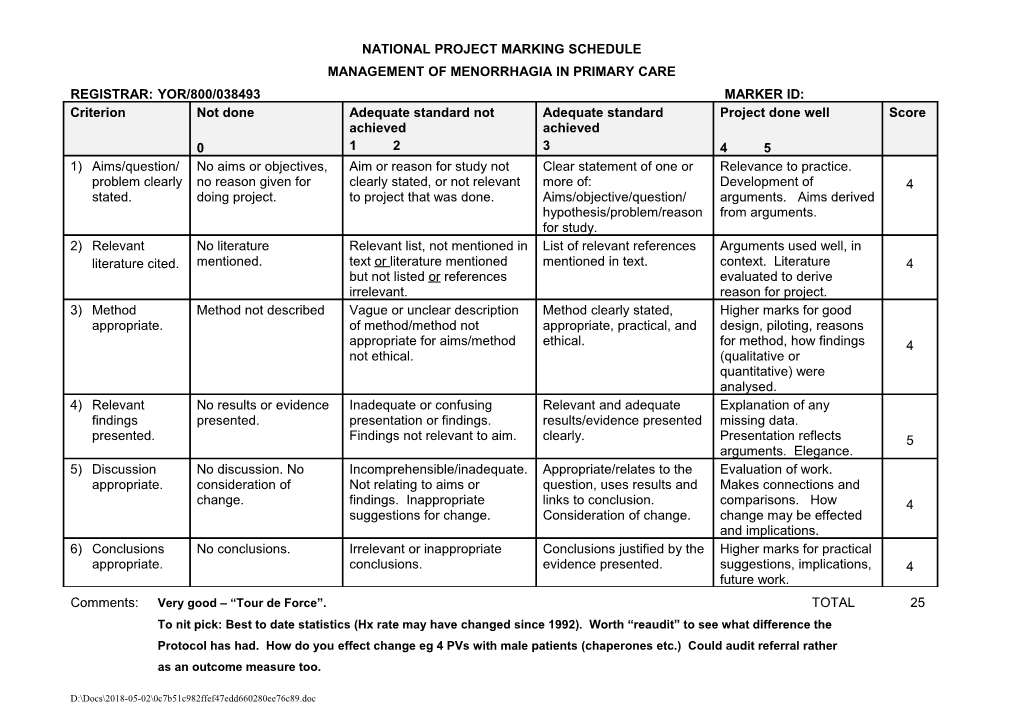
NATIONAL PROJECT MARKING SCHEDULE MANAGEMENT OF MENORRHAGIA IN PRIMARY CARE REGISTRAR: YOR/800/038493 MARKER ID: Criterion Not done Adequate standard not Adequate standard Project done well Score achieved achieved 0 1 2 3 4 5 1) Aims/question/ No aims or objectives, Aim or reason for study not Clear statement of one or Relevance to practice. problem clearly no reason given for clearly stated, or not relevant more of: Development of 4 stated. doing project. to project that was done. Aims/objective/question/ arguments. Aims derived hypothesis/problem/reason from arguments. for study. 2) Relevant No literature Relevant list, not mentioned in List of relevant references Arguments used well, in literature cited. mentioned. text or literature mentioned mentioned in text. context. Literature 4 but not listed or references evaluated to derive irrelevant. reason for project. 3) Method Method not described Vague or unclear description Method clearly stated, Higher marks for good appropriate. of method/method not appropriate, practical, and design, piloting, reasons appropriate for aims/method ethical. for method, how findings 4 not ethical. (qualitative or quantitative) were analysed. 4) Relevant No results or evidence Inadequate or confusing Relevant and adequate Explanation of any findings presented. presentation or findings. results/evidence presented missing data. presented. Findings not relevant to aim. clearly. Presentation reflects 5 arguments. Elegance. 5) Discussion No discussion. No Incomprehensible/inadequate. Appropriate/relates to the Evaluation of work. appropriate. consideration of Not relating to aims or question, uses results and Makes connections and change. findings. Inappropriate links to conclusion. comparisons. How 4 suggestions for change. Consideration of change. change may be effected and implications. 6) Conclusions No conclusions. Irrelevant or inappropriate Conclusions justified by the Higher marks for practical appropriate. conclusions. evidence presented. suggestions, implications, 4 future work. Comments: Very good – “Tour de Force”. TOTAL 25 To nit pick: Best to date statistics (Hx rate may have changed since 1992). Worth “reaudit” to see what difference the Protocol has had. How do you effect change eg 4 PVs with male patients (chaperones etc.) Could audit referral rather as an outcome measure too.
D:\Docs\2018-05-02\0c7b51c982ffef47edd660280ee76c89.doc