of 4mg at 8:00 AM. Her pain has been reduced to a 6/10. You got her a crossword puzzle from the volunteer’s cart and told her that you spoke to her physician and he has increased her pain medications from 2 mg to 4 mg. You offer her a backrub and a fresh pillowcase. She tears up and says, “Thank you so much for caring, I was so afraid that I was going to die from this pain that I just couldn’t sleep last night.”
It is 12:00 PM, and Mrs. Jones wants her pain medication. She is still a 6/10. She is resting 30 minutes after receiving the medication. She opens her eyes for one moment and whispers to you, “I’m finally at a 3/10 and I am going to take a long nap. “God bless you.”
At 1:00 PM; you receive the following lab values.
VALUE LAB NORMAL VALUE PTT 35 sec (25-35) PT 12 sec (12-15) BUN 15 (5-25) Creat 1.0 (0.5-1.5) Sodium 138 (135-145) Potassium 3.7 (3.5-5) Glucose 120 (70-100) Ca 9.0 (8.5-10) Hgb 9.0 (13.5-17) Hct 28 (40-54)
SECTION III
Instructions: The facilitator will encourage discussion of the questions.
1. Which lab(s) value(s) is/are critical?
H/H Once they figure this out, tell them that ‘they looked in the chart and found that her previous H/H results were: 2200 - 10.1 and 30, and yesterdays at 10:00 AM - 11.3 and 32. Students need to report the H and H to the ordering physician.
Discuss therapeutic range for PTT, PT and Glucose
Discuss why the blood glucose is elevated
5 Mercy Hospital School of Nursing Nursing Care of the Adult Patient with Acute Care Health Needs Instructions: The facilitator will instruct the groups to write what they would say to the health care provider using the I-SBAR-R format. (Give the groups five minutes to complete and then have them read the report)
1. Write the information that you would provide to the health care provider. (Students present their I-SBAR- R to group).
Introduction: “Hello, my name is ______, I am an RN, and I am calling from 14 Tower. I am caring for Hilary Jones in room 16.
Situation: I am calling regarding Mrs. Jones lab work. Her H/H from 10 am was 9.0 and 28. Her H/H from 2200 was 10.1 and 30.
Background : Mrs. Jones is a 70-year-.old. who had an ORIF of the right hip three day ago, s/p fall at home - and developed a PE on post op day two. She is on a Heparin infusion.
Assessment: “Her VS are ______& wound assessment reveals ______. Her H/H are being drawn BID at 10 and 10. She has a PMHx of Anemia (Students provide VS and wound data – gives students opportunity to critically think about VS and describing a wound – (normal versus abnormal)
Recommendation: Would you want a T&C? Transfuse? Do you want to increase frequency of labs to q4-6 hours? Should we repeat the lab – these are some of the options
Instructions: Facilitator provides the following information.
The physician ordered a T&C, increased H/H to Q4hrs, and started patient on Ferrous Sulfate, 325mg PO TID with meals. (Faculty to read)
SECTION IV
Instructions: Facilitator will have students write an end of shift report and practice giving report to another student using I-SBAR-R. (Timeframe 30 minutes)
Give them time to write their report. When students complete shift report, have them break into groups of 2. One student will give report, the other student will receive report Encourage the ‘receiver’ to ask questions. Give time for the students to finish ‘report” Ask for a student volunteer to read their end of shift report.
6 Mercy Hospital School of Nursing Nursing Care of the Adult Patient with Acute Care Health Needs Example of a student report: (For Facilitator use only). Situation:
Hilary Jones is a 70 year-.old, obese white female, whom was admitted four days ago after falling at home. In the ER, X-rays revealed a fractured right hip and the patient had an ORIF that day. On Post-op day 2, Mrs. Jones had an increased heart rate and fever. A spiral CT scan was done which revealed a PE. She was started on a Heparin IV infusion at 1300 units/hour, after receiving a 1000 unit IV bolus.
Background:
Mrs. Jones has a PMHx of HTN, DM, GERD, and anemia with past surgical history of a Cholecystectomy in 2002. Her medications at home include Metropolol, Glucophage, and Prevacid which the doctors ordered for her to take here, and she has NKDA.
Last night she was very agitated and was on the call light often, and her husband was at the bedside concerned. Apparently her Dilaudid dose of 2mg every 6 hours was not giving her relief, and the MD was notified and the medication was increased to 4mg every 4 hours, and her pain has been better controlled. In addition, the lab called with the 10AM H/H of 9 and 28. She is trending down from 10.1/30 and 11.3/32. I notified Doctor Jones, who ordered an H and H Q4hours and Type and cross plus started her on iron. Her repeat PTT and H/H were drawn at 2:00 PM.
Assessment:
Neurological – intact, AAOx3. Pain 3/10, last Dilaudid dose was given at noon.
CV- skin is warm, dry, and intact. No breakdown, no edema. Distal pulses intact bilaterally at 2+. ORIF incision is well approximated, no redness or drainage. Dressing changed at 1200. BP 132/82, HR 78. Temp 98.9. Heparin infusing via 18 gauge in right forearm at 800 units/hour. Last PTT was 50 and Doctor Jones wrote an order to continue infusion and recheck at 2200. Abductor pillow in place.
Resp – 18 and non-labored. Oxygen @ 4 L via NC and O2 Sat @ 98%. Lungs sound clear at the bases. No cough, no distress. She is using her incentive spirometer frequently
GI – Denies nausea and vomiting. Abdomen soft and non-tender with bowel sounds all quads. Had a large formed BM this afternoon. .
GU- Foley patent and draining clear yellow urine. Quantity sufficient
DIET - tolerating 1800 calorie ADA diet.
P/S – husband at the bedside all day. Since she is comfortable, he went home. She is planned for discharge to home this weekend, and homecare will follow up at home regarding her anticoagulant therapy and PT/OT. She is in a pleasant mood, since she is comfortable.
Recommendations: Check for the afternoon PTT and H/H results; remind Mrs. Jones that she can have pain medication again at 4:00 to keep her comfortable. Do you have any questions?
7