PANCREATITIS HANDOUT 2008
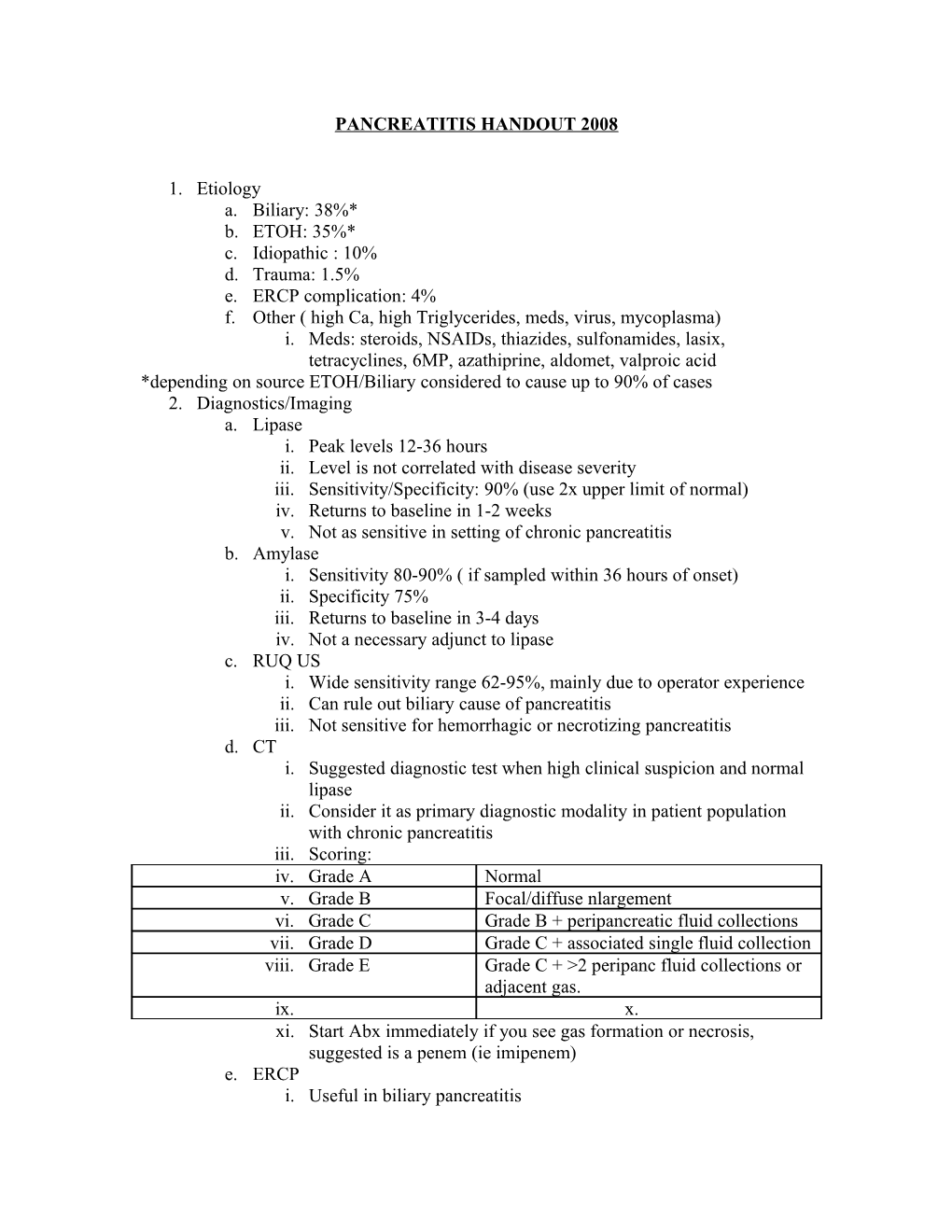
1. Etiology a. Biliary: 38%* b. ETOH: 35%* c. Idiopathic : 10% d. Trauma: 1.5% e. ERCP complication: 4% f. Other ( high Ca, high Triglycerides, meds, virus, mycoplasma) i. Meds: steroids, NSAIDs, thiazides, sulfonamides, lasix, tetracyclines, 6MP, azathiprine, aldomet, valproic acid *depending on source ETOH/Biliary considered to cause up to 90% of cases 2. Diagnostics/Imaging a. Lipase i. Peak levels 12-36 hours ii. Level is not correlated with disease severity iii. Sensitivity/Specificity: 90% (use 2x upper limit of normal) iv. Returns to baseline in 1-2 weeks v. Not as sensitive in setting of chronic pancreatitis b. Amylase i. Sensitivity 80-90% ( if sampled within 36 hours of onset) ii. Specificity 75% iii. Returns to baseline in 3-4 days iv. Not a necessary adjunct to lipase c. RUQ US i. Wide sensitivity range 62-95%, mainly due to operator experience ii. Can rule out biliary cause of pancreatitis iii. Not sensitive for hemorrhagic or necrotizing pancreatitis d. CT i. Suggested diagnostic test when high clinical suspicion and normal lipase ii. Consider it as primary diagnostic modality in patient population with chronic pancreatitis iii. Scoring: iv. Grade A Normal v. Grade B Focal/diffuse nlargement vi. Grade C Grade B + peripancreatic fluid collections vii. Grade D Grade C + associated single fluid collection viii. Grade E Grade C + >2 peripanc fluid collections or adjacent gas. ix. x. xi. Start Abx immediately if you see gas formation or necrosis, suggested is a penem (ie imipenem) e. ERCP i. Useful in biliary pancreatitis ii. Can decrease morbidity/mortality if used in the first 72 hours iii. Can cause pancreatitis f. CXR i. Nondiagnostic but may see certain changes ii. Pleural effusion (particularly L) iii. Colon changes c/w ileus iv. Elevated hemidiaphragm v. Pericardial effusion 3. Clinical Features a. LUQ/epigastric pain that most commonly radiates to the back, b. Tachycardia, febrile, hypotension, distress c. +/- associated ileus d. Cullen’s sign ( bluish discoloration around the umbilicus); rare and late finding e. Gray Turner’s sign (bluish discoloration at the flanks) rare and late finding 4. Disposition a. Based on labs, comorbidities, clinical condition, vital signs, age b. If the patient is young, pain is controlled, they have normal vital signs, no other labs abnormalities, no biliary cause, tolerating po and close follow up can be managed as an outpatient all others must be admitted (which means most of them!) c. Mortality is around 25% d. Clinical Rules can be used for stratification, but are minimally helpful in the ED i. Ranson’s Criteria: ii. At admission iii. Initial 48 h iv. Age >55 v. Hct drop >10% vi. WBC >16k vii. BUN increase >5 viii. Glucose >200 ix. Ca <8 x. LDH >350 xi. PaO2 <60 xii. AST >250 xiii. Base deficit >4 xiv. Fluid sequestration >6L
xv. Score 0-2 2% mortality, Score 3-4 15% mortality, Score 5-6 40% mortality, score 7-8 100% mortality xvi. Sensitivity 63% & Specificity 76% xvii. Modified Glasgow score: 1. age >55 2. pO2 <60 mmHg 3. WBC >15 4. Ca <2 5. LDH >600 6. glucose >10mmol/L 7. BUN >16 mmol/L 8. albumin <3.2 g/L 9. Min score 0 and Max score 8: if <3 severe pancreatitis unlikely, if > or = to 3 severe pancreatitis is likely xviii. Sensitivity 72% & Specificity 84% xix. APACHE II score (>8 predicts 11-18% mortality) 1. Hemorrhagic peritoneal fluid 2. obesity 3. indicators of organ failure 4. hypotension or tachycardia 5. po2<60 mmHg 6. Oliguria (<50 mL/h) or increasing BUN/Cr 7. Serum Ca <1.9 mmol/L (8 mg/dL) or serum albumin <33g/L (3.2 g/dL) 5. Management a. IVF –aggressive hydration b. NPO/bowel rest c. Antiemetics/analgesics d. Monitor electrolytes e. Add antibiotics with necrotizing pancreatitis or concern for infection/sepsis 6. Complications a. ARDS b. ARF c. Cardiac depression/arrhythmias d. Sepsis/shock e. Pancreatic necrosis/hemorrhage/pseudocyst f. Hyperglycemia g. hypocalcemia