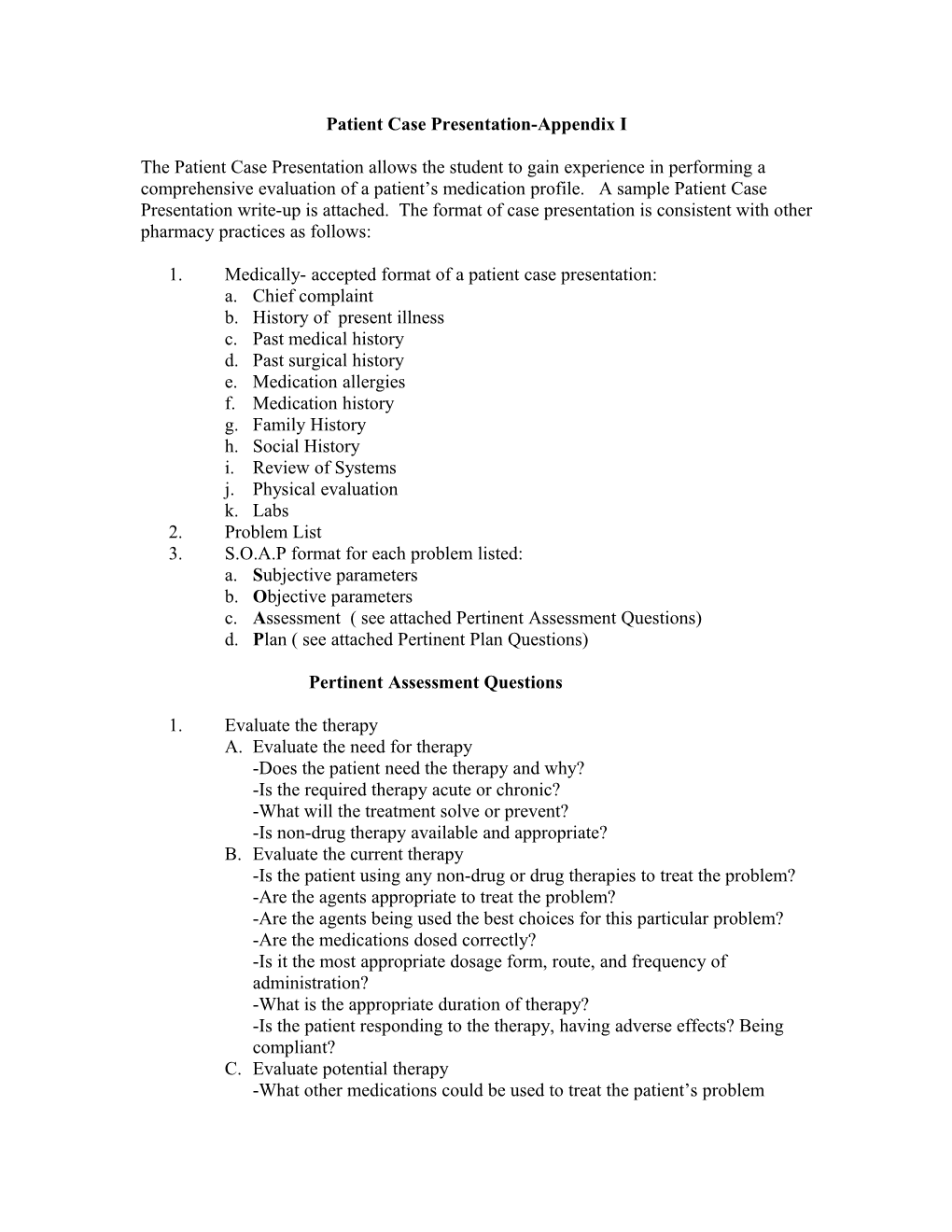
Patient Case Presentation-Appendix I
The Patient Case Presentation allows the student to gain experience in performing a comprehensive evaluation of a patient’s medication profile. A sample Patient Case Presentation write-up is attached. The format of case presentation is consistent with other pharmacy practices as follows:
1. Medically- accepted format of a patient case presentation: a. Chief complaint b. History of present illness c. Past medical history d. Past surgical history e. Medication allergies f. Medication history g. Family History h. Social History i. Review of Systems j. Physical evaluation k. Labs 2. Problem List 3. S.O.A.P format for each problem listed: a. Subjective parameters b. Objective parameters c. Assessment ( see attached Pertinent Assessment Questions) d. Plan ( see attached Pertinent Plan Questions)
Pertinent Assessment Questions
1. Evaluate the therapy A. Evaluate the need for therapy -Does the patient need the therapy and why? -Is the required therapy acute or chronic? -What will the treatment solve or prevent? -Is non-drug therapy available and appropriate? B. Evaluate the current therapy -Is the patient using any non-drug or drug therapies to treat the problem? -Are the agents appropriate to treat the problem? -Are the agents being used the best choices for this particular problem? -Are the medications dosed correctly? -Is it the most appropriate dosage form, route, and frequency of administration? -What is the appropriate duration of therapy? -Is the patient responding to the therapy, having adverse effects? Being compliant? C. Evaluate potential therapy -What other medications could be used to treat the patient’s problem -How do they compare to the current therapy? -How do they compare to one another? -Why are the other therapies less suited for the patient, or not recommend?
Pertinent Plan Questions
1. Recommendations A. Recommended therapy -Current therapy: continue and adjust if needed or discontinue -New therapy: provide drug, dose, route, frequency, duration -Non-drug therapy: Include lifestyle-changes B. Drugs to be avoided -Medications to be avoided and why? C. Further Test/ Follow-up -Test necessary for baseline evaluation of problem or medication to be used -When should the patient be re-evaluated? 2. Goals and monitoring parameters (toxic and therapeutic) A. Goals -Long term goal for the problem, specific for the patient -Include cure, relief, and control of disease and associated symptoms -Include prevention of complications of disease and adverse medication events B. Monitoring Parameters Therapeutics -Disease state -signs and symptoms for progression/ resolution -tests to monitor disease progression/ resolution and frequency of testing -Endpoints for therapy (when should you discontinue or change therapy?) -Medications -appropriate blood concentrations -appropriate alterations in laboratory values C. Monitoring Parameters Toxic -Medications -Side effects of medications -Potential drug-drug interactions III. Patient Education -Use lay language to communicate the following to the patient: -Disease state and needs for medications -Medication information including name, dose, route, frequency, duration, indication, precautions, potential side effects, proper storage -Medications to avoid (OTC) -Drug-food interactions -Non-drug therapies including life-style changes