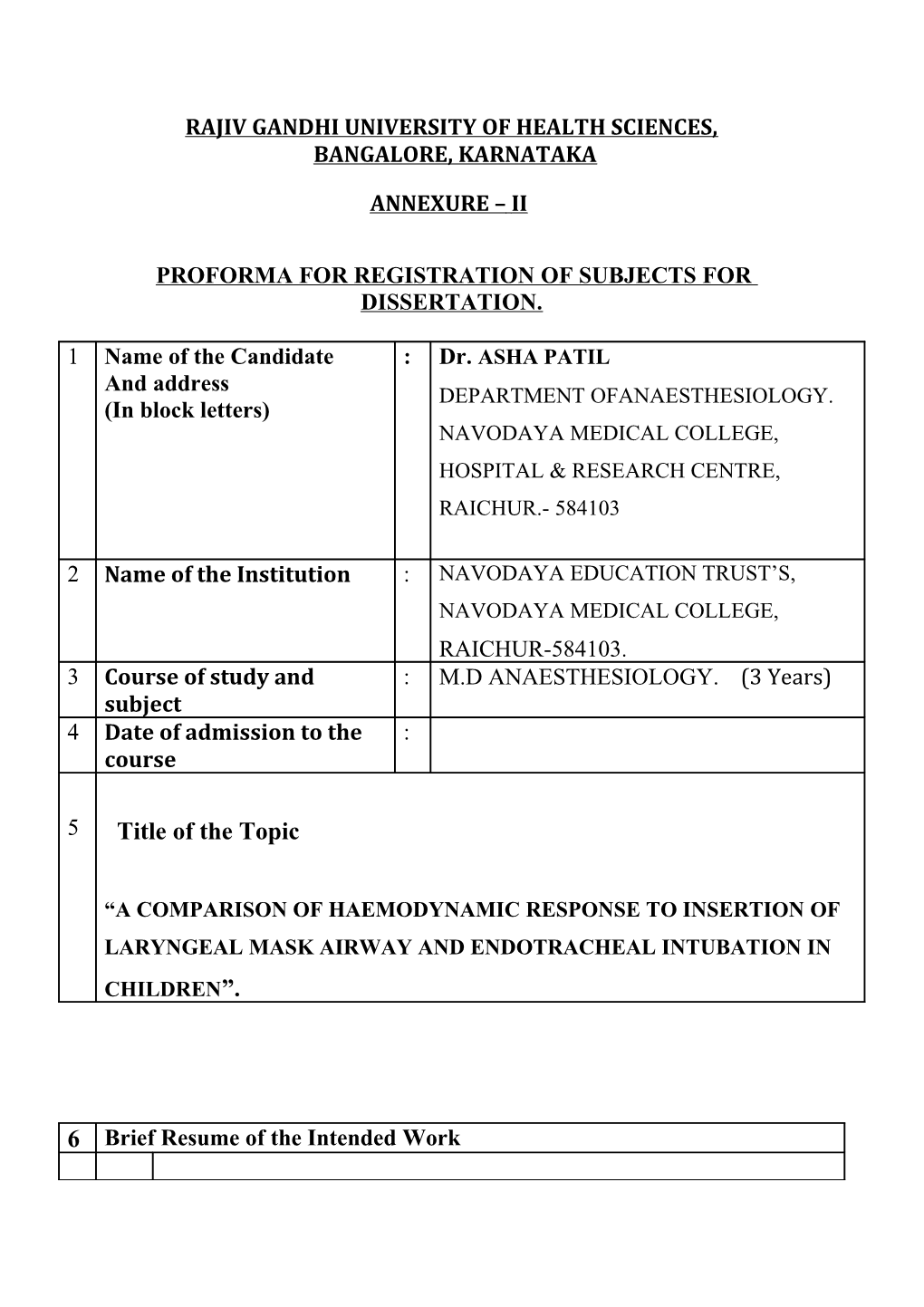
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE, KARNATAKA
ANNEXURE – II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION.
1 Name of the Candidate : Dr. ASHA PATIL And address DEPARTMENT OFANAESTHESIOLOGY. (In block letters) NAVODAYA MEDICAL COLLEGE, HOSPITAL & RESEARCH CENTRE, RAICHUR.- 584103
2 Name of the Institution : NAVODAYA EDUCATION TRUST’S, NAVODAYA MEDICAL COLLEGE, RAICHUR-584103. 3 Course of study and : M.D ANAESTHESIOLOGY. (3 Years) subject 4 Date of admission to the : course
5 Title of the Topic
“A COMPARISON OF HAEMODYNAMIC RESPONSE TO INSERTION OF LARYNGEAL MASK AIRWAY AND ENDOTRACHEAL INTUBATION IN CHILDREN”.
6 Brief Resume of the Intended Work 6.1 Need of the study :
Endotracheal intubation is the translaryngeal placement of endotracheal tube into the trachea via nose (nasotracheal intubation) or mouth (oro-tracheal intubation).Laryngeal mask airway insertion is an alternative method to endotracheal intubation for maintaining airway and anesthesia. In contrast to endotracheal intubation laryngeal mask airway insertion does not require instrumentation i.e.1aryngoscopy of the upper airway. Moreover laryngeal mask airway does not pass through glottis but is placed over the glottis. Laryngoscopy and tracheal intubation or laryngeal mask airway insertion are noxious stimuli which provoke a transient but marked sympathetic response manifesting as hypertension and tachycardia. In susceptible patients particularly those with systemic hypertension, coronary heart disease, cerebrovascular disease and intracranial aneurysm even these transient changes can result potentially deleterious effects eg: left ventricular failure, arrhythmias, myocardial ischaemia, cerebral haemorrhage and rupture of cerebral aneurysm.There are many numbers of ways to blunt these haemodynamic changes. They include minimizing the duration of laryngoscopy to less than 15 seconds, the use of intravenous narcotics, the use of intravenous lidocaine, vasodilators and beta -blocking agents. Laryngeal mask airway insertion involves lesser mechanical manipulation of upper airway than endotracheal intubation. This study aims to compare the haemodynamic response to endotracheal intubation and laryngeal mask airway insertion in children.
6.2 Review of Literature: The development of laryngeal mask airway began in 1981 at Royal London Hospital, White Chapel, London. A British anaesthesiologist Dr. Archie Brain1 began his work with the assumption that artificial airways in common use had a number of significant limitations. The face mask connects with the anatomic airway only at the mouth and nares. The tracheal tube requires visualization of the larynx for insertion and lateral pressure applied to the tracheal epithelial structures may provoke undesirable autonomic responses and impairs effective coughing. Hence Brain conceived the idea of developing an artificial tube which delivers anaesthetic gases and oxygen directly over the glottic aperture to be delivered to tracheo-bronchial tree. Shahin N Jamil et al conducted a study of use laryngeal mask airway insertion in children and compared it with endotracheal intubation found that laryngeal mask airway is suitable for positive pressure ventilation and has less haemodynamic response when compared to endotracheal intubation3.
Wilson IG et al found that insertion of the laryngeal mask airway has smaller cardiovascular responses than those after laryngoscopy and endotracheal intubation and it is useful in those patients who has marked pressor response4.
Braude N et al studied the pressor response of laryngeal mask insertion. They concluded that there were significant differences in haemodynamic changes between laryngeal mask group and endotracheal tube group5. Alan R et al found that laryngeal mask airway can be used as an alternative in children with uncomlpicated upper respiratory tract infections since it has reduced chances of bronchospasm,oxygen desaturation and coughing when compared to endotracheal inubation6. Al-Mazrou et al studied that laryngeal mask airway is suitable for children undergoing nasal surgery because it offers airway protection from blood contamination when compared with uncufffed endotracheal tube with throat pack7. Chen L, Hsiao AL found that in peadiatric arrest laryngeal mask airway has more rapid and effective ventilation8. Jonathan L.Benumof reported that clinical record of laryngeal mask airway use in "cannot ventilate, cannot intubate" situation has been excellent and in patients whose lungs cannot be ventilated because of the supraglottic obstruction and whose trachea cannot be intubated due to unfavorable anatomy, the laryngeal mask should be immediately available and considered as the first treatment of choice10. Shailendra Joshi, Robert R.Sciacca, Daneshvari. R et al conducted a study for evaluation of clinical tests for placement of laryngeal mask airway. They have concluded that of all nine tests, ability to generate an airway pressure of 20 cm H2O and ability to ventilate manually are the most specific tests11.
6.3 Objectives of the study: 1.The main objective of the study is designed to compare the haemodynamic responses to insertion of Laryngeal mask airway-classic and endotracheal intubation in children.
7 Materials and Methods:
7.1 Source of Data:
After obtaining institutional ethical clearance and written informed consent from the patients,6o patients of ASA I and ASA II grade children aged 2 -12 years undergoing elective surgery from department of surgery, Navodaya Medical College,Hospital and Research Center, Raichur,are included in the study.
7.2 Methods of collection of Data :
Design of study: Prospective study Duration of study -2 years. Patients are selected randomly allocated into 2 groups. Group L(n = 30) Laryngeal mask airway-classic group. Group E(n=30) Endotracheal tube intubation group.
All patients were randomly allocated to E (ETT group) laryngoscopy and endotracheal intubation with appropriate sized uncuffed endotracheal tube , while in Group L (LMA group) LMA-classic was inserted. All patients were premedicated with glycopyrolate 0.004mg/kg, metoclopramide 0.1mg/kg , midazolam 0.03mg/kg iv, tramadol 1mg/kg. Induction of anaesthesia was done with propofol 2mg/kg and relaxation by inj succinylcholine 1.5mg/kg iv and unresponsive to pain followed by vecuronium bromide 0.1 mg.kg iv to facilitate insertion of endotracheal tube/LMA. Haemodynamic changes were recorded before induction (baseline), just after intubation (0 min), then one of the two groups of 60 patients each, applying at 1, 3 and 5 min after intubation. At the end of surgery the residual neuromuscular blockade was reversed with neostigmine 0.05mg/kg iv and glycopyrolate 0.008 mg/kg iv.
INCLUSION CRITERIA 1. Children weighing 10-30 kgs. 2. ASA grade I and II. 3. Both sexes of age between 2 – 12 yrs of age. 4. Elective surgeries.
EXCLUSION CRITERIA
1. ASA grade III and IV.
2. History of respiratory diseases.
3. Pharyngeal pathology.
7.3 Does the study require any investigation or intervention to be conducted on patients or other humans or animals? If so, please describe briefly. 1. Estimation of Haemoglobin %.
2. Total blood cell count and Differential white blood count.
3. Blood grouping and cross matching.
4. Bleeding time and clotting time.
5. Urine analysis for sugar, albumin and microscopy.
6. HIV test and HBsAG Test. 7.Chest x-ray.
7.4 Has ethical clearance been obtained from your institution in case of 7.3?
The protocol of the study was revived and approved by the institutional Ethical Committee of Navodaya Medical College and Research center , Raichur.
8 List of references :
1. Archie Brain 1990 “Proper technique for insertion of the laryngeal mask” Anesthesiology, 73 : 1053.
2 Brain AIJ, Verghese C, Addy EV et al 1997 “The intubating laryngeal mask;Development of new device for intubation of trachea.” Br J Anaesth; 79 : 699- 703.
3. Shahin N Jamil et al 2009 “ A study of the use of laryngeal mask airway in children and its comparison with endotracheal intubation”.Indian journal of anaesthesia 53(2):174-178.
4. Wilson IG et al 1992 “Cardiovascular responses to insertion
of the laryngeal mask”. Anaesthesia, Apr;47(4):300-2.
5. Braude N, Clements EAF, Hodges UM et al 1989 “ The pressor response and laryngeal mask insertion: A comparison with tracheal intubation”. Anaesthesia; 44 :551 - 554.
6. Alan R et al 1998 “Use of the laryngeal Mask Airway in Children with Upper Respiratory Tract Infections: A Comparison
with Endotracheal Intubation”. Anesth Analg 1998;86:706-11.
7. Al-Mazrou et al 2010 “Laryngeal mask airway vs. uncuffed endotracheal tube for nasal and paranasal sinus
surgery: paediatric airway protection”. EJA:January - Volume 27 - Issue 1 - p 16-19.
8. Chen L, Hsiao AL 2008 “Randomized trial of endotracheal tube versus laryngeal mask airway in simulated prehospital pediatric arrest”. Pediatrics. Aug;122(2):e294-7. Epub 2008 Jul 21.
9. Benumof JL 1996 “Laryngeal mask airway and ASA difficult airway algorithm”.Anesthesiology; 84 : 686 - 99.
10.Shailendra Joshi, Robert R. Sciacca, Daneshvari R et al 1998 “A prospective evaluation of clinical tests for placement of laryngeal mask airways”. Anesthesiology;1141-6. 9. Signature of the Candidate
10. Remarks of the Guide Recommended and forwarded 11. 11.1 Name and Designation of Dr.ARVIND SHURPALI.M.D. Guide (In block letters) ASSOCIATE PROFFESOR. DEPT OF ANAESTHESIOLOGY AND CRITICAL CARE NAVODAYA MEDICAL COLLEGE AND RESEARCH CENTER RAICHUR. 11.2 Signature
11.3 Co-guide (if any) Dr.D.S.RAMCHANDRA. M.D. PROFESSOR & HEAD DEPT OF ANAESTHESIOLOGY, DR.AMIT.J.P,ASSITANT PROFESSOR. 11.4 Signature
11.5 Head of the Department Dr.D.S.RAMCHANDRA. M.D. PROFESSOR & HEAD DEPT OF ANAESTHESIOLOGY NAVODAYA MEDICAL COLLEGE & RESEARCH CENTER, RAICHUR.- 584103 11.6 Signature 12 12.1 Remarks of Chairman and Principal
12.2 Signature