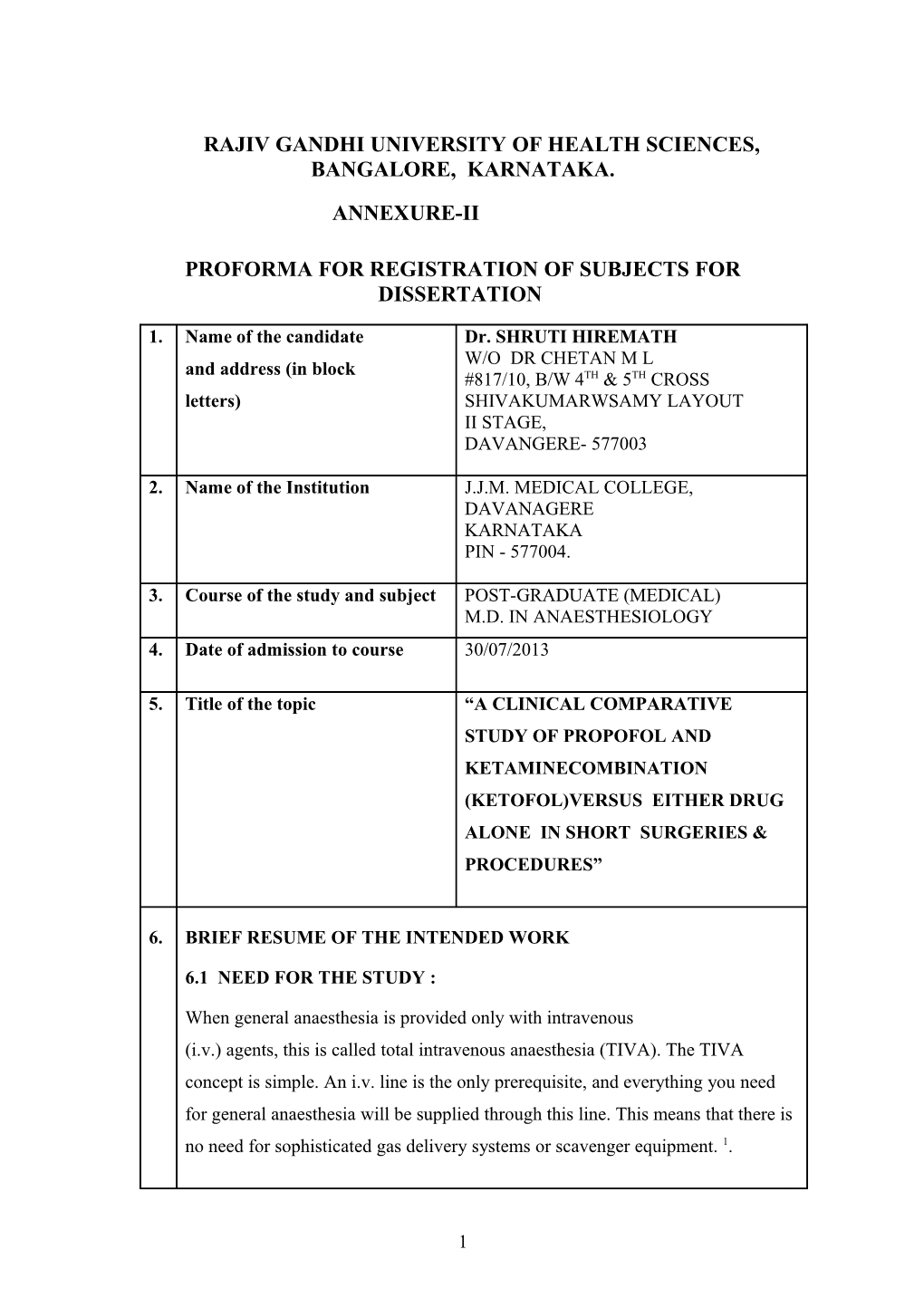
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE, KARNATAKA.
ANNEXURE-II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. Name of the candidate Dr. SHRUTI HIREMATH W/O DR CHETAN M L and address (in block #817/10, B/W 4TH & 5TH CROSS letters) SHIVAKUMARWSAMY LAYOUT II STAGE, DAVANGERE- 577003
2. Name of the Institution J.J.M. MEDICAL COLLEGE, DAVANAGERE KARNATAKA PIN - 577004.
3. Course of the study and subject POST-GRADUATE (MEDICAL) M.D. IN ANAESTHESIOLOGY 4. Date of admission to course 30/07/2013
5. Title of the topic “A CLINICAL COMPARATIVE STUDY OF PROPOFOL AND KETAMINECOMBINATION (KETOFOL)VERSUS EITHER DRUG ALONE IN SHORT SURGERIES & PROCEDURES”
6. BRIEF RESUME OF THE INTENDED WORK
6.1 NEED FOR THE STUDY :
When general anaesthesia is provided only with intravenous (i.v.) agents, this is called total intravenous anaesthesia (TIVA). The TIVA concept is simple. An i.v. line is the only prerequisite, and everything you need for general anaesthesia will be supplied through this line. This means that there is no need for sophisticated gas delivery systems or scavenger equipment. 1.
1 TIVA has many advantages over inhalational anesthesia such as no operating room pollutions, minimal cardiac depression, lesser neurohumoral response, decreased oxygen consumption 2. Various drugs have been tried from time to time in TIVA. Since no single drug can provide all the characteristics of an ideal intravenous agent, several drugs are used in different combinations to provide balanced anesthesia in TIVA, that is, amnesia, hypnosis and analgesia 2. Propofol is a preferred inducing agent for short surgical procedures is a nonopioid, nonbarbiturate, sedative-hypnotic agent with rapid induction and recovery times and antiemetic effects 3. However, adverse effects include dose-dependent cardiorespiratory depression, injection pain, and having no analgesic properties 3, 4,5. Ketamine causes little or no cardio-respiratory depression and unlike propofol, has pain relieving properties. Ketamine use as a single induction agent, however, is limited by emergence hallucinations, elevation of blood pressure and heart rate due to its sympathomimetic effects, and increased intracranial pressure 6,7.
Effectiveness of the two agents – propofol and ketamine – in combination (ketofol) has been recently demonstrated and may provide a novel induction agent with favorable hemodynamics and reduced side effects attributed to either drugs8. By combining propofol and ketamine, there is additive effect of GABA agonism by propofol and NMDA antagonism by ketamine leading to lesser doses of propofol required along with ketamine 9. Ketamine in subanaesthetic doses with propofol has gained attention in total intravenous anaesthetic technique because of its powerful analgesic action without causing myocardial or respiratory depression 10,11,12.
6.2 REVIEW OF LITERATURE :
In a randomized double blind prospective study which included 90 ASA I & II patients aged between 15 and 50 years scheduled for ambulatory urological; ambulatory urogynaecological procedures, they concluded tht among the two
2 admixtures propofol ketamine has an edge over propofol-thiopentone because of its better hemodynamic stability and superior airway maintenance 9.
In a randomized double blind prospective study which included 100 chidrens scheduled for LMA insertion the effects of ketofol and propofol were compared and concluded that ketofol is a safe and effective alternative induction agent for LMA insertion in children with rapid onset of action and lower incidence of injection pain. It provided better LMA insertion conditions, improved hemodynamic stability with less prolonged apnoea when compared with propofol3.
In a randomized double blind prospective study which included 80 ASA I & II patients posted for laryngeal tube suctioning compared the effects of propofol and ketofol and concluded that ketofol provided better insertion summed score for LTS than propofol with minimal haemodynamic changes 9.
In a randomized double blind prospective study which included 40 female pa- tients undergoing short gynaecological procedures concluded that the association propofol-ketamine reach an adequate level of anesthesia with few and negligible effects on cardiorespiratory system, thus allowing a better operability and safety. The incidence of post operative psychotic disturbances seems to be low and mod- erate.
In a randomized double blind prospective study which included 68 ASA I & II patients undergoing elective general, orthopaedic & gynaecological procedures concluded that induction dose of propofol is reduced considerably by prior ad- ministration of small dose of ketamine compared to placebo using loss of verbal contact as end point of induction. Ketamine had the advantage of better haemo- dynamic stability 13.
In the 10 trials comparing the combination of ketamine and propofol with either agent alone for procedural sedation in the emergency department were examined. The evidence reviewed suggests that combining these agents may help to mini- mize adverse effects such as hypotension and respiratory depression. Ketamine is
3 not commonly used as a single agent in adults because of the risk for emergence reactions; however, when combined with propofol, no significant increase in this adverse effect was found compared with propofol monotherapy14.
In a randomized double blind prospective study which included 100 children, of age 3–14 years, American Society of Anesthesiologist physical status IE-IIE, posted for emergency short surgical procedures concluded that The combination of low-dose ketamine and propofol is more effective and a safer sedoanalgesia regimen than the propofol–fentanyl combination in paediatric emergency short surgical procedures in terms of haemodynamic stability and lesser incidence of apnoea15
In a randomized double blind prospective study which included 90 adults patients Posted for LMA insertion concluded that the addition of ketamine 0.5 mg x kg(- 1) improves haemodynamics when compared to fentanyl 1 microg x kg(-1), with less prolonged apnoea, and is associated with better LMA insertion conditions
16 than placebo (saline) .
In a randomized double blind prospective study which included 60 healthy women undergoing gynaecological laparoscopy to investigate infertility were studied, and concluded that use of low-dose ketamine with propofol-fentanyl anaesthesia in patients undergoing DGL was associated with less pain during propofol injection, lower incidence of haemodynamic changes, lower total dose of propofol and improved postoperative analgesia17.
6.3 AIMS AND OBJECTIVES OF STUDY :
The objectives of this comparative study using propofol, ketamine and ketofol as an inducing agents in short surgical procedures is to evaluate and compare the
4 following effects.
Onset of induction
Duration
Quality of analgesia
Cardiorespiratory stability
Emergence phenomenon
Recovery
Adverse effects
7. MATERIALS AND METHODS :
7.1 SOURCE OF DATA :
The study will be conducted on patients with minimum of 50 in each group
5 i.e propofol alone, ketamine alone and ketofol aged between18 to 60 years posted for short surgical procedures at Bapuji Hospital and Chigateri General Hospital attached to JJM medical college Davanagere.
7.2 METHODS FOR COLLECTION OF DATA :
A minimum of 50 patients in each group will be selected randomly after taking informed written consent from the relatives.
All patients will be pre medicated.
Patients will be randomly allocated into 3 groups.
Group P-Propofol Group.
Group K – Ketamine group.
Group KP- Combination (ketamine+propofol=ketofol) group.
Inclusion Criteria
Age group between 18 to 60 years Both sexes ASA I, II & III Patient scheduled for short surgical procedures lasting for about 20 min- utes.
6 Patients who have not eaten solid food within 8 hours before or liquids in the two hours before
Exclusion Criteria
An acute lung infection Procedures involving stimulation of the posterior pharynx Coronary heart disease, CHD, and angina or suspected aortic dissec- tion History of uncontrolled hypertension or BP > 140/90mmHg Injury cerebral focal neurological deficit or loss of consciousness Mass in CNS, hydrocephalus or other conditions with increased in- tracranial pressure. Glaucoma or eye damage Prior hyperthyroidism or thyroid hormone replacement Pregnancy or lactation Major psychiatric disorder Previous mild allergic reaction to ketamine, propofol, lidocaine, or egg albumin Patient who refuses to provide informed consent
Procedure:
A prospective, randomised, single blind study will be undertaken Patients will be randomly allocated into 3 groups.
A minimum of 50 patients in each group will be selected randomly after taking informed written consent from the patients.
7 Patients will be randomly allocated into 3 groups
Group P-Propofol Group will receive a Loading dose-2mg/kg body weight.
Group K – Ketamine group will receive a loading dose of 2mg/kg body weight
Group KP- Combination (ketofol) group will receive a dose of ketamine 0.5mg/kg bodyweight
Followed by Propofol 2mg/kg bodyweight
IV line secured and patients will be connected to monitor to record pulse,
NIBP, ECG and SpO2.
Pre medication will be done with injection Glycopyrrolate 0.2mg i.v, Pentazocine
30mg i.v, & Midzolam 1mg i.v.
Patient will be preoxygenated with 100% oxygen for 3 minutes
The allocated group will receive the specific drug intravenously.
Following this below mentioned parameters were documented
Onset of action, Duration , Quality of analgesia, Cardiorespiratory stability, any adverse effects like vomiting, emergence phenomenon, Recovery at 1min, 5mins, 15mins. 30 mins, and the end of the procedure.
Assessment tools:
Assessment will be done based on the following scores
Onset of Induction
Taken by the absence of eyelash reflex/ loss of verbal contact
Analgesic score
8 Measured by four point scale by CAMERON et al
0: no pain,
1: mild pain(grimace),
2: moderate pain (grimace + cry),
3: severe pain (cry + withdrawal). Apnoea Defined as absence of spontaneous respiration for > 20 seconds Recovery score Evaluated using Aldrete score (1-10)
Safety will be assessed by monitoring laboratory test results, vital signs, ECG findings, physical examination findings, withdrawal related events and adverse events. Quantitative data will be analysed by suitable statistical tests like chi square test, ANOVA test, unpaired t test etc..
7.3 Does the study require any investigations or interventions to be conducted on patients or other humans or animals? If so, please describe briefly.
Yes, on Patients.
Investigations:
9 Blood:
Haemoglobin %, Total Count , Differential count.
Random Blood Sugar (RBS), Blood Urea, Serum creatinine
ECG
HIV and HBsAg
Chest X Ray
Urine :
albumin, sugar, microscopy
7.4 Has the ethical clearance been obtained from your institution in case of 7.3?
Yes,
Approval from the ethical committee of J.J.M Medical College, Davangere has been taken. Side effects of the drugs will be clearly explained to the patients in the local language and consent will be taken.
8. LIST OF REFERENCES:
1. Henrik Eikaas and Johan Raeder; Total intravenous anaesthesia techniques for ambulatory surgery; Current Opinion in Anaesthesiology; 2009,22:725–729 2. Sukhminder Jit Singh Bajwa,, Sukhwinder Kaur Bajwa1, Jasbir Kaur :Comparison of two drug combinations in total intravenous anesthesia: Propofol–ketamine and propofol–fentanyl Vol. 4, Issue 2, May-August 2010:72-79 3. Gamal T. Yousef, Khalid M. Elsayed: A clinical comparison of ketofol (ketamine
10 andpropofol admixture) versus propofol as an inductionagent on quality of laryngeal mask airway insertionand hemodynamic stability in children: Anesthesia: Essays and Researches; 7(2); May-Aug 2013 4. Bassett KE, Anderson JL, Pribble CG, Guenther E. Propofol for procedural sedation in children in the emergency department. Ann Emerg Med 2003;42:773-82.
5. Arora S. Combining ketamine and propofol (ketofol) for emergencydepartment procedural sedation and analgesia: A review. West J Emerg Med 2008;9:20-3. 6. Strayer RJ, Nelson LS. Adverse events associated with ketamine for procedural sedation in adults. Am J Emerg Med 2008;26:985-1028. 7. Morgan GE, Mikhail MS, Murray MJ. Nonvolatile anesthetic agents. Clin Anesthesiology 2002;8:151-77. 8. Nathan JS, Michael LB, Thomas MD, Matthew DK. Ketofol as a Sole Induction Agent is Associated with Increased Hemodynamic Indices in Low-Risk Patients. ASA abstracts 2011;16:A485. 9. Kalpana S. Vora, Prabodhachandran M.S., Guruprasad P. Bhosale, Neeta Singhal, Geeta P. Parikh, Veena R. Shah: Comparison of Admixtures of Propofol- Thiopentone, Propofol-Ketamine and Propofol in Ambulatory Surgery: J Anaesth Clin Pharmacol 2005; 21(4) : 413-418. 10. T.W Hui, T G Short, W Hong,m T Suen, T Gin, J Plummer. Additive interactions between propofol and ketamine when used for anaesthesia induction in female patients. Anesthesiology 1995; 82: 641-647. 11. Guit JBM, Koning H M, Coster M C, Neimejer R P E, Mackie D P. Ketamine as analgesia for total intravenous anaesthesia with propofol. Anaesthesia 1990; 46: 24- 27. 12. Kaushik Saha, M Saigopal, Rajini Sundar, M palaniappan, Anil C Mathew. Comparative evaluation of propofol-ketamine and propofol-fentanyl in minor surgery. Ind. J. Anaesth 2001; 45(2): 100-103. 13. Dr. Uma Srivastava1 Dr. Neeraj Sharma2 Dr. Aditya Kumar3 Dr. Surekha Saxena small dose propofol or ketamine as an alternative to midazolam co-induction to propofol :Indian J. Anaesth. 2006; 50 (2) : 112 – 114
14. Thomas MC, Jennett-Reznek AM, Patanwala AE. Combination of ketamine and propofol versus either agent alone for procedural sedation in the emergency department. Am J Health Syst Pharm . 2011 Dec 1;68(23):2248-56.
11 15. Samit Kumar Khutia, Mohan C Mandal, Sabyasachi Das, and SR Basu Intravenous infusion of ketamine-propofol can be an alternative to intravenous infusion of fentanyl-propofol for deep sedation and analgesia in paediatric patients undergoing emergency short surgical procedures; Indian J Anaesth. 2012 Mar-Apr; 56(2): 145–150. 16. Goh PK, Chiu CL, Wang CY, Chan YK, Loo PL. Randomized double-blind comparison of ketamine-propofol, fentanyl-propofol and propofol-saline on haemodynamics and laryngeal mask airway insertion conditions. Anaesth Intensive Care. 2005 Apr;33(2):223-8.
17. Atashkhoyi S, Negargar S, Hatami-Marandi P. Effects of the addition of low-dose ketamine to propofol-fentanyl anaesthesia during diagnostic gynaecological laparoscopy. Eur J Obstet Gynecol Reprod Biol. 2013 Aug;170(1):247-50
12 9. SIGNATURE OF THE CANDI- DATE
10. REMARKS OF THE GUIDE The present study is undertaken to evaluate the effectiveness of combination of two drugs (propofol+ketamine) with respect to quality of analgesia, duration & cardiorespiratory stability in short surgeries .
DR. RAVISHANKAR R B 11. NAME & DESIGNATION MD.DA. Professor, 11.1 GUIDE Department Of Anaesthesiology, J.J.M Medical College, Davanagere- 577004
11.2 SIGNATURE
11.3 CO-GUIDE (If any) -
11.4 SIGNATURE -
DR. MANJUNATH JAJOOR., 11.5 HEAD OF THE DEPART- M.D., D.A. Professor and Head, MENT Department Of Anaesthesiology, J.J.M Medical College, Davanagere- 577004
11.6 SIGNATURE
12 REMARKS OF THE CHAIRMAN & PRINCIPAL
12.1 SIGNATURE
13