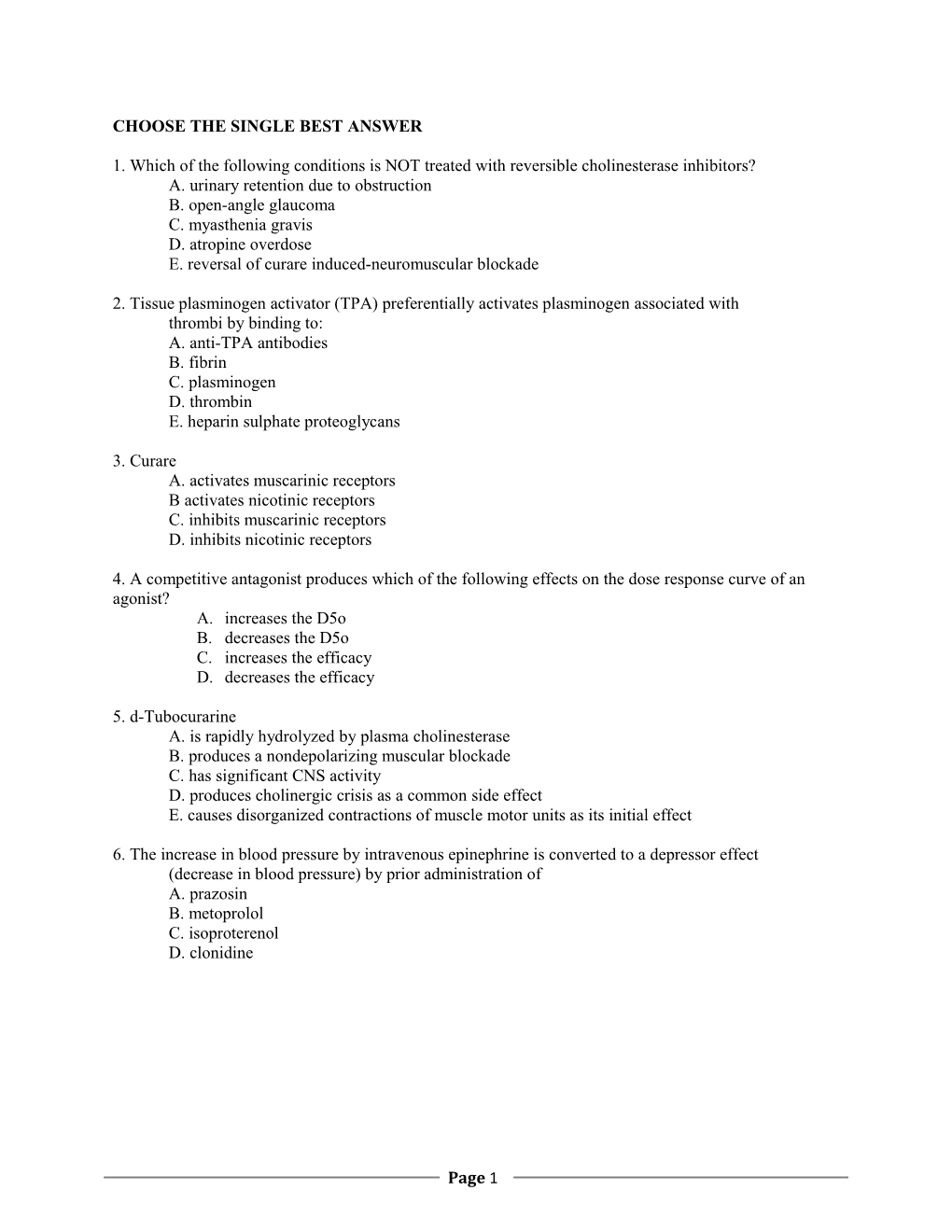
CHOOSE THE SINGLE BEST ANSWER
1. Which of the following conditions is NOT treated with reversible cholinesterase inhibitors? A. urinary retention due to obstruction B. open-angle glaucoma C. myasthenia gravis D. atropine overdose E. reversal of curare induced-neuromuscular blockade
2. Tissue plasminogen activator (TPA) preferentially activates plasminogen associated with thrombi by binding to: A. anti-TPA antibodies B. fibrin C. plasminogen D. thrombin E. heparin sulphate proteoglycans
3. Curare A. activates muscarinic receptors B activates nicotinic receptors C. inhibits muscarinic receptors D. inhibits nicotinic receptors
4. A competitive antagonist produces which of the following effects on the dose response curve of an agonist? A. increases the D5o B. decreases the D5o C. increases the efficacy D. decreases the efficacy
5. d-Tubocurarine A. is rapidly hydrolyzed by plasma cholinesterase B. produces a nondepolarizing muscular blockade C. has significant CNS activity D. produces cholinergic crisis as a common side effect E. causes disorganized contractions of muscle motor units as its initial effect
6. The increase in blood pressure by intravenous epinephrine is converted to a depressor effect (decrease in blood pressure) by prior administration of A. prazosin B. metoprolol C. isoproterenol D. clonidine
Page 1 7. Which of the following may be useful in preventing chronic embolic complications associated with the presence of a prosthetic mitral valve A. heparin B. vitamin K C. streptokinase D. coumadin E. protamine
8. A drug is highly selective if it A. exhibits first order elimination B. produces therapeutic effects before toxicity occurs
C. has a low D50 D. has a high therapeutic index E. is metabolized to inactive compounds
Matching. Match a mechanism of action to each drug. Each may be used once, more than once, or not at all. A. inhibits synthesis of cholesterol B. decreases reabsorption of bile acids C. increases fatty acid oxidation D. blocks binding of LDL to scavenger receptors E. increases lipoprotein lipase (LPL) activity
9. _____ Cholestyramine
10. _____ Atorvastatin
11. _____ Clofibrate
CHOOSE THE SINGLE BEST ANSWER
12. The value of low doses of aspirin (ASA) in decreasing the risk of coronary artery thrombosis is based on its ability to induce: A. inhibition of platelet cyclooxygenase B. inhibition of ADP receptors C. activation of plasminogen D. activation of endothelial cyclooxygenase E. activation of anti-thrombin
13. Which of the following may be useful in controlling the ventricular rate of a patient presenting to the emergency room with atrial fi associated with a rapid ventricular response rate? A. adenosine B. lidocaine C. quinidine D. verapamil E. dobutamine
14. If an agonist drug is removed from the body by renal elimination, what will be the effect of impaired renal function? A. decrease the potency of the drug B. increase the potency of the drug C. decrease the efficacy of the drug D. increase the efficacy of the drug
Page 2 15. Dihydropyridines such as nifedipine decrease blood pressure because they A. increase catabolism of epinephrine B. inhibit influx of Ca 2+ C. are vagolytic D. increase production of nitric oxide E. decrease renin production
16. Bradycardia due to digitalis - induced heart block may be treated with which of the following: A. metoprolol B. verapamil C. epinephrine D. atropine E. amiodarone
17. Drug X is a weak base with a pK of 8.4. What will be the ratio of unprotonated to protonated forms of the drug in the plasma at pH 7.4?
A. 0.01 B. 0.10 C. 1.0 D. 10 E. 100
18. The anti-arrhythmic properties of amiodarone are due in part to its ability to A. slow conduction through the AV node B. increase the effective refractory period of cardiac cells C. increase vagal tone D. activate Na+-channels E. inhibit Na+, K+-ATPase
19. Which of the following drugs would NOT be used in the treatment of glaucoma? A. carbachol B. physostigmine C. pilocarpine D. timolol E. atropine
20. First pass metabolism of a drug may be decreased by which of the following? A. administration of the drug on an empty stomach B. formulation as enteric coated capsules that dissolve in the intestine C. substituents that decrease metabolism by hepatic P450's D. modifications that increase plasma protein binding E. alterations that increase the partition coefficient of the drug
21. Use of a beta-adrenergic receptor antagonist (beta-blocker) is indicated for a patient with a symptomatic arrhythmia due to which of the following conditions? A. acute left ventricular failure B. heart block C. hypercalcemia D. hyperthyroidism E. hyperkalemia
Page 3 22. Which of the following events is NOT a corollary of the Fight or Flight response A. increased liver glycogenolysis B. vasoconstriction in the skin and musosa C. reduced blood flow to the kidneys and abdominal viscera D. decrease in lipolysis E. relaxation of bronchiolar smooth muscle
23. The selective activity of lidocaine as an anti-arrhythmic is attributable to its
A. preferential activity in depolarized tissues + B. preferential binding to resting Na -channels C. a vagolytic activity D. short half-life E. inactivation by molecular O2
24. A patient with myasthenia gravis who is being treated with neostigmine complains of side effects that include constant sweating, salivation, and urination. Which of the following treatments would be most effective? A. terminate neostigmine treatment B. prescribe atropine in addition to neostigmine C. prescribe bethanechol in addition to neostigmine D. prescribe physostigmine instead of neostigmine E. increase neostigmine treatment
25. Which of the following drugs can be used to provide anti-coagulation in a patient who is pregnant, has thrombophlebitis, (TPA), and is judged to be at risk for pulmonary emboli? A. aspirin B. heparin C. coumadin D. vitamin K E. tissue plasminogen activator (TPA)
26. Which subfamily of cytochrome P450 is responsible for the highest number of clinically important drug interactions based upon metabolism? A. 1C B. 2D C. 3A D. 4B E. 5E
27. Which of the following EKG abnormalities is indicative of toxicity due to a Class I anti- arrhythmic such as quinidine? A. loss of the P-wave B. T-wave inversion C. ST-segment elevation D. prolongation of the PR interval E. broadening of the QRS complex
28. Glucuronyl transferase is unique among phase 11 or synthetic drug biotransformation reactions because it A. utilizes acetyl CoA as a co-factor B. catalyzes the hydrolysis of succinylcholine C. produces metabolites readily reabsorbed in the kidney D. is inducible by chronic drug administration E. catalyzes the oxidation of aromatic hydrocarbons
Page 4 29. A partial agonist at saturating concentrations A. incompletely activates all of its receptors B. cannot activate some of its receptors at all C. has low potency D. has weak binding to its receptor
30. Cocaine acts by A. directly blocking vesicular uptake of cytoplasmic norepinephrine into chromogranins B. blocking the neuronal transport system I for catecholamines C. inhibiting mitochondrial monoamine oxidase D. decreasing norepinephrine interaction with postsynaptic as-adrenergic receptors E. stimulating presynaptic α2-adrenergic receptors
31. Which of the following classes of drugs is thought to be useful in preventing the ventricular remodeling associated with chronic congestive heart failure? A. beta-adrenergic receptor agonists B. cardiac glycosides C. angiotensin converting enzyme inhibitors D. phosphodiesterase inhibitors E. calcium channel blockers
32. The α1 adrenergic receptor primarily acts by being coupled to A. a pentameric ion channel B. a G protein C. transcription factors D. a membrane bound phosphatase
33. Drug X has a volume of distribution of 0.6 liters/kg body weight. What loading dose of drug (in μg) will you administer i.v. to a 60 kg woman to obtain an initial plasma concentration of 0.3 μg/liter? A. 3.6 B. 10.8 C. 18.0 D. 72.8 E. 180
34. Which of the following receptors mediate smooth muscle contraction
A. β1 -adrenergic B. β2-adrenergic C. α2-adrenergic D. α 1-adrenergic E. β3-adrenergic
Matching. Each may be used once, more than once, or not at all. A. d-tubocurarine B. ipratropium C. hexamethonium D. succinylcholine E. carbachol
35._____ nicotinic agonist used for endotracheal intubation
Page 5 36. _____ Cholinergic antagonist used in the treatment of chronic obstructive pulmonary disease
37. Arterial vasodilators such as minoxidil
A. have greater effects on preload compared to afterload B. increase central sympathetic outflow C. are most often used as single agents for control of blood pressure D. act by blocking K+ channels E. decrease angiotensin II production
38. Prolonged treatment with propranolol may induce G-f) A. glaucoma
B. desensitization of β2-adrenergic receptors C. supersensitization of β 1 and β2-adrenergic receptors D. severe tremors E. non-specific blockade of amine transporters
39. The repolarization of a ventricular myocyte (phase 3) is due to A. reactivation of Na+-channels B. the opening of voltage - activated Ca+2 channels, C. activation of beta-adrenergic receptors D. activity of the Na+- K+ - ATPase E. opening of K+ channels
40. The increased excitability of myocardial cells associated with digitalis toxicity is due to A. increased intracellular Ca+2 B. decreased intracellular Na+ C. increased intracellular K+ D. hypokalemia E. decreased vagal tone
41. When given orally, which of the following statements about bethanechol is TRUE? A. It is sensitive to the action of acetylcholinesterase B. It binds both muscarinic and nicotinic receptors C. It should not be used in patients with asthma D. Its effects are reversed by physostigmine E. It can decrease bladder tone and intestinal contractions
42. Drugs which work by promotion of inositol triphosphate (IP3) turnover most likely cause activation of
A. G5 B. Gi C. Go D. Gq/11
43. Use of inotropic catecholamines such as dobutamine in patients with acute left ventricular failure is associated with an increased risk of A. pulmonary edema B. arrhythmias C. heart block D. decreased myocardial oxygen demand E. hypotension
Page 6 44. The agent of choice for treatment of acute anaphylactic type I hypersensitivity A. phenylephrine B. pindolol C. dopamine D. epinephrine E. dobutamine
45. A child is brought to the emergency room after ingesting a drug from the parent's medicine cabinet. If the plasma level of the drug is 100 µg/liter, the rate constant of elimination is 0.19/hour, and elimination is first-order, how long will it take (in hours) for the plasma level of drug to decrease to the non-toxic level of 15 pg/liter? C) . 19 A. 2.5 B. 5 C. 10 D. 25 E. 50
46. Which of the following clinical conditions is well suited for therapy with a cardiac glycoside such as digoxin? A. recurrent ventricular tachycardia B. chronic atrial fibrillation with heart failure C. ventricular arrhythmias associated with general anesthesia D. 2nd degree heart block E. hyperkalemia
47. Treatment of chronic severe asthma with an inhaled β2-adrenergic agonist alone is ill-advised because A. it allosterically blocks Ca++ channels B. it does not activate 131-adrenergic receptors C. it decreases heart rate D. it causes miosis E. it does not treat the underlying inflammation
48. Which of the following is a frequently encountered complication of prolonged therapy with procainamide? A. sedation B. lupus - like syndrome C. diarrhea D. masked hypoglycemia E. colorful visual abnormalities
49. The destruction of norepinephrine in nerve endings is performed for the most part by A. cytochrome P450 B. catechol-0-methyl transferase C. phosphodiesterase D. Monoamine oxidase E. Dopamine β-hydroxylase
Page 7 50. Which of the following drugs would be life-saving for a patient recently exposed to high levels of sarin or a similar type nerve gas? A. d-tubocurarine B. atropine C. succinylcholine D. pralidoxime E. carbachol
51. Doparnineis frequently used in patients with acute left ventricular failure and hypotension (cardiogenic shock) to A. decrease afterload B. increase pulmonary capillary wedge pressure C. decrease left ventricular pre-load D. increase cardiac contractility E. decrease renal blood flow
52. The antiarrhythmic activity of lidocaine is due to its ability to A. delay repolarization B. increase intracellular Na+ C. inhibit vagal activity D. prolong the effective refractory period E. suppress conduction through the AV node
53. Which of the following causes a general enhancement of parasympathetic activity? A. Hemorrhage B. Rage C. Helpless terror D. Jumping up from a supine position E. Sprinting away from a mugger
54. Nasal congestion can be treated with A. atenolol B. phenylephrine C. yohimbine D. guanethidine E. salmeterol
55. If the clearance of drug X is 20 liters/hour and its oral bioavailability is 50%, what maintenance dose (in µg/hour) will you administer orally to achieve a steady-state plasma concentration of 0.1 µg/liter. A. 2 B. 4 C. 6 D. 8 E. 10
Page 8 56. Drug X induces a hepatic P450 that catalyzes the biotransformation of X to an inactive metabolite. Chronic administration of drug X will increase which of the following parameters of the drug?
A. clearance B. oral bioavailability C. volume of distribution D. therapeutic index E. efficacy
57. Slow infusion of norepinephrine (NE) causes bradycardia because A. NE hyperpolarizes pacemaker cells in the SA node B. Neurons in the vasomotor center are directly excited by the NE that crosses the blood-brain barrier C. NE inhibits the release of NE from sympathetic varicosities in the SA node D. NE -induced vasoconstriction triggers reflex vagal nerve firing E. NE increases unstressed volume
58. Nitroglycerine is useful in treating angina because it A. has a slow onset of action and a long half-life B. has predominant effect on arterial tone
C. decreases myocardial O2 demand D. increases myocardial contractility E. decreases formation of atherosclerotic plaques
59. The positive inotropic activity of beta - adrenergic agonists is due to A. activation of "L"-type Ca +2 channels B. inhibition of cyclic nucleotide phosphodiesterase C. activation of the Ca+2-ATPase D. inhibition of the Na+/ Ca+2- exchanger E. phosphorylation of acto-myosin
60. Intravenous infusion of drug X at a dose rate of I µg/hour produces a steady-state plasma drug concentration of 0.05 µg/liter. If X is eliminated 75% by hepatic metabolism and 25% by renal elimination, what is the renal clearance of the drug (in liters/hour)? - A. 5 B. 10 C. 15 D. 20 E. 25
61. The action of nifedipine on L-type calcium channels A. decreases K+ efflux B. is enhanced by cAMP C. is greater in arterial compared to cardiac smooth muscle cells D. increases myocardial contractility E. decreases AV nodal conduction
Page 9 62. Use of β-blockers is contraindicated for all of the following EXCEPT A. Chronic obstructive pulmonary disease (COPD) B. Insulin-dependent diabetes C. Asthma D. Hypertension E. First degree heart block
63. Congestive heart failure is likely to alter the half-life of which of the following drugs? A. adenosine B. amiodarone C. digoxin D. aspirin E. lidocaine
Page 10 ANSWERS: 53. C 1. A 54. B 2. B 55. B 3. D 56. A 4. A 57. D 5. B 58. C 6. A 59. A 7. D 60. A 8. D 61. C 9. B 62. D 10. A 63. E 11. E 12. A 13. D 14. B 15. B 16. D 17. B 18. B 19. E 20. C 21. D 22. D 23. A 24. B 25. B 26. C 27. E 28. D 29. A 30. B 31. C 32. B 33. B 34. D 35. D 36. B 37. B 38. C 39. E 40. A 41. C 42. D 43. B 44. D 45. C 46. B 47. E 48. B 49. D 50. B 51. D 52. D
Page 11