RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES KARNATAKA, BANGALORE
ANNEXURE II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
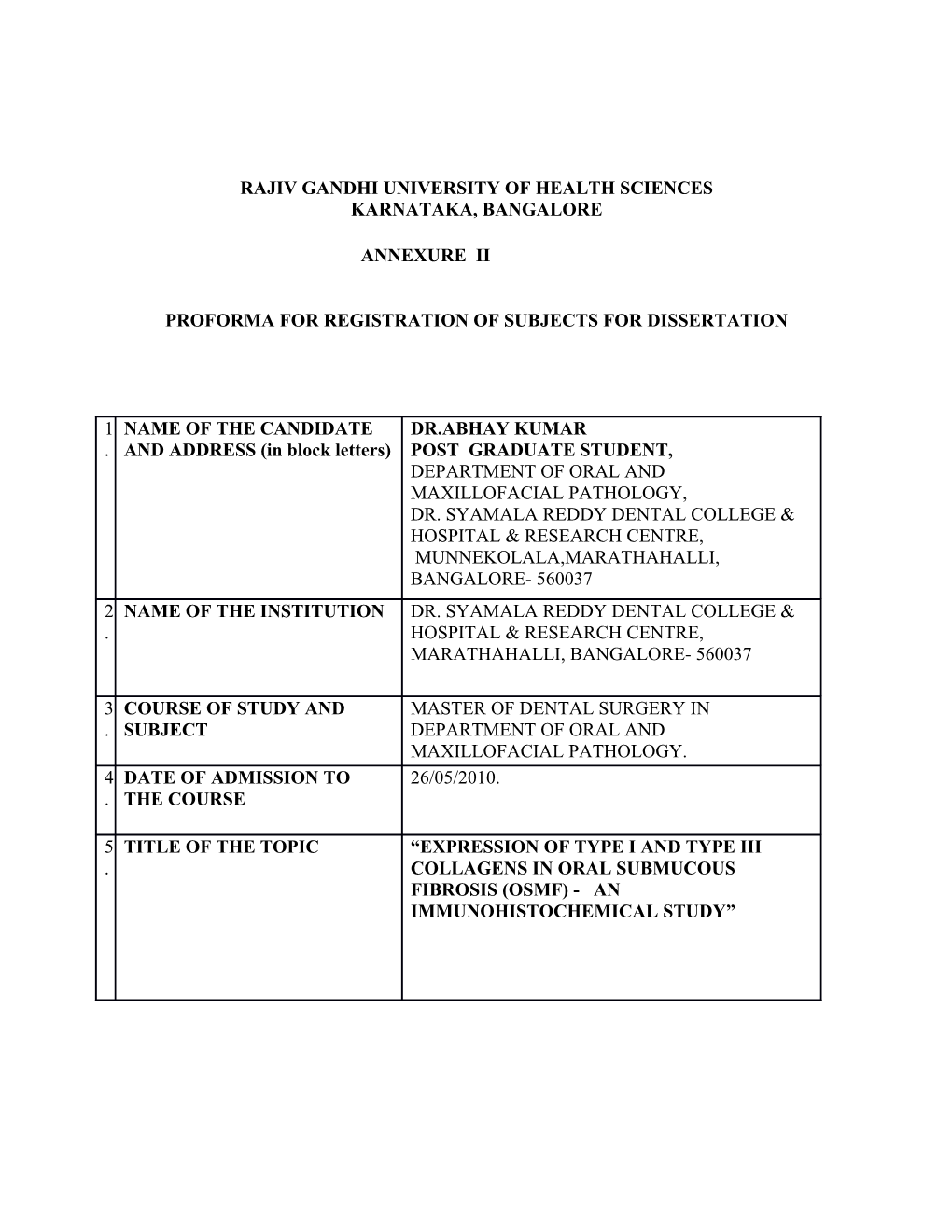
1 NAME OF THE CANDIDATE DR.ABHAY KUMAR . AND ADDRESS (in block letters) POST GRADUATE STUDENT, DEPARTMENT OF ORAL AND MAXILLOFACIAL PATHOLOGY, DR. SYAMALA REDDY DENTAL COLLEGE & HOSPITAL & RESEARCH CENTRE, MUNNEKOLALA,MARATHAHALLI, BANGALORE- 560037 2 NAME OF THE INSTITUTION DR. SYAMALA REDDY DENTAL COLLEGE & . HOSPITAL & RESEARCH CENTRE, MARATHAHALLI, BANGALORE- 560037
3 COURSE OF STUDY AND MASTER OF DENTAL SURGERY IN . SUBJECT DEPARTMENT OF ORAL AND MAXILLOFACIAL PATHOLOGY. 4 DATE OF ADMISSION TO 26/05/2010. . THE COURSE
5 TITLE OF THE TOPIC “EXPRESSION OF TYPE I AND TYPE III . COLLAGENS IN ORAL SUBMUCOUS FIBROSIS (OSMF) - AN IMMUNOHISTOCHEMICAL STUDY” 6. BRIEF RESUME OF INTENDED WORK:
6.1 Need for the study:
Collagens are most abundant proteins in the human body. Collagens are insoluble, extracellular, glycoproteins. Collagens are essential structural components of all connective tissues. They strengthen and support many tissues in the body, therefore collagen composition within each tissue needs to be maintained for proper tissue integrity. Till date about 19 types of collagen have been identified in humans. Collagens I, II & III are present in abundance in the human body (80- 90% of all types of collagens).The collagen molecules pack together side by side to form long thin fibrils of similar structure . Collagen Type I is long, thin fibril and found in abundance in most connective tissues, having enormous tensile strength. Col I alpha I is a human gene that encodes the major component of Type I collagen and is located on chromosome 17. Col 3 alpha1 genes located on chromosomes 2 and encodes type III collagens. Collagen type III is frequently present in association with Type I collagen. Oral Submucous Fibrosis (OSMF) is an insidious , chronic disease affecting any part of oral cavity, associated with a juxtapithelial inflammatory reaction followed by a fibro-elastic change of the lamina propria, with epithelial atrophy, characterized by burning sensation in oral cavity, blanching and stiffness of the oral mucosa leading to trismus and inability to open the mouth . The excessive fibrosis in the mucosa is the primary pathology in OSMF. The important histopathological features of OSMF are connective tissue changes characterized by deposition of dense collagen fibres with or without alteration of collagen types in oral mucosa; OSMF is hence regarded as a disease of altered collagen metabolism (i.e. increased collagens fiber production & decreased collagen degradation resulting in formation & deposition of dense collagens fibers bundles in oral tissue leading to fibrosis). OSMF is also considered as a pre-malignant condition, with the reported risk of malignant transformation of 7.6%.
Immunochemistry (IHC) refers to the process of localizing proteins in cells of a tissue sections exploiting the principle of antibodies binding specifically to antigens in biological tissues. IHC is widely used in basic research to understand the distribution and localization of biomarkers and differentially expressed proteins in different parts of a biological tissue. Immunohistochemical procedures have become an integral part of the clinical laboratory routine, evolving from a research tool to a diagnostic necessity in pathology. Direct involvement of collagens in the pathophysiology of various disease processes has been established, so it is but natural that the expression and role of collagens in OSMF be assessed to understand the pathogenesis of the lesion. The excessive fibrosis may be due to an abnormal deposition of normal collagen with preserved phenotype or with an alteration of phenotype and consequent resistance to degradation mechanisms. We plan to study the identification & expression of collagen I and III in OSMF by immunohistochemistry & compare it with normal mucosa.
6.2 Review of Literature:
In a study, Hiroko and his colleagues examined forty biopsy specimen of OSF and 10 of normal buccal mucosa for expression/deposition modes of eight ECM moleculs( like collagen III, collagen I, fibronectin etc) . In early stages of oSF, collagen III, tenascin , fibronectin were characteristically enhanced in the lamina propria and the submucosal layer. In advanced stage, collagen III, fibronectin,tenascin deposition decreased and were entirely replaced with collagen type I only. The result indicates that the ECM remodeling steps in OSf are similar to each phase of usual granulation tissue formation. Restricted mouth opening may be a result of loss of variety of ECM molecules including elastin in the homogeneity of collagen type I replacing muscle fibres1.
An investigation was done to compare fibroblast (responsible for production of collagens I and III) population in oral submucous fibrosis and compared with healthy oral mucosa. The result showed relatively high fibroblast (F3), which produced significantly large quantities of collagen type I and III in oral submucous fibrosis cases2.
An immuohistochemical study done on distribution of procollagen type III, collagen type VI and tenascin in OSMF revealed a loss of stainable procollagen type III and collagen type VI in the fibrotic zones of oral submucous fibrosis compared to normal oral mucosa. This study showed predominance of collagen type I in collagen fiber bundles with loss of procollagen type III and almost complete loss of collagen type VI3. . Presence of collagen fibrils surrounding normal airways, are a prominent feature of airway remodeling in human asthma with evidence of enhanced collagen III and I fibril deposition. An immune-labeling method was developed to identify collagen I and III in equine lung and to describe the collagen fiber type and distribution within the walls of the noncartilagenous bronchioles. Results of this study showed that collagens I and III were present in the lamina propria and adventitial area of the noncartilaginous bronchioles4.
A study was being conducted on fibrosis of bladder tissue characterized by an abnormal deposition of connective tissue within different layers of the bladder wall, ultimately contributing to renal scarring and failure. They examined molecular mechanisms responsible by analyzing alteration in collagen types I and III. Immunohistochemical localization of collagen types I ,III and IV was carried out using type specific monoclonal antibodies. The result showed connective tissue infiltration of smooth muscle bundles been specific for collagen type III. Protein analysed demonstrated 1) an increase in total collagen 2) a statistically significant increase in collagen III and ratio5. The distribution of collagens I and III in mouse oral mucosa and the age-related changes over 3days to 2 years of age was examined by immunofluorescence and electron microscopy, with use of purified polyclonal antibodies. The staining intensity of collagen I was stronger and increased more markedly in the lamina propria of the hard palate and gingiva than in buccal mucosa. For Collagen III staining intensity markedly increased with age in all connective tissues examined. Examination of immune gold–labeled tissues demonstrated that most of the collagen fibrils were labeled for both type I and III collagens . This study was first to demonstrate the distribution of collagens I and III and collagens age related changes in mouse oral mucosa6.
6.3 OBJECTIVE OF THE STUDY 1) Evaluate and analyze the distribution of the collagen I and III in different stages of OSMF- by immunohistochemistry.
2) Compare the expression of collagen I and III in OSMF with healthy oral buccal mucosa.
3) To assess genetic correlation and changes related to the altered expressions of Type I and Type III collagens in OSMF, if feasible.
7.Materials and methods 7.1 Source of the data:
Paraffin embedded tissues from cases which satisfy the criteria will be included in the study. Though archival sections would be the target, fresh biopsies would be taken if the need arises in all the mentioned groups. Routine procedures of consent and patient information and clearances from the Ethical Research Committee will be ensured.
7.2 METHOD OF COLLECTION OF DATA
Paraffin wax embedded slides of the following groups to be utilized either from archival collections (preferably) or fresh biopsies ( as the need arises).
1) Individuals with clinically proven cases of OSMF -50. 2) Individuals with tobacco and areca nut related habits but without clinical OSMF - 50 3) Normal mucosa- 25. 4) Paraffin sections of other collagen disorders such as scleroderma, keloid, scar tssue etc.- (maximum number attainable)
7.3 METHODOLOGY:
All the slides will be stained and diagnostically verified by a group of independent observers. 1. All paraffin sections to be stained with hematoxylin and eosin for establishing diagnosis, grade and tissue changes as per standard criteria. 2. All paraffin sections to be additionally stained with collagen stains Van Gieson and/or Mallory’s Trichrome for collagen identification and distribution. 3. All paraffin sections to be immunohistochemically stained with antibodies to Type I and Type III collagen. Staining of the slides to be done according to standard protocol provided by manufacturer. 4. Areas of expression of immunomarker will be assessed visually using a standard compound microscope and by image analysis software along with standard light microscope. . 7.3 Does the study require any investigation or intervention to be conducted on patients or other Humans or Animals? If so, please describe briefly. YES, biopsies of patients and relevant staining of tissue sections.
7.4 Has ethical clearance been obtained from your institution in case of 7.3? YES 8. List of references:
1: Utsunomiya H, Wanninayake M, Tilakaratne, Oshiro K, Maruyama S, Suzuki M, Yonemochi HI, Cheng J, Saku T: Extracellular matrix remodeling in oral submucous fibrosis: its stage specific modes revealed by immunohistochemistry and in situ hybridization. J Oral Path & Med.Vol 34,Issue 8, 2005
2: De Waal J, Olivier A, Van Wyk CW, Maritz JS:The fibroblast population in oral submucous fibrosis. J Oral Path & Med;26:69-74; 1997
3:Reichart, P.A., Van Wyk , C.W., Becker, J.and Schuppan D: Distribution of procollagen type III, collagen type VI, tenascin in oral submucous fibrosis(OSF).J Oral Path & Med.,vol 23,Issue 9,pages394-398, Oct 1994
4:Furness MC, Bienzle D, Caswell JL, Delay J, Viel L :Immunohistochemical Identification Of Collagen in the Equine Lung. Univ of Guelph, Guelph, Ontario , Canada
5: Catherine M. D, Edward J. M, Umberto K, David H. E, William R. A, Pamela S. H: Molecular Analysis Of Collagens In Bladder Fibrosis.J Urology,Vol 160, Issue 4,1518-1527,Oct 1998
6:Xu L X, Ohsaki Y, Nagata K, Kurisu K:Immunohistochemical Studies On the Distributions And Age Related Changes Of Types I and III Collagen In The Oral Mucosa Of Mice. J Dent Res, 72(9):1336-43; Sep1993.
9. Signature of the candidate:
10. Remarks of guide: 11. Name and designation of : (in block letters) 11.1 Guide: Dr. V.V.KAMATH PROFESSOR AND HEAD, DEPARTMENT OF ORAL AND MAXILLOFACIAL PATHOLOGY, Dr.SYAMALA REDDY DENTAL COLLEGE HOSPITAL & RESEARCH CENTRE, BANGALORE-560037 11.2 Signature:oo
11.3 Co- guide (if any): DR KRISHNANAND P SATELUR READER DEPARTMENT OF ORAL AND MAXILLOFACIAL PATHOLOGY DR SYAMALA REDDY DENTAL COLLEGE, HOSPITAL AND RESEARCH CENTRE, MUNNEKOLALA, MARATHALLI, BANGALORE-560037. 11.4 Signature:
11.5 Head of the DR.V.V.KAMATH Department: PROFESSOR AND HEAD, DEPARTMENT OF ORAL AND MAXILLOFACIAL PATHOLOGY, Dr.SYAMALA REDDY DENTAL COLLEGE HOSPITAL & RESEARCH CENTRE, BANGALORE-560037
11.6 Signature:
12. 12.1 Remarks of the Chairman and Principal
12.2 Signature: