Draft 16.11.12
Draft Policy on National Criteria to Access Services for Children and Young People with Disabilities
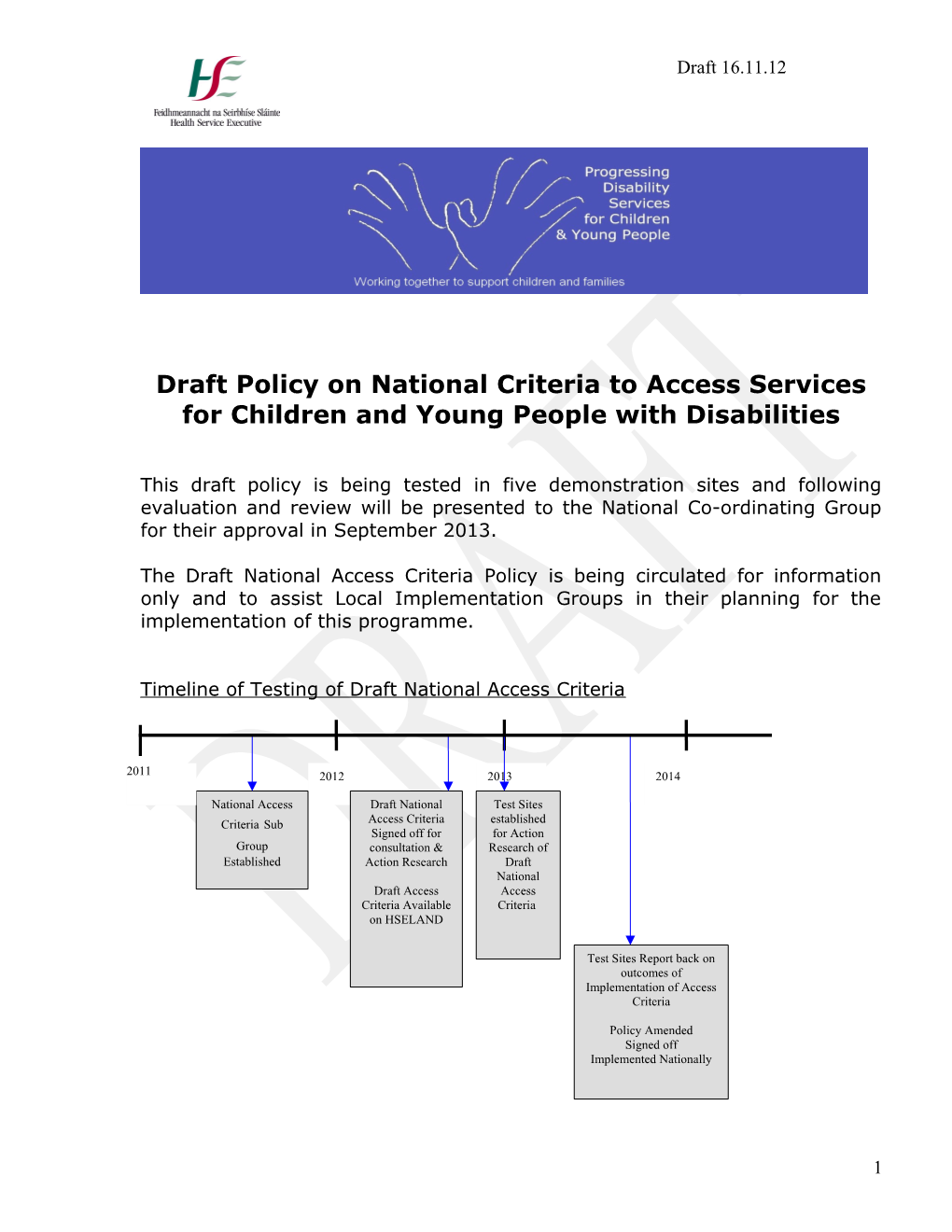
This draft policy is being tested in five demonstration sites and following evaluation and review will be presented to the National Co-ordinating Group for their approval in September 2013.
The Draft National Access Criteria Policy is being circulated for information only and to assist Local Implementation Groups in their planning for the implementation of this programme.
Timeline of Testing of Draft National Access Criteria
2011 2012 2013 2014
National Access Draft National Test Sites Criteria Sub Access Criteria established Signed off for for Action Group consultation & Research of Established Action Research Draft National Draft Access Access Criteria Available Criteria on HSELAND
Test Sites Report back on outcomes of Implementation of Access Criteria
Policy Amended Signed off Implemented Nationally
1 Draft 16.11.12
Access Criteria Working Group
This policy was developed by the Access Criteria Working Group convened by the National Co-ordinating Group of the Progressing Disability Services for Children & Young People programme.
Terms of reference
1. To provide advice to the National Co-ordinating Group in relation to a proposed national directive on criteria for access to primary care, network disability teams and specialist disability services for children with disabilities.
2. To consult with key stakeholders on the proposed criteria, including through the channel of the National Co-ordinating Group
3. To identify a review date for any national directive issued
4. To establish a glossary of terms for the purpose of common understanding
Members of the Access Criteria Working Group Barbara Bolger, Health Service Executive Regional Specialist Primary Care Caroline Cantan, Programme Co-ordinator Progressing Disability Services for Children & Young People Carol Cuffe, General Manager Health Service Executive Dublin South West Kildare West Wicklow Mary Fitzgerald, Co-Ordinator Regional ASD Services Brothers of Charity Cork Owen Hensey, Consultant Paediatrician Children’s University Hospital Temple Street and Medical Director Central Remedial Clinic Denise Keoghan, Performance & Development Health Service Executive Dublin Mid Leinster Aisling Lenihan, Early Intervention Lead Cork Health Area Penny O’Connell, Children’s Disability Services Co-ordinator Meath Aoife Thornton, Inclusion Ireland Parent Representative
2 Draft 16.11.12
Maria Walls, Director of Research & Policy Development National Federation of Voluntary Bodies
Acknowledgements The Access Criteria Subgroup wish to thank all parents and health & education professionals who contributed directly or indirectly to this document by submitting and sharing their work:
Contents
Page Number 1. Introduction 4
2. Purpose & Scope 5
3. Relevant Legislation, Reports & PPPG’s 5
4. National Access Criteria to Children’s Disability Services 6
Figure 1 Referral Pathway 8
5. Glossary of Abbreviations & Definitions 10
6. Description of Levels of Service 14
7. Roles & responsibilities 17
8. Proposed Process 17
Figure 2 Children’s Disability Services Forum 20
9. Audit & Review 21
10. Implementation Plan 21
11. Appendices 21
3 Draft 16.11.12
1.0 Introduction
1.1 Aims and objectives of Progressing Disability Services for Children & Young People are as follows:
One clear pathway to services for all children and young people with a disability, focusing on the needs of the child/young person and their family
Effective range of teams, across all levels of service delivery, working in partnership with parents, children & young people: Level 1 Primary Care Teams Level 2 Children’s Network Disability Teams Level 3 Children’s Specialist Disability Services Level 4 Tertiary & Acute Services
Resources used to the greatest benefit for all children, young people and families.
1.2 The above aims and objectives form the basis for this policy. A national directive on access to services criteria will drive consistency and equity, and will support the developing structure of service delivery under this programme.
The Report of the Reference Group on Multidisciplinary Services for Children aged 5 to 18 Years (2009) forms the policy basis to this programme of change in children’s disability services. The Reference Group was asked to make recommendations on preferred models and a framework for the future development of service delivery. The Group recommended a structure whereby children and their families would receive services and supports at the closest level to their home as appropriate to their needs.
1.3 The current economic environment and other factors beyond the control of local implementation groups and services make it extremely challenging to fully implement this structure. Services must also manage other pressures including compliance with the Disability Act 2005. However, the objectives of using our resources in the most effective way for the benefit of children and families according to the principles of this framework will provide us with strong foundations on which to build.
1.4 Principles The principles underpinning services, as agreed by the local implementation group and guided by the Guidelines for local implementation groups on developing a governance structure and policies for children’s disability1, should inform all access criteria to services.
1 Guidelines for local implementation groups on developing a governance structure and policies for children’s disability services. See Progressing Children’s Disability Services on the Change Hub www.hseland.ie
4 Draft 16.11.12
2.0 Purpose and Scope
2.1 The purpose of this policy is to provide Regional and Local Implementation Groups and staff members working in Primary Care Teams, Children’s Network Disability Teams and Children’s Specialist Disability Services with criteria for access to services for children and young people with disabilities, to support consistency and clarity.
2.2 The scope of this policy is for: Regional and Local Implementation Groups for the Progressing Disability Services for Children & Young People programme to implement access criteria for their Health Areas when the network early intervention and school age teams are formed All staff members working within the three levels of service provision: Primary Care Teams, Children’s Network Disability Teams within the Health and Social Care Networks and Children’s Specialist Disability Services All those who refer children to disability services
3.0 Relevant Legislation, Reports and PPPGs
o The Report of the Reference Group on Multidisciplinary Services for Children aged 5 to 18 Years (2009) o Disability Act, 2005 o Trust In Care (2005), o Children First: National Guidelines for the Protection and Welfare of Children 2011, o The Protection of Persons Reporting Child Abuse Act (1998) o The Interim Guidelines on the Sharing of Information (2008) o HSE Confidentiality Policy
5 Draft 16.11.12
4.0 National Access Criteria to Children’s Disability Services
1.5 Determining services according to the child’s needs: Children will be seen at the level of service (Primary Care Team & HSCN, Network Disability Team or Specialist Disability Service) which will best address their needs.
Diagnosis plays an important role in determining a child’s needs and the intervention indicated. However diagnosis on its own does not determine the most appropriate service to meet those needs, and in the absence of diagnosis no child should be denied access to services.
Children’s needs for disability services do not exist in isolation from their other needs and the needs of their families (see Life Needs Model in Appendices). Shared pathways of services and supports should be arranged with the Children and Families Agency, Child and Adolescent Mental Health Services and the education sector for individual children and their families as appropriate.
The threshold for the child’s needs to meet eligibility for network disability teams will be determined by the range and extent of functional difficulties (i.e activity limitations and participation restrictions ) and the level of interdisciplinary supports needed as opposed to the number of impairments and the number of disciplines required to input.
If it is unclear as to the pathway for a child/young person, the local Children’s Disability Services Forum should decide where the child’s needs will be best met at any particular time. (See Section 8.4)
Geographic Areas: The geographic areas served by Primary Care Teams, Network Disability Teams and Specialist Disability services are specified nationally and the child’s residence will determine which HSE Health Area will provide health services. See Schedule Networks and PCT version 7 August 2012
1.6 Primary Care: The Primary Care Team will2 be the main provider of support for children with non complex difficulties in functional skills/applied skill sets required for activities of daily living, learning new skills and social interactions. This may involve physical, social, emotional, communication and behavioural needs.
It should be clearly demonstrable that these needs can be met on a uni- disciplinary basis or the multidisciplinary framework of a Primary Care Team.
2 411 teams are now in place with GP involvement and an additional 37 teams with GP yet to be involved, out of 489 planned teams.
6 Draft 16.11.12
For individual cases, a shared care arrangement may be agreed with the Children’s Network Disability Team or Children’s Specialist Disability Service as part of the plan of care for the child and family.
1.7 Children’s Network Disability Teams: Criteria to access Network Disability Services include the age of the child, home and school address and the needs of the child.
4.3.1 Age of child Early intervention services will be provided for children from birth up to the commencement of formal schooling allowing for a period of transition and support3. Transition to school age services should be appropriately planned in advance, and managed flexibly on an individual family centred basis. School age services will be provided for children from the time of transition from early intervention services at the stage of the commencement of formal schooling until their eighteenth birthday or where appropriate when they finish school.
4.3.2 Geographic area Early Intervention Teams - children will be seen by the Children’s Network Disability Team according to the address of their home. School Age Teams - where a child attends a school outside his Health Area, the home address Health Area will remain responsible for all the child’s services. Local arrangements for service delivery may be coordinated on an individual basis between the child’s Network Disability Team and the Network Disability Team where the school is based, or on a broader basis as agreed by local management.
4.3.3 Needs of Child and Family The Children’s Network Disability Teams will be the main provider of support for children and young people and their families who require a complexity of services and support which should be available through the skill mix within the interdisciplinary network team. Evidence must be demonstrated with the referral that the child has this level of needs through diagnosed disability, objective measurement, screening tools and health or education professional reports. Standardised referral and screening processes will be decided nationally following the learning from the pilot of this policy. In the case of parental referrals, the referral form may be completed by them in conjunction with a primary care clinician, GP or network disability team member.
3 This can be defined by the team
7 Draft 16.11.12
It should be clearly demonstrable that these needs cannot be met within the uni-disciplinary basis or multidisciplinary framework of a primary care service. Children with complex needs will receive the majority of supports at Network level but have short term access to Primary Care and Specialist Disability level care pathways where this is appropriate to their needs.
1.8 Children’s Specialist Disability Services may operate at Health Area, national and/or regional service level and will provide the specialised expertise that some children, young people and their families require.
. The role of Children’s Specialist Disability Services is to support to the Children’s Network Disability Teams and Primary Care Teams, who will remain the main service provider for the child with disability and their family. . Specialist services may involve addressing physical, social, emotional, communication and behavioural needs which in many cases require linkages with ISA/Regional and/or national medical specialties. . Individual plans will be required for children who require access to Specialist Disability Services. . It should be clearly demonstrable that these needs can not be met solely within a uni-disciplinary basis or multidisciplinary framework of a primary care team or solely by a Network level team.
8 Draft 16.11.12
Figure 1. Referral Pathway
Referrers*
*Referrers: Include Parents/legal guardians, health and social care professionals, hospitals, education professionals, assessment officers and case managers. All referrals must be accompanied by signed consent by parent/legal guardian. 1 l e v e **Population: The number of children accessing the different levels depends on the L Criteria: Children with non-complex Primary needs.child population in the area (see Census 2011 figures) and prevalence rates. A prevalence rate of 4% is suggested toCare be used as an estimate of the number of children with complex needs in an area.Teams Criteria: Diagnosis of 2
l condition e
v associated with e
L complex needs or Criteria: Children with complex. Children’s Network complex needs needs Disability Teams identified by screening reports 5.0 Glossary of Abbreviations and Definitions
This is a glossary of terms used in this document and also of terms used currently in 3
l some services. The pilot phase will generate additional terms and defnitions e v e L Criteria: ConsultationAbbreviations and short Children’s term intervention for children who Specialist require specialist expertise Disability Services CTM Clinical Team Meetings GP - General Practitioner HOD - Heads of Discipline HSCN - Health and Social Care Network OT - Occupational Therapy PCT – Primary Care Team PCSDO- Primary Care Service Development Officer PHN - Public Health Nursing PT - Physiotherapy PN - Practice Nurse SLT - Speech and Language Therapy SW - Social Work HA - Health Area MDVI - Multi-disabled and visually impaired FSW _ Family Support Worker
9 Draft 16.11.12
HT Home Teacher NCSE - National Council for Special Education SENO - Special Education Needs Organiser
Definitions 1.9 Access to Service Criteria: A statement of the criteria by which it will be judged which is the appropriate service to meet the child’s needs
1.10 Activity and participation Activity is the execution of a task or action by an individual. Participation is involvement in a life situation. Activity limitations are difficulties an individual may have in executing activities. The ICF- CY (International Classification of Functioning, Disability and Health: Children and Youth Version) includes learning and applying knowledge, general tasks and demands, communication, mobility and self care as functional skill domains within which functional skill deficits/activity limitations occur. Participation restrictions are problems an individual may experience in involvement in life situations. During childhood and adolescence, limitations and restrictions may also take the form of delays or lags in the
emergence of activities and participation. The ICF-CY includes the following domains whereby participation restrictions may be experienced: domestic life, interpersonal interactions and relationships, major life areas and community, social and civic life.
1.11 Assessment: The evaluation of the developmental status and intervention needs of a child/young person and family.
1.12 Child/Family Plan: A child/family plan is developed by the team with the child/young person and family. It documents and guides the goals identified by the family and team, the intervention process for children and their families and the delivery of services and supports. It will contain information about the services being offered to facilitate a child’s development and enhance the family’s capabilities both to care for the child and to facilitate the child’s development.
1.13 Complex and Non Complex Needs
Non Complex Needs refers to one or more impairments giving rise to functional difficulties which result in mild restrictions in participation in normal daily living. It may also refer to children with moderate functional difficulties
10 Draft 16.11.12
which are likely to be mitigated by unidisciplinary or primary care team level supports.
Interventions: Children with Non Complex Needs will receive their interventions and support at the Primary Care Team level.
Complex Needs: Complex Needs refers to one or more impairments which contribute to a range of functional skill deficits and give rise to significant activity limitations or at least moderate restrictions in participation in normal daily living activities and interactions. The child with complex needs and their family will require additional supports in terms of key working, interdisciplinary management and or medical supports to mitigate secondary impairments and their challenges in terms of environmental and personal factors.
Interventions: Children with Complex Needs will receive their interventions and support at the Network Disability Team level.
Changes in Complexity: Children may receive their services and supports at different levels of service as the complexity of their needs changes over time.
1.14 Discharge: This occurs when a child fulfils any of the following:
Is no longer in need of a service, Has reached full potential as appropriate to their age, Has withdrawn from the service or has attained the age of 18
In circumstances where the relevant health professional has determined that the child requires no further intervention, then (a) the parents/guardians and (b) the initial referrer should be advised in writing that the intervention is at an end and that if the child’s condition or developmental progress gives any cause for concern they should contact the service to seek advice or request a review. This should not be confused with transfer between services e.g. from Primary Care or Early Intervention to School Aged teams.
Inactive or Dormant Status: If service users are given the status of inactive or dormant the service still has a duty to be actively involved. If no intervention or review is needed, offered or accepted, Duty of Care would indicate that after a certain time the child should be discharged or referred
11 Draft 16.11.12
onwards if appropriate. Parents/guardians should be informed that a re- referral is available on request. Inactive or dormant status retained for a very long time could be in breach of the Data Protection Act. Rule 5 is Keep it accurate and up to date and Rule 7 is Retain it for no longer than is necessary for the purpose or purposes.
1.15 Duty of Care: Duty of Care is defined as taking responsible care to avoid any acts or omissions which could reasonably be foreseen and would be likely to injure another individual. In processing referrals and offering services the interests and welfare of the child should be paramount at all times. From the time the child is referred to a service, the service has obligations and duties to that child. There is a duty to move with reasonable dispatch in providing a screening assessment to determine if the service is the most appropriate one to meet the child’s identified needs. Please refer to Inactive or Dormant Status above in 5.6.
1.16 Family-Centred Service: Family-Centred Service is a method of service delivery that: Recognises parents as the experts on their child’s abilities and needs Promotes partnerships between parents and service providers Supports the family’s role in decision-making about services for their child (Rosenbaum, King, Law, King & Evans, 1998; Shelton & Stepanek, 1995)
1.17 Foundation Skills: Single skills that allow a child to function in meaningful ways in their environment, such as mobility (King at al)
1.18 Functional Skills: ‘Applied skill sets related to day-to-day function in the real world (i.e., higher order, composite skills that enable a child to function confidently and competently in real life settings). Applied skill sets reflect the integrated application of foundational skill and reflect mastery across different situations and contexts’ (King et al). An example provided by King at al is the functional/applied skill set of social competency which results from the application of several foundation skills, including listening skills and understanding social rules.
1.19 Health Areas: The delivery of health services is currently divided into 17 Health Areas and 126 Health and Social Care Networks. (See Schedule Networks and PCTs v.7 August 2012) for a list of these.
ICF-CY International Classification of Functioning, Disability and Health: Children and Youth Version. The ICF-CY is intended for use by clinicians, educators, policy makers, family members, consumers and researchers to document characteristics of health and functioning in children and youth.
12 Draft 16.11.12
The ICF-CY is intended as the broad framework for the access criteria: each health service area will have to agree referral forms , screening tools and or assessments which provide a practical methodology to implement this access framework.
For further detail on ICF-CY see appendix.
1.20 Impairments: Loss, abnormality or deviation from the norm in body structure or physiological function (including mental functions)
1.21 Interdisciplinary: An interdisciplinary team is a number of professionals from different disciplines who work together and share information, decision-making and goal-setting. They have common procedures and policies and frequent opportunities for communication. They work with the family and child or young person, who are all seen as part of the team, to meet their identified needs with a joint service plan.
1.22 Multidisciplinary Team: A multidisciplinary team is a group of professionals from diverse disciplines who come together to provide comprehensive assessment and consultation. While their primary purpose is typically to help team members resolve difficult cases, teams may fulfil a variety of additional functions. They can promote coordination; provide a "checks and balances" mechanism to ensure that the interests and rights of all concerned parties are
addressed; and identify service gaps and breakdowns in coordination or communication between agencies or individuals. They also enhance the professional skills and knowledge of individual team members by providing a forum for learning more about the strategies, resources, and approaches used by various disciplines.
1.23 Network: A Network refers to Health and Social Care Networks as defined by the HSE. See Description of Service Levels for further information. See appendix X for National Map of all Health & Social Care Networks.
1.24 Plan of Care (Primary Care): A Plan of Care is defined as a document developed after the person is discussed at a Primary Care Team Clinical Team Meeting that identifies the actions to be taken in response to identified needs, the timeframe for implementation and the responsible person/s.
1.25 Primary Care Team (PCT) is a team of health professionals who work closely together to meet the needs of the people living in the
13 Draft 16.11.12
community. They provide a single point of contact to the health system for the person. The Primary Care Team members also link with other community- based disciplines to ensure all health and social needs are provided for.
1.26 Referral: Children aged 0 – 18 years referred for consideration of access to the service, assessment and possible admission to services. Parent/guardians, health professionals or other relevant professionals may make referrals.
1.27 Screening Assessment: An assessment to establish the appropriate service for the child and family.
1.28 Urgent and Non Urgent referrals & Prioritisation: Children should normally be seen in order of date of referral.
An urgent referral may include the following:
Medical health risk to the child, Risk of home placement breaking down, Risk of school placement breaking down.
Any prioritisation policy must be clearly documented, linked to policies in Child and Family Services and Primary Care and other relevant services and made available for parents and referrers.
1.29 Waiting List: Names of children should only be placed on a service waiting list after the relevant screening process has identified the service as being appropriate to meet their identified needs and where services are not readily available. Full and accurate records should be kept of waiting lists; the design of the waiting list, weighting systems, and waiting list reviews. Parents and
referrers should be fully advised of same and made aware of the status of the wait list following a review. Duty of Care dictates that once a child and family have been offered services or the child’s name placed on the waiting list, there is a commitment to provide a service, be in regular contact and keep the parents/guardians informed of their status. This duty and responsibility continues until the child is transferred or discharged from the service. A child should not be transferred to another service straight from a waiting list without their current needs being reviewed following consultation with the family.
14 Draft 16.11.12
6.0 Description of Levels of Service
1.30 Primary Care: A Primary Care Team (PCT) is a multidisciplinary team of healthcare professionals who work together to meet the health and social care needs of
defined population of between 7,000-10,000 Othe people (see Figure 1). All the health care GP r professionals on the team work together to PHN develop individualised plans of care Phy incorporating support for people particularly SW those with chronic illnesses and other complex OT needs. They share information and their HH respective skills to ensure that people with the SLT greatest need receive services in a timely and Cor coordinated way. eExtended
Primary care clinicians in order to provide services for children with disabilities need to have skills in screening and paediatric therapy. Screening tools need to be agreed nationally to assist this piece. In relation to therapy services, rotation of basic grade clinicians into posts in disability team is recommended to extend knowledge and experience.
1.31 Health and Social Care Integrated Networks: The Primary Care strategy defines Services “Health & Social Care Network Services (HSCN)” Multi as a wider network of additional professionals Agencies Hospitals Children’s Network who … provide the therapy services required by a Disability Early
InterventionPCT TeamPCT number of core primary care teams (See figure ‘E’ ‘B’ Children’s 2). Formal communication processes will be Specialist
Disability PCT established between the core Primary Care Teams Service PCT ‘C’ ‘D’ and the wider HSCN professionals. Health & Private Providers Integrated Social Care Network Areas are defined by Specialist Services boundaries and encompass a number of primary Children’s Network Disability School Age care teams serving a population of 30,000 – Team 60,000 people. Voluntary
1.32 Children’s Network Disability Teams: Network Disability Teams will be established Voluntary within defined geographic areas i.e. Health and • Support Social Care Networks. They will be formed to address the needs of children with a wide range of disabilities including but not limited to, intellectual disability, physical disability, sensory disability and autism.
15 Draft 16.11.12
The team members should work within an interdisciplinary team model, contributing to a joint integrated plan for each child, young person & family. The family will always be seen as part of the network disability team.
Children’s Network Disability Services incorporate Early Intervention and School Aged Teams and should be co-located to allow for effective provision of services.
The Children’s Network Disability Teams and Primary Care Teams should Multi develop clear protocols for the effective transition of children between Agencies services when appropriate. • Private 1.33 Children’s Specialist Disability Services may operate at Health Area, national and/or regional service level and will provide the highly specialised expertise that some children, young people and their families require. The role of Children’s Specialist Disability Services is to support to the Children’s Network Disability Teams and Primary Care Teams, who will remain the main service provider for the child with disability and their family.
This role will also include the development and promotion of specialist skills and knowledge in team members, in line with current best practice. Specialist Disability Services will disseminate knowledge through consultation and training, and provide direct assessment and intervention when required, ideally on a short-term basis. The distribution and number of Specialist Disability services required ultimately be determined by the prevalence of specific conditions which require such services and supports in the area, and by available resources.
These specialist services are considered essential in order to maintain quality based and effectively delivered health services.
The following are the main themes which should be considered and these points should be used as a benchmark for Children’s Specialist Disability Services providers:
The staff providing the Specialist Disability Service have a level of experience and training above and beyond that available in a Primary Care Team level and at Network Disability Services level. This training often includes a post graduate qualification and specialist training. In addition, a number of individual staff members will be acknowledged and known by their peers as being experts in the
field e.g. medical and orthopaedic consultants, behaviour support and clinical specialists.
The service has the necessary critical number of children and young people with specific diagnoses and throughput to enable staff to develop and maintain necessary expertise. Children and young people with complex but low incidence
16 Draft 16.11.12
conditions, not commonly seen in the community, may be referred with a query or for an opinion which has not been answerable by a local team. The staff are in a position to provide second opinions when required Team members with specific expertise in an area work together as a multidisciplinary team to provide services for children & young people who have specific areas of need or a specific diagnosis. Referrals are often made because a full team review is not available locally. Staff have close links with Academic Institutions, Professional Organisations and Paediatric Hospitals. These links are supported by their Specialist Disability organisation ensuring that staff and teams maintain a high level of knowledge and skills in specific conditions and keep up to date with current evidence based best practice. Staff are sufficiently skilled that they are in a position to act as a clinical resource for their colleagues on a national and/or regional and/or local basis, providing mentoring, advice and formal training in management of specific clinical conditions and areas of need. The Children’s Specialist Disability Services, collaborating with local Primary Care and Network Disability Teams, promote best practice initiatives. The service is in a position to promote and lead research in a given care area.
7.0 Roles and Responsibilities
It is the responsibility of Management of Children’s Disability Services 0-18 years to do the following:
Implement the national access criteria as soon as the appropriate structures are in place.
17 Draft 16.11.12
Inform all stakeholders in Children’s Disability Services including parents, health professionals and other referrers as appropriate Ensure staff work within the framework of the access criteria Ensure staff receive training as appropriate to provide a service within the framework of the access criteria
8.0 Proposed Process
1.34 Primary Care Teams will use agreed screening tools to identify children and young people with a developmental delay/disability. Voluntary Where there are two and more disciplines involved with the child and young person and their family, the practitioner will seek the consent of the family to discuss the individual case with the other PCT practitioners. The individual case will be scheduled for a Clinical Team Meeting (CTM). Following discussion at the CTM, a referral may be made to the Children’s Network Disability Team and/or a Plan of Care devised. The PCT Practitioner may contact the Children’s Network Disability Team for advice prior to referral.
1.35 Primary Care Teams will: Primarily provide interventions and support for children and young people with non complex needs. For individual children and young people, with complex needs, the PCT may provide a service in support of a shared Individual Plan agreed with the Children’s Network Disability Team.
1.36 Children’s Network Disability Services will screen all appropriate referrals. Referrals will be by standard application form with signed parental consent. • Support
Referrals to Children’s Network Disability Services may be received from a number of sources including parents, guardians and health professionals. Referrals should be accompanied by all evidence of complex • Support needs including reports, information from parents, assessment & screening tools
Children with an identified disability at birth or high risk of disability may directly access the Children’s Network Disability Teams until such time as the child and family’s support needs may be deemed non complex.
Changes in Complexity: Children’s services can be transferred between the various levels of service as the complexity of their needs changes over time.
1.37 Primary Care Teams and/or Children’s Network Disability Teams may refer a child and young person to a Children’s Specialist Disability
18 Draft 16.11.12
Services for additional advice, support and direct intervention where necessary as part of a child’s individual plan.
Children’s Disability Services Forum (See Figure 2 ) 1.38 Local Disability Implementation Groups and/or the local governance group will agree the Children’s Disability Services Forum Model and ensure all agencies (HSE and Voluntary Organisations) are involved in planning and development. The Children’s Disability Services Forum will be responsible for a designated geographic area which covers designated Health and Social Care Network/ Cross Networks. It should be chaired by a Manager in Children’s Disability Services, and meet on a monthly basis. It will include representatives of Primary Care, Children’s Network Disability Teams, Children’s Specialist Disability Services, Community Paediatrician, education and other relevant services as needed.
The functions of the Children’s Disability Services Forum include: To act as a decision making forum on referrals where pathways or level of service is not clear. To make recommendations for shared care provision i.e. joint working across primary care, network disability team and disability specialist services where pathways or level of service is not clear. To identify shared goals for service developments.
19 Draft 16.11.12
Figure2. Children’s Disability Services Forum
20 Draft 16.11.12
9.0 Audit and Review
1.39 This National Access Criteria Policy and associated processes and procedures, including referral forms and screening tools should be reviewed annually.
10.0 Implementation Plan
1.40 The National Coordinating Group and the National Disability Governance Group on acceptance of this policy document will agree an implementation plan.
The policy will be tested in at least four HSE Area demonstration sites (one in each HSE Region) for a period of six months, followed by detailed evaluation.
This National Access Criteria should form part of the regional and local implementation plans for Progressing Disability Services for Children & Young People in each area.
11.0 Appendices
ICF diagram ……………………………………………………………………………..P 22 Life needs model ………………………………………………………………………P 23 Scenarios…………………………………………………………………………………..P 24 Childhood visual impairment…………………………………………………….P 34 National schedule primary care and HSCNs (Networks) ………..P 38
21 Draft 16.11.12
ICF _CY International Classification of Functioning, Disability and Health: Children and Youth Version
The ICF-CY is intended for use by clinicians, educators, policy makers, family members, consumers and researchers to document characteristics of health and functioning in children and youth. Training is required in the use of the ICF-CY before it can be implemented in a service.
The ICF- CY provides a means of categorising the child’s needs across the developmental stages in terms of; Body functions including psychological functions Body structures, Activities and participation of children and youth, Environmental & personal factors both facilitators and barriers to performance
The ICF-CY focuses on both the capacity and the performance of the individual, thus assisting in setting child and family centered service goals.
Categorising and coding children’s needs, using the ICF-CY must be based on-“primary information in the form of direct measurement, observation first-hand interview and/or professional judgment”.
Where standardised assessment instruments are not available or appropriate, qualitative information based on direct observation can be used to support coding of the child’s functioning.
The encouragement of first hand interview and observational assessment can facilitate child and family centered goal setting and promote the use of natural learning environments to facilitate service goals. It is consistent with a bio-psycho- social approach in that it recognises the dynamic interaction between impairment, environment and personal factors.
22 Draft 16.11.12
Life Needs Model
23 Draft 16.11.12
Sample Scenarios
Sarah Age 10 years Diagnosis if any - Referrer School Presenting difficulties Fine motor skills and handwriting and needs for services Teacher thinks OT needed as stated by referrer Further information School reports needed and suggested Vision test tools to measure function Level of service required Primary care assessment if needed, and handwriting group or individual handwriting programme for school and home Support from specialist Availability of training in DCD and dyspraxia for primary disability services care clinicians. Other services and Information - packs for parents and teachers, useful supports websites, community supports.
Richard Age 5 Diagnosis if any - Referrer School Presenting difficulties Poor social and communication skills and needs for services as stated by referrer
Further information Assessment in school to investigate possibility of bullying, needed and suggested shyness, separation difficulties tools to measure Social and Communication Questionnaire (SCQ) aged 4 function years and older Australia Scale for Asperger Syndrome (ASAS) age 5 years and older
Level of service required Primary care for screening assessment. Onward to network team if assessment reveals complex needs e.g. query ASD Support from specialist Training with screening assessments and processes services Support from ASD specialist as needed Other services and supports
24 Draft 16.11.12
Kate Age 8 years Diagnosis if any Severe/profound ID. CP. Epilepsy Referrer Previous service provider – has moved address Presenting difficulties Non verbal, self harming, very limited independent mobility, and needs for services epilepsy poorly controlled as stated by referrer Interdisciplinary team needed to meet complex needs
Further information Existing reports and assessments needed and suggested tools to measure function Level of service Network team. Link with special school/class. Family required support. Keyworker. Nurse Support from specialist Seating services Other services and Medical. Community information and supports supports
John Age 12 years Diagnosis if any Congenital blindness Referrer Parents Presenting difficulties Social isolation. Lacking social skills. Dependent. and needs for services as stated by referrer Needs social support, AT, mobility for visually impaired. Independent living skills
Further information Report from school needed and suggested tools to measure function Level of service Primary care OT required Support from specialist High tech AT, Child Vision and NCBI for independent living services and mobility skills Other services and National Braille Centre Drumcondra. Community information supports and supports
25 Draft 16.11.12
Jenny Age 18 months Diagnosis if any Hypoxic Ischemic Encephalopathy Referrer Hospital consultant Presenting difficulties Severe epilepsy. Spastic quadriplegia. Global developmental and needs for services delay. No suck/gag reflex. Life expectancy short. as stated by referrer Needs interdisciplinary team. Major support for family needed, including nursing and respite.
Further information Peabody Infant Sceening assessment needed and suggested Parent questionnaire that covers deeding, dressing, washing tools to measure and sensory info . Non- standardised function Observations Medical and other professional reports from hospital Level of service Network team. Family support, keyworker, dietician required Support from specialist Postural management, services Other services and Medical. Jack and Jill. Sunshine Home. Community supports information and supports
Kenneth Age 12 years Diagnosis if any Hydrocephalus, CP, epilepsy, cortical blindness, severe global developmental delay, osteoporosis Referrer Hospital consultant Presenting difficulties Non-verbal, feeding difficulties, bone injuries due to and needs for services osteoporosis as stated by referrer Interdisciplinary team needed. Support for long term foster parents. Further information Medical and professional reports needed and suggested tools to measure function Level of service Network team. Family support. Links with hospital team. required Links with special school. Nursing Support from specialist Visual impairment, postural management services Other services and Community information and supports supports
26 Draft 16.11.12
Conor Age 12 months Diagnosis if any CP hemiplegia. MRI signs of brain damage Referrer Hospital consultant Presenting difficulties and Increased tone on right side. Not yet standing or needs for services as crawling. stated by referrer Requires physiotherapy and occupational therapy
Further information Full reports from hospital needed and suggested Peabody Infant Screening Assessment tools to measure function Alberta Infant Motor Scales Observations Level of service required Network team. Full team assessment. Support for family around diagnosis. Equipment as needed. Long term might be referred to primary care if hemiplegia mild and non-complex, and no further need for team intervention with re-referral to Network Team if needed. Support from specialist Spasticity management as needed - orthotics, possible services Botox treatment in future, gait analysis, upper limb splinting Other services and Community information and supports supports
Ben Age 9 Months Diagnosis if any - Referrer AMO Presenting difficulties 1 hospitalisation for reflux ,history of croup, query convergent squint, difficulty sitting unsupported, not rolling from tummy to back, support needs for parents as sibling with ASD, delayed and limited babbling, some concerns re play and social skills development & poor fine motor skills. Needs for services as stated by Ophthalmologist, physiotherapy, speech and language referrer therapy, occupational therapy, psychology, paediatrician Further information needed Parent questionnaire that covers deeding, dressing, and suggested tools to washing and sensory info . Non- standardised measure function Peabody Infant Screening Assessment Sensory screening questionnaire for 0-12 months or the Infant/Toddler Sensory profile Play observations Level of service required Network Disability team Support from specialist Not indicated as yet needs can be met within the services network Other services and supports Community information and supports
27 Draft 16.11.12
Lee Age 7 Diagnosis if any SLI attended class for Specific language Impairment Referrer Parent initially to SLT service Presenting difficulties Expressive language difficulties Bereavement Needs for services as stated Severe speech and language difficulties at time of by referrer initial referral Further information needed School report and suggested tools to Discharge report from language class will provide measure function standardised and functional summary of need and will be supported by teachers report and other health professional reports
Level of service required Primary care SLT & Child and family psychology Support from specialist CAMHS if bereavement significant issue services Other services and supports Community information and supports
Caroline Age 15 Diagnosis if any Severe Specific Language Disorder attended class for SSLD for early years Referrer SLT Presenting difficulties Articulation Sensory processing Needs for services as stated PCC SLT for speech work and school supports PCC by referrer OT for further input on sensory processing. Further information needed School report and suggested tools to Discharge report from language class will provide measure function standardised and functional summary of need and will be supported by teachers report and other health professional reports
Level of service required Primary Care Support from specialist No services PCC services met needs
28 Draft 16.11.12
Mary Age 7 years Diagnosis if any Down Syndrome and a moderate level of intellectual disability. Referrer Parents Presenting difficulties Coping well in mainstream school with supports. Concerned that Mary has no friends and is bored in evenings and at the weekends. Needs for services as Community linker stated by referrer Further information Reports from parents and teachers needed and suggested tools to measure function Level of service required Network team member with community link work role/function to support parents in identifying extracurricular activities that will encourage the development of a natural support network and promote the development of friendships with peers in the community Support from specialist Not required services Information, supports Access to Downs Syndrome Ireland and community organisations
Tadhg Age 17 Diagnosis if any Autism, Mild ID, ADHD Referrer Network team Presenting difficulties Obsessive compulsive behaviours and Disruptive in class needs for services as Feelings of paranoia stated by referrer Self harming
Further information Report from school needed and suggested Update reports from network team tools to measure Connors Rating Scale function Depression Anxiety Stress Scale(DASS) Level of service required Network team for school support, SLT, OT, parental support Consult with ASD Specialist service Referral to CAMHS
29 Draft 16.11.12
Niamh Age 14 years Diagnosis if any Spina bifida. Mild impairment Referrer Children’s Network Disability Team Presenting difficulties Needs for services as stated Niamh has attended children’s disability services since by referrer she was a baby. Now she only requires orthotics and physiotherapy to monitor her function
Further information needed Clinical reports and suggested tools to Assessed as good range of movement, grade 4-5 muscle measure function power at hips and knees, grade 2 at ankles Level of service required Primary care. Niamh is independently mobile and has an average level of function in all areas. She does not require interdisciplinary team intervention. Support from specialist None required services Information, supports and Niamh is actively engaged in local social and leisure community organisations activities
30 Draft 16.11.12
Aaron Age 15 Diagnosis if any Severe Specific language disorder, motor planning and sensory processing disorder
Referrer SLT Presenting difficulties Severe expressive language disorder, severe literacy difficulties, severe motor planning, organisational difficulties and sensory processing difficulties, difficulty with peer relationships, motivation issues, attention difficulties Needs for services as stated NEPS review by referrer SLT OT Further information needed Asperger Syndrome Screening Questionnaire and suggested tools to Australia Scale for Asperger Syndrome (ASAS) measure function Social and Communication Questionnaire (SCQ) aged 4 years and older
Level of service required Network Disability School age team Support from specialist CAMHS as necessary pending recommendation of NEPS services review Information, supports and Parent support group for teenagers. community organisations Linkages with community youth groups
Oliver Age 3 years Diagnosis if any Referrer Mother Presenting difficulties Only 10 words, limited understanding and Does not eat much needs for services as Little interaction with peers stated by referrer Limited eye contact Anxious around change
Further information Parent questionnaire that covers feeding, dressing, needed and suggested washing and sensory information Non- standardised tools to measure Peabody Developmental Assessment function QCHAT aged 0-36 months Preschool report Level of service required Primary care SLT, Cognitive assessment and screening for ASD Referral to Network team if screening positive for ASD Support from specialist Not indicated as yet needs can be met within the network
31 Draft 16.11.12
services
Summary Working Paper to Access Criteria Working Group
Specialist services for children with a visual impairment & summary of limited data on prevalence rates and of trends in recent aetiological data re childhood visual impairment
Aoife Thornton
Specialists for children with a visual impairment:-
1. National Council for the Blind (Whitworth Road, Dublin 9) 2. Child Vision (formerly St. Joseph’s Centre for the Visually Impaired) (Dublin 9)
National Council for the Blind The NCBI provides regionally based supports to children (and adults) with a visual impairment or blindness in the areas of:- Mobility training Training in use of low-vision aids
32 Draft 16.11.12
Supply and support of technology aids for the classroom Training in use of educational technology aids Family support via Community Resource Workers
Child Vision In addition to its campus based local service provision in Dublin (with limited service based in Cork), Child Vision currently provides specialist supports to children with a visual impairment and blindness, and their families, nationally (currently 595 clients, 433 via outreach), in the areas of:- Assessment of Needs*, including o multi-disciplinary/multi agency co-assessment (e.g. functional vision experts in Child Vision working on a particular issue with Assistive Technology experts from CRC) Therapies consultation (physiotherapy, S&L therapy, OT) with children’s local service providers, initially and periodically incorporating direct therapeutic engagement with child Provision of advice on vision impairment/blindness and its implications for daily living, and for development, in particular with regard to children with multiple disabilities including vi [MDVI] in child-specific cases and via on- campus formal training seminars Training, education and activities for parents and families (via seminars, workshops, including from invited overseas experts) Functional vision assessment (incorporating Children’s University Hospital vision assessment clinics)
* (due to demand this is currently running at the rate of 1 infant and 1 school- age assessment per week)
Childhood Visual Impairment and Blindness Summary of limited data on prevalence rates and on trends in aetiology
There is a dearth of research into prevalence of childhood visual impairment and blindness (henceforth “VI”) not just in Ireland, where there is none since a report in 1991 (Goggin and O’Keefe, 1991), but globally, both in relation to VI in developing and the developed countries (Rahi and Dezateux, 1998). This document doesn’t attempt to report fully on such prevalence indicators as are known, as time and resources have not allowed this. However, it summarises some relevant data, for purposes of informing the Access Criteria working group of the National Co- Ordinating Group on Progressing Children’s Disability Services, to aid understanding of the importance of, and the specialist nature of, the healthcare and education needs of this subgroup of disabled children.
VI, as a category of disability, relates, the writer suggests, to a double cohort of disabled children – that is, VI and MDVI. ‘MDVI’ refer to a specific category of individuals who have a visual impairment or are blind, and have a second disability,
33 Draft 16.11.12
or more than one other disability, one of which is usually intellectual disability, often in the severe range. Child Vision uses the criteria of VI and two other disabilities – there is some disagreement internationally on the specific criteria (MDVI Euronet) but MDVI is a term increasingly widely used in Britain, Europe and North America. Often, MDVI incorporates vision impairment related to neurological abnormalities due to damage to the visual cortex.
Data on childhood VI rates (hereafter to be understood as applying herein to developed countries only) is both limited and, where it exists, is unlikely to reflect the true occurrence rates, due partly to under-registration of childhood VI with statutory registration schemes (for example, Flanagan, Jackson and Hill, 2003). Studies typically examine a limited geographical educational or healthcare area and extrapolate therefrom.
Data suggests that upto two per cent of the childhood population is visually impaired (Rahi and Dezateux, 1998). It also suggests that, in the past thirty years or so, the nature of the main conditions of VI in the childhood population has changed.
In Western Europe, the main causes of childhood VI are lesions of the central nervous system, congenital anomalies and retinal disorders (Kocur and Resnikoff, 2002). In North America, the leading causes of childhood VI are cortical visual impairment, retinopathy of prematurity and optic nerve hypoplasia (Steinkuller et al., 1999). Research in Sweden in 1999 suggests that the two main diagnostic groups are neuro-opthalmological and retinal diseases (Blohme and Tornqvist, 1999). In Ireland, birth asphyxia and retinopathy of prematurity were the commonest causes of identified childhood VI in 1989/90 (Goggin and O’Keefe, 1991).
There is, as reported by Flanagan, Jackson and Hill (2003), researching in Northern Ireland, an evidenced decrease in numbers of cases of isolated VI with an increase in instances of VI with co-existing neurological disability, which findings support the research mentioned above.
Other Northern Ireland research describes a drop, in the last thirty years, in the occurrence rates of more historically typical causes of VI such as congenital glaucoma and cataracts (which would typically be ‘stand alone’ VI) and an increase in cases of non-treatable VI - especially albinism - and cortical visual impairment (McClelland et al., 2007). The primary cause for the increase in VI with neurological basis is argued to be advances in medical care and intervention both with pre-term infants and infants born with severe neurological impairment and/or other serious, often complicated, medical conditions (Edmond and Foroozan, 2006, McClelland et al., 2007).
Some evidence suggests that Cortical Visual Impairment (henceforth “CVI”) is now the most common form of childhood VI (Blohme and Tornqvist, 1999). CVI, which involves deficits in the functioning of the vision pathways in the brain, encompasses a range of visual functioning from having no light perception to normal visual acuity with cognitive visual dysfunction (Edmond and Foroozan, 2006). Cognitive visual
34 Draft 16.11.12
dysfunction means, essentially, that the brain doesn’t understand what it sees – which means that it doesn’t, to varying extents, ‘see’ the environment.
The prevalence of neurologically-based and other cortical/cerebral impairments of vision explains to some extent why a considerable percentage of children with an intellectual disability/developmental delay present with visual impairment, and hence fit the category of MDVI. There is a correlation between low IQ/developmental delay and visual impairment (Sandfeld Nielsen, Skov and Jensen, 2007). This Danish study on the prevalence and aetiologies of VI in children with developmental delay found VI in 10.5% of their study group and 22.4% in those with an IQ at or below 50.
Flanagan’s Northern Ireland study found that, of the 76 participant children, 21% had isolated VI, 32% were following a normal developmental pattern, 79% had other medical problems, 43% had a severe intellectual disability and 45% of the children had CVI. Interestingly, only 22% of the children were registered VI/blind (Flanagan et al., 2003).
Flanagan broadly supports Clunies-Ross’s (1997) findings that 34.5% of the estimated 19,000 VI children in England Scotland and Wales were registered as having a visual impairment and other special needs. Flanagan concludes that blind/vi registers have limited value for planning of services and the prevalence of multi-disability including visual impairment suggests a need for early and specialist assessment and intervention for these children to optimise visual potential in childhood. Children who are otherwise disabled and visually impaired are deserving of extensive educational/developmental specialist attention as the impact of impaired vision may be greater than in children without another disability (Rahi and Dezateux, 1998).
Writer’s Addendum: It is almost certain that many children in Ireland today who are diagnosed as DD/ID also have a deficit in visual functioning which is not recognised, leading to lack of optimisation of the child’s achievements and quality of life via appropriate interventions. Awareness of MDVI, and use of appropriate assessment, training and support, is important. More Irish research on prevalence rates and VI causes in the child population, including in particular the intellectually disabled child population, is urgently needed. ______References
Blohmé, J. and Tornqvist, K. (1997), Visual impairment in Swedish children. Acta Ophthalmologica Scandinavica, 75: 681–687.
35 Draft 16.11.12
Clunies-Ross, L. (1997), Where have all the children gone? An analysis of new statistical data on visual impairment amongst children in England, Scotland and Wales, British Journal of Visual Impairment, May 1997, Vol. 15, Issue 2: pp.48-53.
Edmond, J.C., and Foroozan, R. (2006) Cortical visual impairment in children, Current Opinion in Ophthalmology, Vol. 17, Issue 6, pp.509-512.
Flanagan, N.M., Jackson, A.J. and Hill, A.E. (2003), Visual Impairment in childhood: insights from a community-based survey, Child, Care Health and Development, 29, 6, 493-499.
Goggin, M. and O’Keefe, M. (1991), Childhood Blindness in the Republic of Ireland: A National Survey, British Journal of Opthalmology, Vol.75, pp.425-429.
Kocur, and Resnikoff, . (2002) Visual Impairment and Blindness in Europe and their prevention, British Journal of Opthalmology, 86:716-722
Malkowicz, D.E., Myers, G., Leisman, G. (2006) Rehabilitation of Cortical Visual Impairment in Children, Intern. J. Neuroscience, 116:1015-1033
McClelland, J., Saunders, K.J., Hill, N., Magee, A., Shannon. M. and Jackson, A.J. (2007) The changing visual profile of children attending a regional specialist school for the visually impaired in Northern Ireland, Opthal. Physiol. Opt. 2007, 27: 556- 60.
MDVI Euronet (2011), MDVI Euronet Conference – Dublin 2011, conference files held by this writer (conference attendee) but available at www.mdvi-conference.org
Rahi, J.S. and Dezateux, C., (1998), Epidemiology of visual impairment in Britain, Arch Dis Child, Vol. 78: 381-386, downloaded from adc.bmj.com on 12.4.2012
Sandfeld Nielsen, L., Skov, L. and Jensen, H. (2007), Visual dysfunctions and ocular disorders in children with developmental delay. Acta Ophthalmologica Scandinavica, 85: 149–156
Steinkuller, P.G., Du, L., Gilbert, C., Foster, A. Collins, M. and Coats, D.K., (1999). Childhood blindness. Journal of American Association for Paediatric Ophthalmology and Strabismus, Vol. 3, Issue 1, pp.26-32.
36 Draft 16.11.12
37