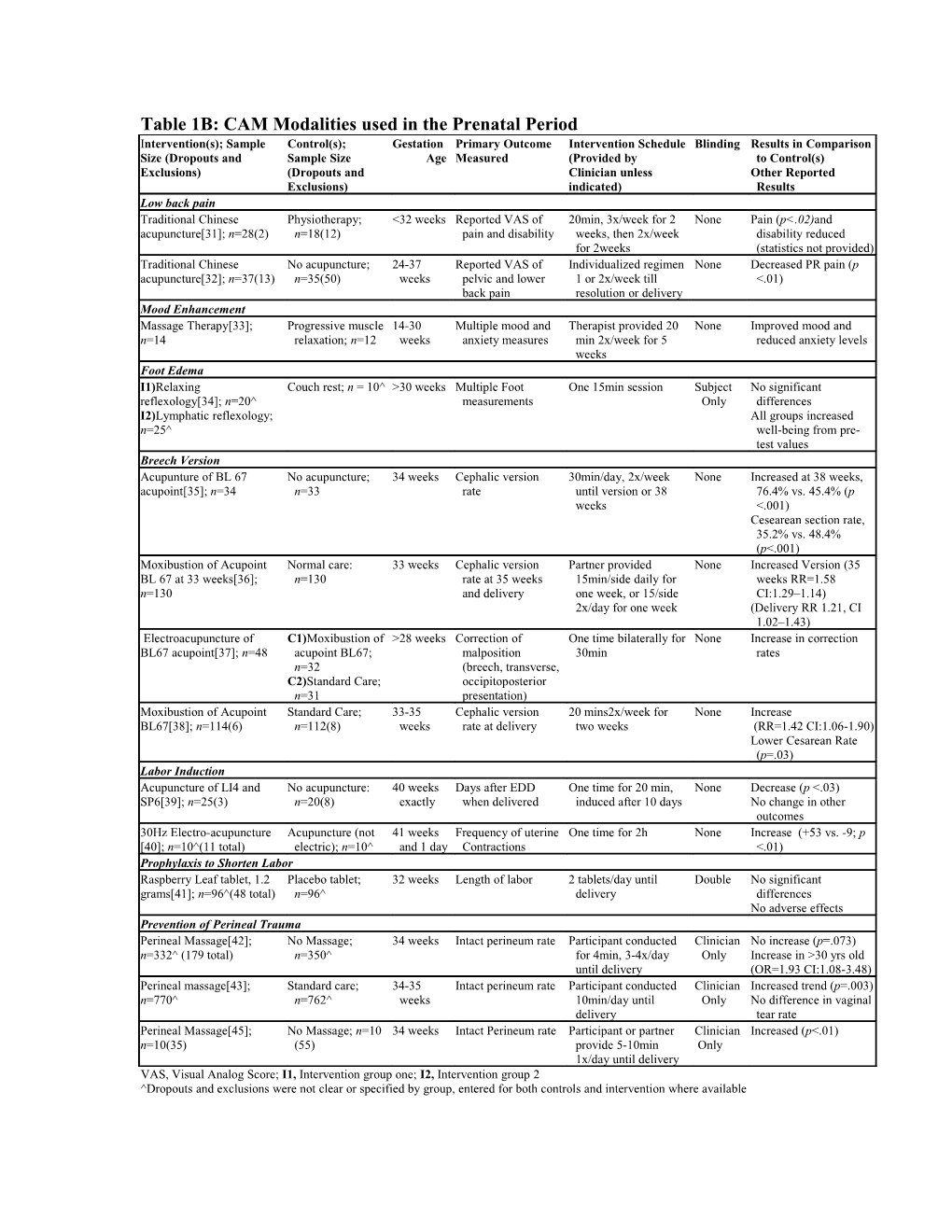
Table 1B: CAM Modalities used in the Prenatal Period Intervention(s); Sample Control(s); Gestation Primary Outcome Intervention Schedule Blinding Results in Comparison Size (Dropouts and Sample Size Age Measured (Provided by to Control(s) Exclusions) (Dropouts and Clinician unless Other Reported Exclusions) indicated) Results Low back pain Traditional Chinese Physiotherapy; <32 weeks Reported VAS of 20min, 3x/week for 2 None Pain (p<.02)and acupuncture[31]; n=28(2) n=18(12) pain and disability weeks, then 2x/week disability reduced for 2weeks (statistics not provided) Traditional Chinese No acupuncture; 24-37 Reported VAS of Individualized regimen None Decreased PR pain (p acupuncture[32]; n=37(13) n=35(50) weeks pelvic and lower 1 or 2x/week till <.01) back pain resolution or delivery Mood Enhancement Massage Therapy[33]; Progressive muscle 14-30 Multiple mood and Therapist provided 20 None Improved mood and n=14 relaxation; n=12 weeks anxiety measures min 2x/week for 5 reduced anxiety levels weeks Foot Edema I1)Relaxing Couch rest; n = 10^ >30 weeks Multiple Foot One 15min session Subject No significant reflexology[34]; n=20^ measurements Only differences I2)Lymphatic reflexology; All groups increased n=25^ well-being from pre- test values Breech Version Acupunture of BL 67 No acupuncture; 34 weeks Cephalic version 30min/day, 2x/week None Increased at 38 weeks, acupoint[35]; n=34 n=33 rate until version or 38 76.4% vs. 45.4% (p weeks <.001) Cesearean section rate, 35.2% vs. 48.4% (p<.001) Moxibustion of Acupoint Normal care: 33 weeks Cephalic version Partner provided None Increased Version (35 BL 67 at 33 weeks[36]; n=130 rate at 35 weeks 15min/side daily for weeks RR=1.58 n=130 and delivery one week, or 15/side CI:1.29–1.14) 2x/day for one week (Delivery RR 1.21, CI 1.02–1.43) Electroacupuncture of C1)Moxibustion of >28 weeks Correction of One time bilaterally for None Increase in correction BL67 acupoint[37]; n=48 acupoint BL67; malposition 30min rates n=32 (breech, transverse, C2)Standard Care; occipitoposterior n=31 presentation) Moxibustion of Acupoint Standard Care; 33-35 Cephalic version 20 mins2x/week for None Increase BL67[38]; n=114(6) n=112(8) weeks rate at delivery two weeks (RR=1.42 CI:1.06-1.90) Lower Cesarean Rate (p=.03) Labor Induction Acupuncture of LI4 and No acupuncture: 40 weeks Days after EDD One time for 20 min, None Decrease (p <.03) SP6[39]; n=25(3) n=20(8) exactly when delivered induced after 10 days No change in other outcomes 30Hz Electro-acupuncture Acupuncture (not 41 weeks Frequency of uterine One time for 2h None Increase (+53 vs. -9; p [40]; n=10^(11 total) electric); n=10^ and 1 day Contractions <.01) Prophylaxis to Shorten Labor Raspberry Leaf tablet, 1.2 Placebo tablet; 32 weeks Length of labor 2 tablets/day until Double No significant grams[41]; n=96^(48 total) n=96^ delivery differences No adverse effects Prevention of Perineal Trauma Perineal Massage[42]; No Massage; 34 weeks Intact perineum rate Participant conducted Clinician No increase (p=.073) n=332^ (179 total) n=350^ for 4min, 3-4x/day Only Increase in >30 yrs old until delivery (OR=1.93 CI:1.08-3.48) Perineal massage[43]; Standard care; 34-35 Intact perineum rate Participant conducted Clinician Increased trend (p=.003) n=770^ n=762^ weeks 10min/day until Only No difference in vaginal delivery tear rate Perineal Massage[45]; No Massage; n=10 34 weeks Intact Perineum rate Participant or partner Clinician Increased (p<.01) n=10(35) (55) provide 5-10min Only 1x/day until delivery VAS, Visual Analog Score; I1, Intervention group one; I2, Intervention group 2 ^Dropouts and exclusions were not clear or specified by group, entered for both controls and intervention where available
Table 1B: CAM Modalities Used in the Prenatal Period
Total Page:16
File Type:pdf, Size:1020Kb
Recommended publications